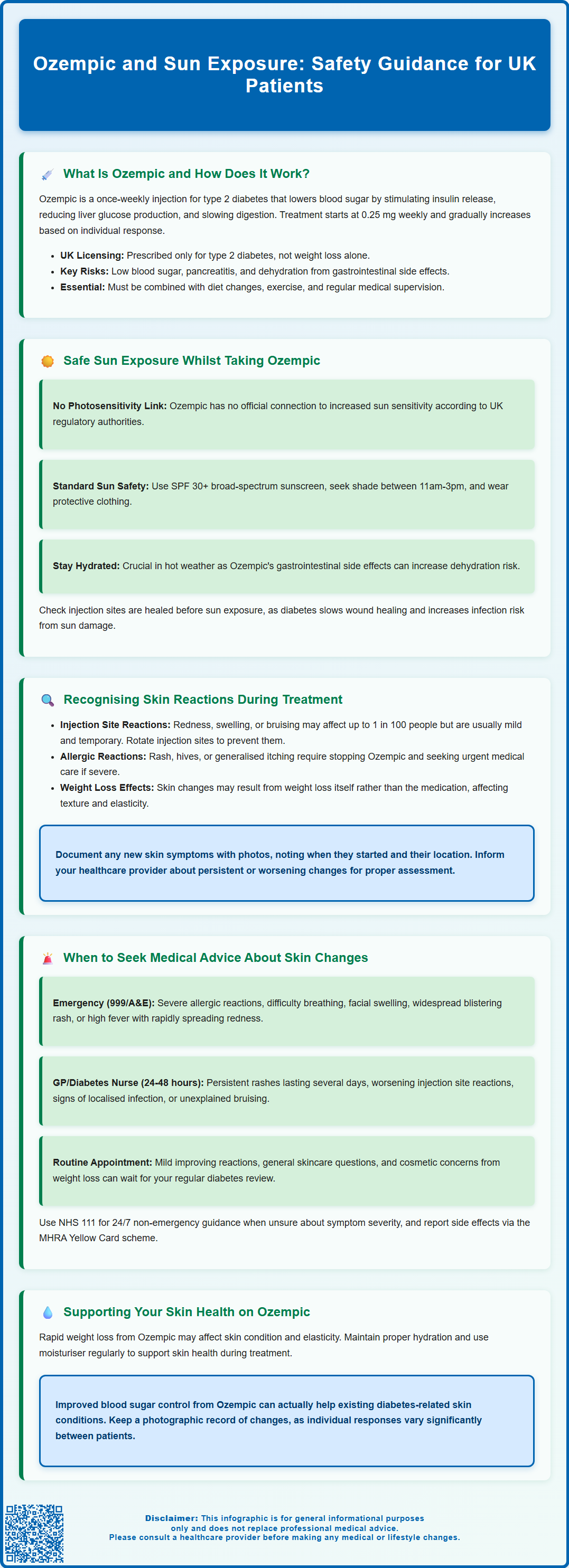
Ozempic (semaglutide) is a glucagon-like peptide-1 (GLP-1) receptor agonist licensed in the UK for treating type 2 diabetes mellitus in adults. Administered as a once-weekly subcutaneous injection, it helps regulate blood glucose by stimulating insulin secretion, suppressing glucagon release, and slowing gastric emptying. Whilst Ozempic is generally well-tolerated, patients often have questions about sun exposure and potential skin reactions during treatment. Currently, no official link exists between Ozempic and increased photosensitivity, though individuals with diabetes should maintain good sun safety practices as part of overall health management. Understanding how to protect your skin and recognise concerning reactions ensures safe, effective treatment.
Summary: There is no established link between Ozempic (semaglutide) and increased photosensitivity or heightened risk from sun exposure according to UK regulatory guidance.
- Ozempic is a GLP-1 receptor agonist licensed for type 2 diabetes, administered as a once-weekly subcutaneous injection.
- Photosensitivity is not listed among known adverse effects in the MHRA-approved Summary of Product Characteristics.
- Standard sun protection measures remain important for people with diabetes, including SPF 30+ sunscreen and seeking shade during peak UV hours.
- Gastrointestinal side effects may increase dehydration risk in hot weather, requiring careful fluid management.
- Injection site reactions (redness, swelling, bruising) are uncommon and typically mild, affecting up to 1 in 100 people.
- Seek urgent medical care for severe allergic reactions, widespread rash with blistering, or signs of serious infection.
Table of Contents
What Is Ozempic and How Does It Work?
Ozempic (semaglutide) is a prescription medicine licensed in the UK for the treatment of type 2 diabetes mellitus in adults. It belongs to a class of medications called glucagon-like peptide-1 (GLP-1) receptor agonists, which work by mimicking the action of a naturally occurring hormone that regulates blood sugar levels.
The mechanism of action involves several key processes:
-
Stimulating insulin secretion from the pancreas when blood glucose levels are elevated
-
Suppressing glucagon release, which reduces glucose production by the liver
-
Slowing gastric emptying, helping to moderate post-meal blood sugar spikes
-
Reducing appetite through effects on brain centres that regulate hunger
Ozempic is administered as a once-weekly subcutaneous injection, typically into the abdomen, thigh, or upper arm. The medication is available in pre-filled pens containing doses of 0.25 mg, 0.5 mg, 1 mg, or 2 mg. Treatment usually begins with a lower dose (0.25 mg weekly for four weeks) to minimise gastrointestinal side effects rather than for glycaemic control, with gradual increases to 0.5 mg and potentially 1 mg or 2 mg based on individual response and tolerability.
According to NICE guidance (TA585 and NG28), GLP-1 receptor agonists like Ozempic may be considered for adults with type 2 diabetes when other treatments have not achieved adequate glycaemic control, and when weight loss would provide significant clinical benefit (with BMI thresholds adjusted for ethnicity). The medication has demonstrated effectiveness in reducing HbA1c levels and can support weight management, though it is not licensed for weight loss (unlike Wegovy, which contains the same active ingredient at a higher dose). Ozempic must be used alongside dietary modifications and increased physical activity.
Important safety considerations include:
-
Increased risk of hypoglycaemia when used with insulin or sulfonylureas
-
Potential risk of pancreatitis (stop treatment and seek urgent care if suspected)
-
Possible early worsening of diabetic retinopathy with rapid improvement in blood glucose control
-
Risk of dehydration due to gastrointestinal side effects, particularly in hot weather
Ozempic is not licensed for type 1 diabetes or diabetic ketoacidosis, and should only be used under appropriate medical supervision with regular monitoring of blood glucose levels and overall metabolic control.
Safe Sun Exposure While Taking Ozempic
Currently, there is no official link established between Ozempic (semaglutide) and increased photosensitivity or heightened risk from sun exposure in the product's Summary of Product Characteristics (SmPC) approved by the MHRA (Medicines and Healthcare products Regulatory Agency). Photosensitivity is not listed among the known adverse effects of semaglutide, and the medication does not contain ingredients typically associated with sun-related skin reactions.
However, individuals with diabetes—regardless of medication—should maintain good sun safety practices as part of overall health management. People with diabetes may experience slower wound healing and are at increased risk of skin infections, making sun protection particularly important to prevent sunburn and subsequent skin damage.
Recommended sun safety measures include:
-
Applying broad-spectrum sunscreen with SPF 30 or higher and at least 4-star UVA protection to exposed skin, reapplying every two hours and after swimming or sweating
-
Seeking shade during peak UV hours (11am to 3pm in the UK)
-
Wearing protective clothing, including wide-brimmed hats and UV-protective sunglasses
-
Staying well-hydrated, especially important for diabetes management
-
Checking injection sites before sun exposure to ensure they are healed and not inflamed
It's particularly important to maintain adequate hydration in hot weather when taking Ozempic, as the gastrointestinal side effects (nausea, vomiting, diarrhoea) can increase the risk of dehydration and potentially acute kidney injury. If you're unable to keep fluids down due to these side effects during hot weather, seek medical advice promptly and follow diabetes sick-day rules.
It's worth noting that rapid weight loss—which some people experience whilst taking Ozempic—can occasionally affect skin condition and elasticity. Maintaining adequate hydration and using moisturiser regularly can help support skin health. If you notice any unusual skin changes or reactions following sun exposure whilst taking Ozempic, it's advisable to discuss these with your GP or diabetes specialist nurse, even though a direct causal relationship has not been established. Individual responses to medications can vary, and your healthcare team can provide personalised advice based on your specific circumstances and medical history.
Recognising Skin Reactions During Ozempic Treatment
Whilst Ozempic is generally well-tolerated, it's important to be aware of potential skin-related adverse effects that may occur during treatment, though these are typically unrelated to sun exposure. According to the medication's SmPC, injection site reactions are among the reported skin-related issues, though they are generally uncommon (may affect up to 1 in 100 people).
Injection site reactions may include:
-
Redness, swelling, or bruising at the injection site
-
Itching or mild discomfort
-
Localised injection-site nodules or lumps
These reactions are usually mild and transient, resolving within a few days without specific treatment. Rotating injection sites with each dose helps minimise these effects and ensures optimal medication absorption.
Other skin reactions that have been reported include:
-
Allergic skin reactions such as rash or urticaria (hives)
-
Pruritus (generalised itching)
-
Rare cases of angioedema (swelling of deeper skin layers)
If you develop signs of a severe allergic reaction, angioedema, or a severe skin rash, stop taking Ozempic and seek urgent medical attention.
It's important to distinguish between expected injection site reactions and more concerning symptoms. Normal injection site reactions typically remain localised, are mild in intensity, and improve over time. In contrast, concerning signs include spreading redness, increasing warmth, severe pain, discharge from the injection site, or systemic symptoms such as fever, which could indicate infection.
Some individuals taking Ozempic may notice skin changes related to weight loss rather than the medication itself. Rapid weight reduction can affect skin texture, elasticity, and appearance. Additionally, improved glycaemic control may positively influence pre-existing diabetes-related skin conditions such as acanthosis nigricans (darkened skin patches) or diabetic dermopathy.
If you develop any new or unusual skin symptoms whilst taking Ozempic—whether or not they appear related to sun exposure—it's advisable to document when they began, their location, and any associated factors. Photographs can be helpful for monitoring progression. Keep your healthcare team informed of any persistent or worsening skin changes, as they can assess whether these require investigation or modification of your treatment plan.
When to Seek Medical Advice About Skin Changes
Understanding when skin changes require professional medical assessment is crucial for anyone taking Ozempic. Whilst most skin reactions are benign and self-limiting, certain symptoms warrant prompt medical attention.
Seek urgent medical care (call 999 or attend A&E) if you experience:
-
Signs of a severe allergic reaction (anaphylaxis): difficulty breathing, swelling of the face, lips, tongue or throat, severe dizziness, or rapid pulse
-
Widespread severe rash with blistering or peeling skin
-
Signs of serious infection: high fever, severe pain, rapidly spreading redness with warmth, or red streaks extending from an injection site
Stop taking Ozempic immediately if you experience any of these severe reactions.
Contact your GP or diabetes specialist nurse within 24-48 hours if you notice:
-
Persistent rash or hives lasting more than a few days
-
Injection site reactions that worsen rather than improve, or don't resolve within a week
-
Signs of localised infection: increasing redness, warmth, swelling, or pus at injection sites
-
New skin lesions, particularly if they're painful, bleeding, or changing rapidly
-
Unexplained bruising or skin discolouration
-
Any skin changes accompanied by other symptoms such as joint pain, fever, or general malaise
-
Persistent vomiting or diarrhoea, especially in hot weather, which could lead to dehydration
Routine discussion at your next scheduled appointment is appropriate for:
-
Mild, stable injection site reactions that are improving
-
Questions about sun protection or general skin care whilst taking Ozempic
-
Cosmetic concerns related to weight loss
-
Gradual improvement in pre-existing diabetes-related skin conditions
Your diabetes care team should conduct regular medication reviews, typically every 3-6 months, which provide an opportunity to discuss any skin-related concerns. Between appointments, maintain a record of any skin changes, including photographs if possible, to facilitate accurate assessment.
Remember that individual responses to medications vary, and what might be normal for one person could indicate a problem for another. When in doubt, it's always better to seek advice rather than wait. The NHS 111 service is available 24/7 for non-emergency guidance if you're uncertain whether your symptoms require immediate attention. Your pharmacist can also provide valuable advice about managing minor injection site reactions and appropriate skincare products to use alongside your diabetes medication.
If you suspect you've experienced a side effect from Ozempic, you can report it directly to the MHRA Yellow Card scheme (yellowcard.mhra.gov.uk or via the Yellow Card app). This helps authorities monitor the safety of medicines.
Frequently Asked Questions
Does Ozempic make your skin more sensitive to sunlight?
No, there is no official link between Ozempic and increased photosensitivity according to MHRA guidance. Photosensitivity is not listed as a known side effect, though standard sun protection remains important for people with diabetes.
What sun protection should I use whilst taking Ozempic?
Apply broad-spectrum sunscreen with SPF 30 or higher and at least 4-star UVA protection, reapplying every two hours. Seek shade during peak UV hours (11am-3pm), wear protective clothing, and maintain adequate hydration, especially important given Ozempic's gastrointestinal effects.
When should I seek medical advice about skin changes on Ozempic?
Seek urgent care (999 or A&E) for severe allergic reactions, difficulty breathing, widespread severe rash, or signs of serious infection. Contact your GP within 24-48 hours for persistent rash, worsening injection site reactions, or unexplained skin changes accompanied by other symptoms.
The health-related content published on this site is based on credible scientific sources and is periodically reviewed to ensure accuracy and relevance. Although we aim to reflect the most current medical knowledge, the material is meant for general education and awareness only.
The information on this site is not a substitute for professional medical advice. For any health concerns, please speak with a qualified medical professional. By using this information, you acknowledge responsibility for any decisions made and understand we are not liable for any consequences that may result.
Heading 1
Heading 2
Heading 3
Heading 4
Heading 5
Heading 6
Lorem ipsum dolor sit amet, consectetur adipiscing elit, sed do eiusmod tempor incididunt ut labore et dolore magna aliqua. Ut enim ad minim veniam, quis nostrud exercitation ullamco laboris nisi ut aliquip ex ea commodo consequat. Duis aute irure dolor in reprehenderit in voluptate velit esse cillum dolore eu fugiat nulla pariatur.
Block quote
Ordered list
- Item 1
- Item 2
- Item 3
Unordered list
- Item A
- Item B
- Item C
Bold text
Emphasis
Superscript
Subscript












