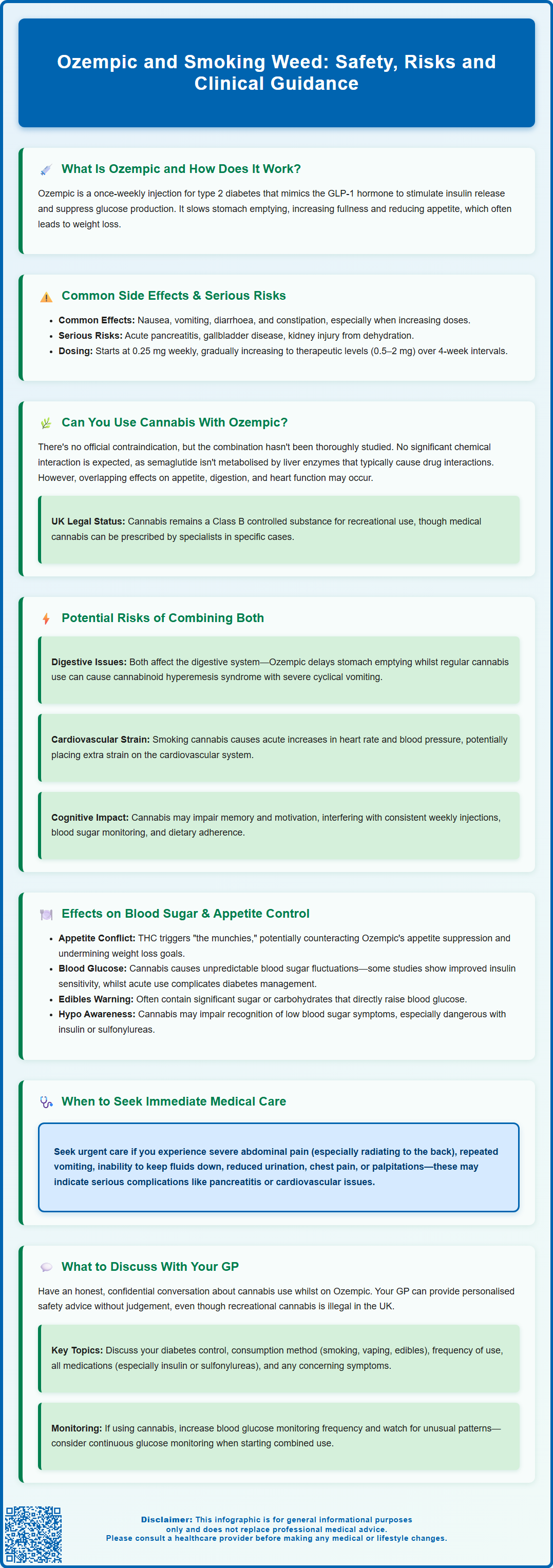
Many people prescribed Ozempic for type 2 diabetes wonder whether it is safe to use cannabis alongside their medication. Whilst there is no formal contraindication listed in UK prescribing guidance, the combination raises important clinical considerations. Ozempic (semaglutide) is a GLP-1 receptor agonist that regulates blood glucose and suppresses appetite, whilst cannabis affects multiple body systems including metabolism, gastrointestinal function, and cardiovascular health. Understanding potential interactions, risks, and the importance of open communication with your GP is essential for safe diabetes management. This article explores the evidence, practical concerns, and harm-reduction strategies for patients considering or currently using cannabis whilst taking Ozempic.
Summary: There is no formal contraindication to using cannabis whilst taking Ozempic, but the combination may affect appetite control, gastrointestinal symptoms, blood glucose regulation, and diabetes self-management.
- Ozempic (semaglutide) is a GLP-1 receptor agonist used for type 2 diabetes management, administered as a once-weekly subcutaneous injection.
- Cannabis may counteract Ozempic's appetite-suppressing effects and cause unpredictable fluctuations in blood glucose levels.
- Both substances can affect the gastrointestinal system; combined use may exacerbate nausea or complicate symptom recognition.
- Smoking cannabis poses respiratory and cardiovascular risks, which may compound existing health vulnerabilities in people with diabetes.
- Patients should discuss cannabis use openly with their GP to ensure safe medication management and appropriate monitoring of diabetes control.
Table of Contents
What Is Ozempic and How Does It Work?
Ozempic (semaglutide) is a prescription medication licensed in the UK for the treatment of type 2 diabetes mellitus. It belongs to a class of drugs known as glucagon-like peptide-1 (GLP-1) receptor agonists. Ozempic is administered as a once-weekly subcutaneous injection and works by mimicking the action of the naturally occurring hormone GLP-1, which plays a crucial role in glucose regulation and appetite control.
The mechanism of action involves several physiological processes. Ozempic stimulates insulin secretion from pancreatic beta cells in a glucose-dependent manner, meaning it only promotes insulin release when blood glucose levels are elevated. This reduces the risk of hypoglycaemia compared to some other diabetes medications, though this risk increases if used alongside insulin or sulfonylureas. Additionally, it suppresses glucagon secretion, a hormone that raises blood sugar levels, thereby preventing excessive glucose production by the liver.
Beyond glycaemic control, Ozempic slows gastric emptying, which means food remains in the stomach longer, leading to increased satiety and reduced appetite. This effect has contributed to its notable impact on weight loss, though in the UK it is primarily licensed for diabetes management rather than obesity treatment alone (though a higher-dose formulation, Wegovy, is available specifically for weight management).
Patients prescribed Ozempic typically start on a lower dose (0.25 mg weekly) which is gradually increased to therapeutic levels (0.5 mg, 1 mg, or 2 mg weekly) at 4-week intervals based on glycaemic response and tolerability. Common adverse effects include nausea, vomiting, diarrhoea, and constipation, particularly during dose escalation. Important safety considerations include the risk of acute pancreatitis (seek urgent medical advice for severe, persistent abdominal pain), gallbladder disease, dehydration leading to acute kidney injury from gastrointestinal effects, and potential worsening of diabetic retinopathy with rapid improvement in blood glucose control.
NICE recommends Ozempic as an option for type 2 diabetes management, and the SmPC states it should be used as part of a comprehensive diabetes management plan that includes dietary modification and physical activity.
Can You Smoke Cannabis While Taking Ozempic?
There is no official contraindication listed in the Ozempic Summary of Product Characteristics (SmPC) that specifically prohibits the concurrent use of cannabis whilst taking semaglutide. However, this does not mean the combination is without potential concerns or that it has been thoroughly studied in clinical trials. The lack of formal guidance reflects the limited research into interactions between prescription diabetes medications and recreational cannabis use.
From a pharmacological perspective, no significant drug-drug interaction is expected via liver enzyme pathways, as semaglutide is not metabolised by the cytochrome P450 enzyme system. The main concerns with combined use are related to overlapping effects on appetite, gastrointestinal function, and cardiovascular system, as well as potential impacts on medication adherence and diabetes self-management.
Cannabis remains a controlled substance under the Misuse of Drugs Act 1971 in the UK, classified as a Class B drug. Whilst medical cannabis can be prescribed in specific circumstances by specialist clinicians, recreational use is illegal. Nevertheless, healthcare professionals can still provide confidential harm-reduction advice and safety planning for patients who choose to use cannabis.
From a clinical perspective, the decision to use cannabis whilst taking Ozempic involves individual risk assessment. Factors to consider include the method of consumption (smoking, vaping, edibles), frequency of use, the presence of other medical conditions, and concurrent medications. Cannabis affects multiple body systems, including metabolic and cardiovascular function, which may interact with the effects of Ozempic.
Patients should be aware that smoking any substance carries inherent respiratory risks, including chronic bronchitis and impaired lung function. For individuals with diabetes, who already face increased cardiovascular risk, adding smoking-related harm may compound existing health vulnerabilities. If you are currently using cannabis and have been prescribed Ozempic, it is essential to have an open, non-judgemental conversation with your GP or diabetes specialist nurse to discuss potential risks and ensure safe medication management.
Potential Risks of Combining Ozempic and Cannabis
Whilst direct drug-drug interactions between semaglutide and cannabis have not been extensively documented in clinical literature, several theoretical and practical concerns warrant consideration. Understanding these potential risks can help patients make informed decisions and recognise warning signs that require medical attention.
Gastrointestinal effects represent a primary concern. Both Ozempic and cannabis can affect the digestive system, though in different ways. Ozempic commonly causes nausea, vomiting, and delayed gastric emptying. Cannabis, particularly when smoked regularly, has been associated with cannabinoid hyperemesis syndrome (CHS), a condition characterised by cyclical severe nausea and vomiting. The combination of Ozempic's gastrointestinal side effects with cannabis use could potentially exacerbate nausea or make it difficult to distinguish between medication side effects and cannabis-related symptoms.
Red flags requiring urgent medical attention include severe, persistent abdominal pain (which may radiate to the back), repeated vomiting, inability to keep fluids down, or reduced urine output. If you experience these symptoms, seek immediate medical care and inform healthcare providers about all medications and substances you are using. Semaglutide should be stopped if acute pancreatitis is suspected, as per the SmPC guidance.
Cardiovascular considerations are also relevant. Clinical trials (such as SUSTAIN-6) have shown cardiovascular benefits in people with type 2 diabetes taking semaglutide, though it does not have a specific UK indication for cardiovascular risk reduction. Cannabis use, particularly smoking, can cause acute increases in heart rate and blood pressure. For individuals with pre-existing cardiovascular disease or risk factors, this combination may pose additional strain on the cardiovascular system.
There are also concerns regarding medication adherence and diabetes self-management. Cannabis can impair cognitive function, motivation, and memory, potentially affecting a person's ability to consistently administer their weekly Ozempic injection, monitor blood glucose levels, or maintain dietary modifications essential for diabetes control. Additionally, the psychoactive effects of THC (tetrahydrocannabinol) may impair judgement regarding food choices or recognition of hypoglycaemic symptoms, which could compromise diabetes management.
Patients with pre-existing diabetic retinopathy should be aware that rapid improvement in blood glucose control with semaglutide may temporarily worsen retinopathy. Seek prompt ophthalmology review if you experience any visual changes.
Effects on Blood Sugar and Appetite Control
The interaction between cannabis and blood glucose regulation is complex and not fully understood. Research suggests that cannabis use may have variable effects on glucose metabolism, insulin sensitivity, and appetite—factors that are particularly relevant for individuals taking Ozempic for diabetes management.
Cannabis is well known for stimulating appetite, a phenomenon commonly referred to as "the munchies". This effect is primarily mediated by THC, which activates cannabinoid receptors in the brain's appetite-regulating centres. For someone taking Ozempic, which works partly by suppressing appetite and promoting satiety, cannabis-induced hunger could potentially counteract the medication's appetite-suppressing effects. This may lead to increased caloric intake, potentially undermining weight management goals and glycaemic control.
Regarding direct effects on blood glucose, the evidence is mixed and largely observational. Some studies have suggested that regular cannabis users may have lower fasting insulin levels and improved insulin sensitivity, whilst others have found no significant metabolic benefits. Acute cannabis use can cause fluctuations in blood sugar levels, though the direction and magnitude of these changes can vary considerably between individuals. For someone with diabetes taking Ozempic, these unpredictable effects could make blood glucose management more challenging.
It is important to note that edible cannabis products may contain significant amounts of sugar or carbohydrates, which can directly impact blood glucose levels. Patients must account for these carbohydrates in their diabetes management plan. Additionally, cannabis-related cognitive impairment might reduce awareness of hypoglycaemic symptoms (low blood sugar), such as tremor, sweating, or confusion, potentially delaying appropriate treatment. This risk is particularly important if you are also taking insulin or sulfonylureas alongside Ozempic, as these combinations increase hypoglycaemia risk and may require dose adjustments of those medications.
Monitoring blood glucose levels becomes even more important if using cannabis whilst taking Ozempic. Patients should maintain regular testing schedules and be alert to unusual patterns or unexplained fluctuations that might indicate problematic interactions. Consider using structured self-monitoring or continuous glucose monitoring if available, especially when first assessing the impact of combined use.
What to Discuss With Your GP Before Using Cannabis
Having an honest, confidential conversation with your GP or diabetes care team is essential if you are considering using cannabis or are already doing so whilst taking Ozempic. Healthcare professionals are bound by confidentiality and their primary concern is your safety and wellbeing, not judgement regarding lifestyle choices. They can provide harm-reduction advice even though recreational cannabis use is illegal in the UK.
Key topics to discuss include:
-
Your current diabetes control: Share your recent HbA1c results, blood glucose monitoring patterns, and any difficulties you're experiencing with diabetes management. Your GP can assess whether adding cannabis to your regimen might complicate glycaemic control.
-
Method and frequency of cannabis use: Different consumption methods (smoking, vaping, edibles) carry different risks. Smoking poses respiratory risks, whilst edibles may contain unpredictable amounts of THC and carbohydrates. Frequency of use also matters—occasional use presents different considerations than daily consumption.
-
Other medications and health conditions: Cannabis can interact with various medications beyond Ozempic. Your GP needs a complete picture of your medication regimen, including over-the-counter products and supplements. If you're also taking insulin or sulfonylureas, your risk of hypoglycaemia may increase, requiring a personalised monitoring plan. Pre-existing cardiovascular, respiratory, or mental health conditions may increase risks.
-
Symptoms or side effects: Report any unusual symptoms, particularly severe or persistent abdominal pain, cyclical vomiting, inability to keep fluids down, reduced urine output, visual changes, or cardiovascular symptoms such as palpitations or chest discomfort. These may require urgent assessment.
-
Alternative options: If you're using cannabis for symptom management (such as pain, anxiety, or nausea), discuss evidence-based alternatives. In rare cases, medical cannabis might be appropriate and can be prescribed legally in the UK by specialist clinicians for specific conditions.
Your GP can provide individualised advice based on your complete medical history and may recommend more frequent monitoring or adjustments to your diabetes management plan. If you experience severe or persistent side effects, contact your GP promptly or call NHS 111 for advice. In emergencies, such as severe chest pain, difficulty breathing, or altered consciousness, call 999 immediately.
If you suspect you are experiencing side effects from Ozempic, these can be reported through the MHRA Yellow Card Scheme, which helps monitor the safety of medicines in the UK.
Frequently Asked Questions
Can I use cannabis whilst taking Ozempic for diabetes?
There is no formal contraindication, but the combination may affect appetite control, blood glucose regulation, and gastrointestinal symptoms. Discuss your individual circumstances with your GP to assess potential risks and ensure safe diabetes management.
Does cannabis interfere with Ozempic's effectiveness?
Cannabis may counteract Ozempic's appetite-suppressing effects through THC-induced hunger, potentially undermining weight management and glycaemic control. Blood glucose monitoring becomes particularly important to identify any unusual patterns or fluctuations.
What symptoms require urgent medical attention when using both substances?
Seek immediate medical care for severe persistent abdominal pain, repeated vomiting, inability to keep fluids down, reduced urine output, visual changes, chest pain, or difficulty breathing. Inform healthcare providers about all medications and substances you are using.
The health-related content published on this site is based on credible scientific sources and is periodically reviewed to ensure accuracy and relevance. Although we aim to reflect the most current medical knowledge, the material is meant for general education and awareness only.
The information on this site is not a substitute for professional medical advice. For any health concerns, please speak with a qualified medical professional. By using this information, you acknowledge responsibility for any decisions made and understand we are not liable for any consequences that may result.
Heading 1
Heading 2
Heading 3
Heading 4
Heading 5
Heading 6
Lorem ipsum dolor sit amet, consectetur adipiscing elit, sed do eiusmod tempor incididunt ut labore et dolore magna aliqua. Ut enim ad minim veniam, quis nostrud exercitation ullamco laboris nisi ut aliquip ex ea commodo consequat. Duis aute irure dolor in reprehenderit in voluptate velit esse cillum dolore eu fugiat nulla pariatur.
Block quote
Ordered list
- Item 1
- Item 2
- Item 3
Unordered list
- Item A
- Item B
- Item C
Bold text
Emphasis
Superscript
Subscript