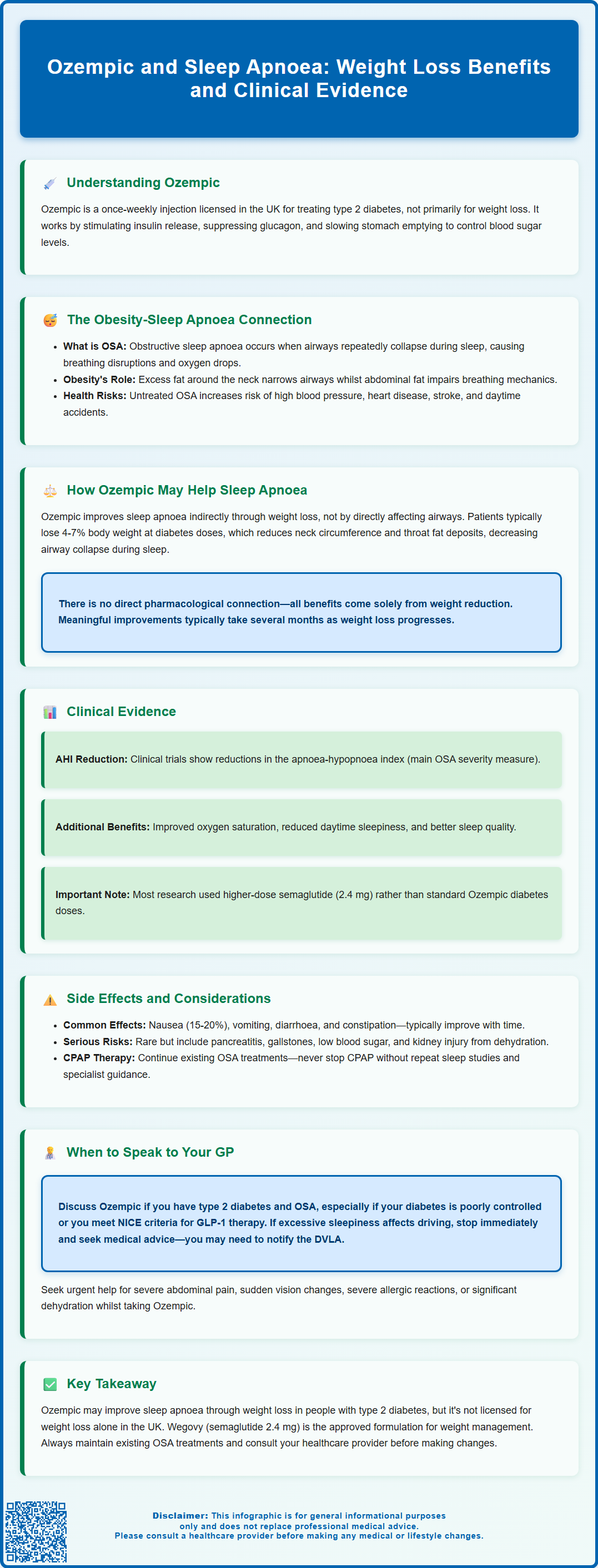
Ozempic (semaglutide) is a glucagon-like peptide-1 (GLP-1) receptor agonist licensed in the UK for treating type 2 diabetes mellitus. Whilst its primary role is glycaemic control, Ozempic has gained attention for its weight loss effects—a factor that may indirectly benefit individuals with obstructive sleep apnoea (OSA). Obesity is the most significant modifiable risk factor for OSA, and weight reduction can improve airway obstruction and sleep quality. This article explores the relationship between Ozempic and sleep apnoea, examining how weight loss may influence OSA outcomes, the clinical evidence supporting this link, and important considerations for patients and healthcare professionals in the UK.
Summary: Ozempic may improve obstructive sleep apnoea indirectly through weight loss, as reduced body weight decreases upper airway obstruction, though it has no direct pharmacological effect on sleep apnoea mechanisms.
- Ozempic (semaglutide) is a GLP-1 receptor agonist licensed in the UK for type 2 diabetes, not specifically for sleep apnoea or weight management.
- Weight loss from Ozempic reduces neck circumference and pharyngeal fat deposits, which can decrease upper airway collapsibility during sleep.
- Clinical trials show semaglutide 2.4 mg reduces apnoea-hypopnoea index (AHI) in patients with obesity and moderate to severe OSA, correlating with weight loss achieved.
- Common side effects include nausea, vomiting, diarrhoea, and constipation; serious risks include pancreatitis, gallbladder problems, and hypoglycaemia when combined with certain diabetes medications.
- Patients using CPAP therapy should continue treatment whilst taking Ozempic, as weight loss takes time and OSA management should not be interrupted without specialist guidance.
- NICE guidance recommends GLP-1 receptor agonists like Ozempic for type 2 diabetes when specific BMI and glycaemic control criteria are met.
Table of Contents
- Understanding Ozempic and Its Primary Uses
- The Link Between Obesity and Obstructive Sleep Apnoea
- How Ozempic May Affect Sleep Apnoea Through Weight Loss
- Clinical Evidence: Ozempic's Impact on Sleep Apnoea Outcomes
- Important Considerations and Potential Side Effects
- When to Speak to Your GP About Ozempic and Sleep Apnoea
- Frequently Asked Questions
Understanding Ozempic and Its Primary Uses
Ozempic (semaglutide) is a prescription medication licensed in the UK for the treatment of type 2 diabetes mellitus. It belongs to a class of drugs known as glucagon-like peptide-1 (GLP-1) receptor agonists, which work by mimicking the action of a naturally occurring hormone that regulates blood sugar levels and appetite.
The medication is administered as a once-weekly subcutaneous injection with a recommended starting dose of 0.25 mg for the first 4 weeks, then increasing to 0.5 mg. The dose may be further increased to 1 mg and up to a maximum of 2 mg once weekly if needed for glycaemic control. Ozempic functions through several mechanisms: it stimulates insulin secretion from the pancreas when blood glucose levels are elevated, whilst simultaneously suppressing the release of glucagon, a hormone that raises blood sugar. Additionally, Ozempic slows gastric emptying, which helps to reduce post-meal glucose spikes and promotes a feeling of fullness that can lead to reduced calorie intake.
In the UK, Ozempic is licensed by the Medicines and Healthcare products Regulatory Agency (MHRA) specifically for glycaemic control in adults with type 2 diabetes. It is not indicated for patients with type 1 diabetes. According to National Institute for Health and Care Excellence (NICE) guidance (NG28), GLP-1 receptor agonists like Ozempic may be considered as part of triple therapy or in combination with insulin when specific criteria are met, including BMI thresholds and inadequate glycaemic control on existing treatments.
Whilst Ozempic has gained considerable attention for its associated weight loss effects, it is important to emphasise that weight reduction is a secondary benefit rather than its primary licensed indication in the UK. A related medication, Wegovy (also semaglutide but at a higher dose of 2.4 mg), is specifically licensed for weight management in certain patient groups. Understanding this distinction is crucial when considering how Ozempic might influence conditions related to excess weight, such as obstructive sleep apnoea.
The Link Between Obesity and Obstructive Sleep Apnoea
Obstructive sleep apnoea (OSA) is a common sleep disorder characterised by repeated episodes of partial or complete upper airway obstruction during sleep, leading to disrupted breathing patterns and fragmented sleep. These episodes, known as apnoeas or hypopnoeas, result in intermittent drops in blood oxygen levels and frequent micro-arousals that prevent restorative sleep. OSA severity is typically classified based on the apnoea-hypopnoea index (AHI): mild (5-14 events/hour), moderate (15-29 events/hour), or severe (≥30 events/hour).
Obesity is the most significant modifiable risk factor for OSA, with research indicating a strong association between increased body weight and OSA prevalence. Excess adipose tissue, particularly around the neck, throat, and upper body, contributes to airway narrowing through several mechanisms. Fat deposits in the pharyngeal walls reduce the airway diameter, whilst increased abdominal adiposity can impair respiratory mechanics and lung volumes. Additionally, obesity is associated with systemic inflammation that may affect upper airway muscle function and collapsibility.
The relationship between body weight and OSA severity is well-established, with studies showing that weight gain substantially increases the risk of developing OSA, while weight loss can improve OSA severity. Some patients experience significant improvement or even resolution of symptoms following substantial weight reduction.
OSA carries important health implications beyond poor sleep quality. Untreated OSA is associated with increased cardiovascular risk, including hypertension, atrial fibrillation, stroke, and coronary artery disease. It also contributes to daytime sleepiness, impaired cognitive function, reduced quality of life, and increased risk of road traffic accidents. People experiencing excessive sleepiness that could affect driving should stop driving and seek medical advice; some may need to notify the DVLA. For individuals with type 2 diabetes—the primary patient group prescribed Ozempic—OSA is particularly prevalent, creating a complex interplay between metabolic dysfunction, obesity, and sleep-disordered breathing that requires comprehensive management.
How Ozempic May Affect Sleep Apnoea Through Weight Loss
The potential benefit of Ozempic for individuals with obstructive sleep apnoea stems primarily from its weight loss effects rather than any direct action on the upper airway or respiratory control mechanisms. Clinical trials of semaglutide have demonstrated weight reduction, though the magnitude varies by dosage. At standard type 2 diabetes doses (0.5-1 mg weekly), patients typically lose around 4-7% of their initial body weight. Higher doses used in obesity treatment (2.4 mg weekly, marketed as Wegovy) have shown greater weight loss of 10-15% over 12-18 months when combined with lifestyle modifications.
This weight loss occurs through multiple pathways. Ozempic acts on appetite-regulating centres in the brain, particularly the hypothalamus, reducing hunger and increasing satiety. The medication also slows gastric emptying, prolonging the feeling of fullness after meals. These effects lead to a reduction in calorie intake without requiring conscious restriction, making sustained weight loss more achievable for many patients compared to diet and exercise alone.
When individuals with OSA lose significant weight, several beneficial anatomical and physiological changes occur. Reduction in neck circumference and pharyngeal fat deposits decreases upper airway collapsibility during sleep. Decreased abdominal adiposity improves lung volumes and respiratory mechanics, reducing the mechanical load on the respiratory system. Additionally, weight loss may reduce systemic inflammation and improve upper airway muscle tone and responsiveness.
It is important to note that there is no official direct pharmacological link between Ozempic and sleep apnoea improvement beyond that mediated by weight reduction. The medication does not specifically target the neural control of breathing, upper airway muscles, or other mechanisms directly involved in OSA pathophysiology. Therefore, any benefit observed in sleep apnoea outcomes should be understood as an indirect consequence of successful weight management rather than a primary therapeutic effect of the drug itself. Patients should not expect immediate improvements in OSA symptoms, as meaningful weight loss typically requires several months of treatment.
Clinical Evidence: Ozempic's Impact on Sleep Apnoea Outcomes
Emerging clinical evidence suggests that GLP-1 receptor agonists, including semaglutide, may improve obstructive sleep apnoea outcomes in patients who achieve significant weight loss. Several studies have examined this relationship, though it is important to note that most research has focused on higher-dose semaglutide formulations (2.4 mg weekly, marketed as Wegovy) rather than standard Ozempic dosing for type 2 diabetes.
Recent clinical trials (STEP-OSA 1 and 2) examined the effects of once-weekly semaglutide 2.4 mg in adults with obesity and moderate to severe OSA. These studies demonstrated that participants receiving semaglutide experienced reductions in the apnoea-hypopnoea index (AHI)—the primary measure of OSA severity—compared to placebo. The AHI reduction correlated strongly with the degree of weight loss achieved, with some participants experiencing significant improvement in OSA severity.
Additional benefits observed in clinical studies include:
-
Improved oxygen saturation during sleep
-
Reduced daytime sleepiness as measured by validated scales
-
Better sleep quality and reduced sleep fragmentation
-
Improvements in cardiovascular risk markers including blood pressure
-
Enhanced quality of life scores
However, several important caveats apply to this evidence base. Most studies have been conducted over relatively short timeframes (typically 12–18 months), and long-term data on sustained OSA improvement remain limited. Additionally, the magnitude of benefit varies considerably between individuals, with some patients experiencing dramatic improvements whilst others show more modest changes despite similar weight loss.
It is also crucial to recognise that weight loss through any means—whether medication, surgery, or lifestyle modification—can improve OSA. The evidence does not suggest that semaglutide has unique properties beyond its weight loss effects. Furthermore, most published studies have not specifically used the standard Ozempic formulation and dosing approved for type 2 diabetes, making direct extrapolation to routine clinical practice somewhat uncertain. In the UK, semaglutide is not licensed specifically for OSA treatment. Patients considering Ozempic should discuss realistic expectations with their healthcare provider.
Important Considerations and Potential Side Effects
Whilst Ozempic may offer indirect benefits for sleep apnoea through weight reduction, patients must be aware of potential side effects and important safety considerations before starting treatment. The medication is generally well-tolerated, but adverse effects are common, particularly during the initial weeks of therapy.
Gastrointestinal side effects are the most frequently reported and include:
-
Nausea (affecting 15–20% of patients)
-
Vomiting and diarrhoea
-
Constipation
-
Abdominal pain and bloating
-
Reduced appetite (which, whilst contributing to weight loss, can be distressing for some)
These symptoms typically improve over time as the body adjusts to the medication. Starting at a low dose (0.25 mg weekly) and gradually increasing, as per standard prescribing protocols, helps to minimise gastrointestinal disturbance.
More serious but less common adverse effects include:
-
Pancreatitis: Stop taking Ozempic and seek immediate medical attention if experiencing severe, persistent abdominal pain
-
Gallbladder problems: Rapid weight loss can increase the risk of gallstones
-
Hypoglycaemia: Particularly when used in combination with insulin or sulphonylureas
-
Diabetic retinopathy complications: Rapid glucose improvement may temporarily worsen retinopathy in susceptible individuals; appropriate monitoring is recommended
-
Acute kidney injury: Severe gastrointestinal side effects may lead to dehydration and kidney problems
Ozempic may also delay the absorption of some oral medications due to its effect on gastric emptying.
The main contraindication for Ozempic in the UK is hypersensitivity to semaglutide or any of the excipients. It is not recommended during pregnancy or breastfeeding, and women of childbearing potential should stop semaglutide at least two months before a planned pregnancy.
For individuals with OSA, there is no evidence that Ozempic worsens sleep apnoea symptoms. Patients using continuous positive airway pressure (CPAP) therapy should continue this treatment even if starting Ozempic, as weight loss takes time and OSA management should not be interrupted. Any decision to modify or discontinue CPAP should only be made following repeat sleep studies and under specialist guidance.
If you experience any side effects, talk to your doctor, pharmacist or nurse. This includes any possible side effects not listed in the package leaflet. You can also report side effects directly via the Yellow Card Scheme at yellowcard.mhra.gov.uk.
When to Speak to Your GP About Ozempic and Sleep Apnoea
If you have obstructive sleep apnoea and type 2 diabetes, or if you suspect you may have undiagnosed OSA, it is important to have an open conversation with your GP about whether Ozempic might be appropriate as part of your overall treatment plan.
You should consider discussing Ozempic with your GP if:
-
Your type 2 diabetes is not adequately controlled despite current medications
-
You meet the NICE criteria for GLP-1 receptor agonist therapy (typically involving specific BMI thresholds and inadequate control on other treatments)
-
You have been diagnosed with OSA and your healthcare team has recommended weight loss as part of your management plan
-
You are experiencing daytime sleepiness, loud snoring, or witnessed breathing pauses during sleep (potential signs of undiagnosed OSA)
Your GP will need to assess whether Ozempic is suitable based on your individual circumstances, including your current medications, HbA1c levels, BMI, and any contraindications. They may use validated screening tools like the STOP-Bang questionnaire or Epworth Sleepiness Scale to assess OSA risk or severity.
You should seek urgent medical advice if:
-
You experience severe, persistent abdominal pain whilst taking Ozempic (possible pancreatitis)
-
You develop signs of severe hypoglycaemia including confusion, loss of consciousness, or seizures
-
You notice sudden changes in vision
-
You experience severe allergic reactions such as facial swelling or difficulty breathing
-
You have significant dehydration from persistent vomiting or diarrhoea
If you experience excessive sleepiness that could affect your driving, you should stop driving and seek medical advice. Some people with OSA causing sleepiness must notify the DVLA.
It is also important to inform your GP if you are already receiving treatment for OSA, such as CPAP therapy or a mandibular advancement device. Do not discontinue existing OSA treatments when starting Ozempic without medical supervision. Weight loss takes time, and premature cessation of proven OSA therapies could expose you to significant health risks.
Finally, if you are considering treatment primarily for weight loss rather than diabetes management, discuss this openly with your GP. Whilst weight reduction may benefit OSA, Ozempic is not licensed in the UK specifically for weight management in people without diabetes. Wegovy (semaglutide 2.4 mg) is the licensed formulation for weight management in eligible patients. Your GP can advise on appropriate referral pathways for both OSA and weight management services within the NHS.
Frequently Asked Questions
Can Ozempic directly treat obstructive sleep apnoea?
No, Ozempic does not directly treat sleep apnoea. Any improvement in OSA symptoms occurs indirectly through weight loss, which reduces upper airway obstruction and improves breathing during sleep.
Should I stop using my CPAP machine if I start taking Ozempic?
No, you should continue CPAP therapy when starting Ozempic, as weight loss takes time and OSA management should not be interrupted. Any decision to modify CPAP should only be made following repeat sleep studies under specialist guidance.
Is Ozempic licensed in the UK for treating sleep apnoea?
No, Ozempic is licensed by the MHRA specifically for glycaemic control in adults with type 2 diabetes, not for sleep apnoea or weight management. Wegovy (semaglutide 2.4 mg) is the licensed formulation for weight management in eligible patients.
The health-related content published on this site is based on credible scientific sources and is periodically reviewed to ensure accuracy and relevance. Although we aim to reflect the most current medical knowledge, the material is meant for general education and awareness only.
The information on this site is not a substitute for professional medical advice. For any health concerns, please speak with a qualified medical professional. By using this information, you acknowledge responsibility for any decisions made and understand we are not liable for any consequences that may result.
Heading 1
Heading 2
Heading 3
Heading 4
Heading 5
Heading 6
Lorem ipsum dolor sit amet, consectetur adipiscing elit, sed do eiusmod tempor incididunt ut labore et dolore magna aliqua. Ut enim ad minim veniam, quis nostrud exercitation ullamco laboris nisi ut aliquip ex ea commodo consequat. Duis aute irure dolor in reprehenderit in voluptate velit esse cillum dolore eu fugiat nulla pariatur.
Block quote
Ordered list
- Item 1
- Item 2
- Item 3
Unordered list
- Item A
- Item B
- Item C
Bold text
Emphasis
Superscript
Subscript