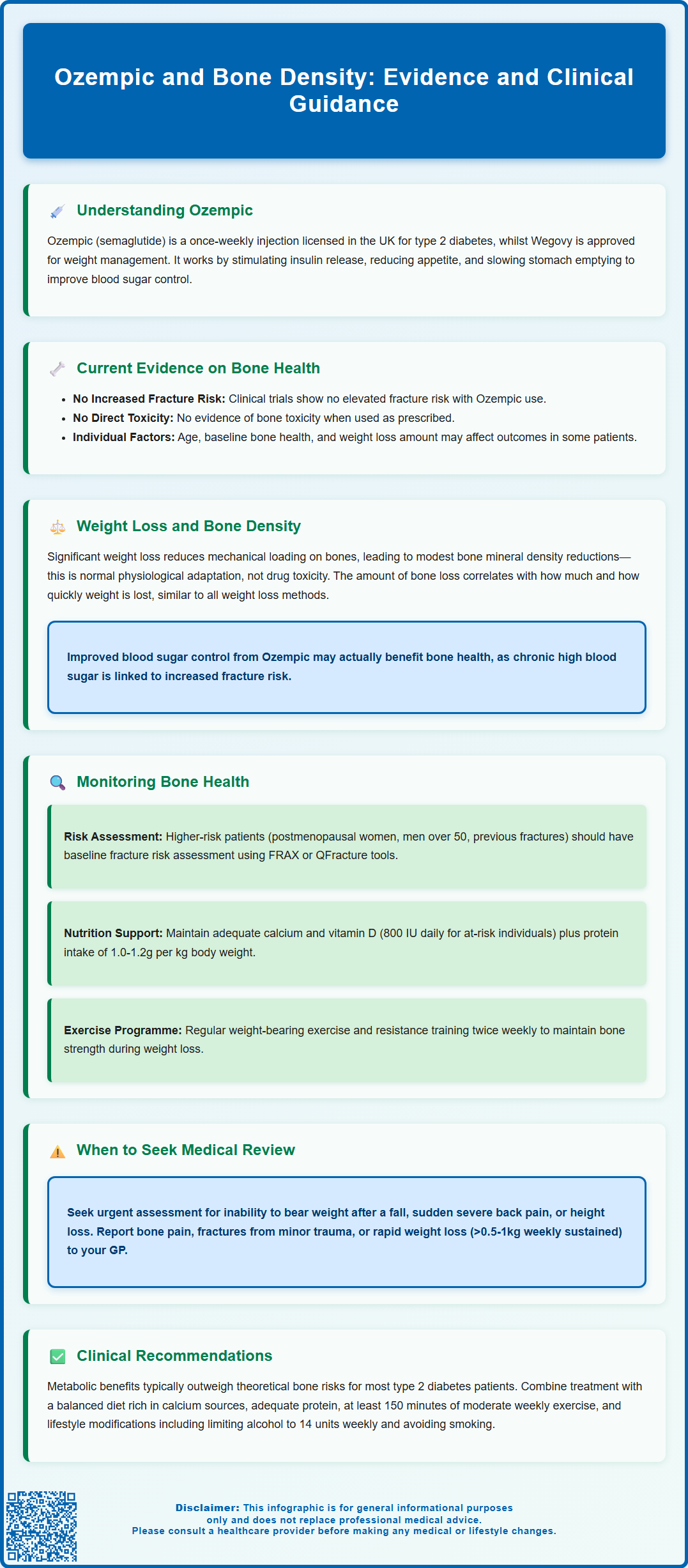
Ozempic (semaglutide) is a glucagon-like peptide-1 (GLP-1) receptor agonist widely prescribed for type 2 diabetes management in the UK. Whilst its efficacy in improving glycaemic control is well established, questions have emerged regarding ozempic and bone density, particularly as patients may experience substantial weight loss during treatment. Understanding the relationship between semaglutide therapy and skeletal health is essential for comprehensive patient care. Current evidence suggests no direct bone toxicity, though weight reduction itself may influence bone metabolism. This article examines the available evidence, explores mechanisms linking GLP-1 receptor agonists to bone health, and provides practical guidance for monitoring and supporting skeletal wellbeing in patients receiving Ozempic.
Summary: Current evidence shows no direct adverse effect of Ozempic on bone density, with large clinical trials demonstrating no increased fracture risk in patients with type 2 diabetes.
- Ozempic (semaglutide) is a GLP-1 receptor agonist licensed in the UK for type 2 diabetes management, administered as a once-weekly subcutaneous injection.
- Large-scale cardiovascular outcome trials have not identified increased fracture incidence with semaglutide compared to placebo or other diabetes treatments.
- Weight loss associated with Ozempic may lead to modest, adaptive bone density reductions due to decreased mechanical loading rather than direct bone toxicity.
- Risk-stratified monitoring is recommended for patients with additional osteoporosis risk factors, including postmenopausal women, those with previous fragility fractures, or patients taking corticosteroids.
- NICE guidance recommends fracture risk assessment using FRAX or QFracture tools, with DXA scanning arranged when results would influence management decisions.
- Patients should maintain adequate calcium and vitamin D intake, engage in regular weight-bearing exercise, and report unexplained bone pain or fractures to their healthcare provider.
Table of Contents
Understanding Ozempic and Its Primary Uses
Ozempic (semaglutide) is a glucagon-like peptide-1 (GLP-1) receptor agonist licensed in the UK for the treatment of type 2 diabetes mellitus in adults. It is important to note that while Ozempic is licensed for diabetes management, a higher-dose formulation (Wegovy) is separately licensed for weight management. Administered as a once-weekly subcutaneous injection, Ozempic works by mimicking the action of the naturally occurring hormone GLP-1, which plays a crucial role in glucose regulation and appetite control.
The primary mechanism of action involves several complementary pathways. Ozempic stimulates insulin secretion from pancreatic beta cells in a glucose-dependent manner, meaning it only promotes insulin release when blood glucose levels are elevated. Simultaneously, it suppresses glucagon secretion, reducing hepatic glucose production. Additionally, semaglutide slows gastric emptying (though this effect may attenuate with chronic dosing) and acts on appetite centres in the brain to reduce food intake.
In UK clinical practice, NICE guidance (NG28) recommends GLP-1 receptor agonists like Ozempic as part of a treatment pathway that considers specific criteria. These include inadequate glycaemic control despite optimised therapy, higher BMI thresholds (typically ≥35 kg/m²), and consideration of cardiovascular risk factors. NICE also specifies continuation criteria based on HbA1c and weight reduction targets. Ozempic is part of a comprehensive diabetes management strategy that includes dietary modification and physical activity.
Whilst Ozempic's glucose-lowering and weight-reduction properties are well established, questions have emerged regarding its potential effects on other physiological systems, including bone metabolism and skeletal health. Understanding these broader impacts is essential for comprehensive patient care, particularly in populations already at risk of osteoporosis or fractures.
Current Evidence on Ozempic and Bone Density
The relationship between Ozempic and bone density remains an area of ongoing research, with current evidence suggesting no signal of increased fracture risk in most patients. Clinical trials evaluating semaglutide have not identified bone loss as a significant adverse effect, though it should be noted that bone mineral density (BMD) was not specifically assessed in most studies.
Large-scale cardiovascular outcome trials, including the SUSTAIN programme, have monitored safety parameters including fractures as adverse events. These studies, which followed thousands of patients over several years, did not demonstrate an increased incidence of fractures compared to placebo or other diabetes treatments. The European Medicines Agency (EMA) assessment and the Medicines and Healthcare products Regulatory Agency (MHRA) have not issued specific warnings regarding bone health concerns with semaglutide use.
However, it is important to distinguish between direct pharmacological effects and indirect consequences of treatment. GLP-1 receptors are expressed in bone tissue, and preclinical studies have explored their role in bone metabolism. Some animal research suggests GLP-1 receptor agonists may influence bone metabolism, though translating these findings to human clinical practice requires caution.
The current consensus among endocrinologists and diabetologists is that there is no evidence of direct bone toxicity with Ozempic when used as directed for its licensed indication. Nonetheless, individual patient factors—including age, sex, baseline bone health, nutritional status, and the extent of weight loss—may influence skeletal outcomes. Clinicians should maintain awareness of these variables when prescribing GLP-1 receptor agonists, particularly in patients with pre-existing osteoporosis or multiple fracture risk factors.
It's worth noting that higher-dose semaglutide for obesity (Wegovy) involves greater weight loss, which could potentially have indirect effects on bone density through mechanisms discussed in the next section.
Weight Loss, Bone Health, and GLP-1 Receptor Agonists
One of the most significant considerations when evaluating bone health in patients taking Ozempic is the substantial weight loss many individuals experience. Whilst weight reduction offers numerous metabolic and cardiovascular benefits, rapid or extensive weight loss can have implications for skeletal health, regardless of the method by which it is achieved.
Mechanical loading is a fundamental stimulus for bone maintenance and remodelling. Weight-bearing activity and body mass provide continuous stress signals that promote bone formation and prevent excessive resorption. When significant weight is lost, particularly over a relatively short period, the reduction in mechanical load may lead to adaptive bone loss. This phenomenon is not unique to pharmacological weight loss—it has been observed with bariatric surgery, very low-calorie diets, and other weight reduction interventions.
Research examining weight loss and bone density has shown that individuals losing substantial amounts of weight may experience modest reductions in BMD, particularly at weight-bearing sites such as the hip and lumbar spine. The magnitude of bone loss appears to correlate with the amount and rate of weight reduction. However, it is crucial to note that this represents a physiological adaptation to reduced mechanical stress rather than a direct toxic effect on bone tissue.
For patients taking Ozempic, the bone health implications of weight loss may be influenced by several factors:
-
Improved glycaemic control itself may benefit bone health, as chronic hyperglycaemia is associated with increased fracture risk
-
Changes in inflammatory markers accompanying weight loss may influence bone metabolism
-
Enhanced mobility and physical activity often follow weight reduction, providing beneficial mechanical stimulation
-
Nutritional adequacy as part of comprehensive diabetes care supports skeletal health
It's important to monitor dietary intake, particularly if gastrointestinal side effects like nausea or early satiety reduce food consumption. Involving a dietitian may be beneficial for patients experiencing significant appetite changes or nutritional challenges.
Clinicians should adopt a balanced perspective, recognising that the overall health benefits of appropriate weight loss in type 2 diabetes typically outweigh theoretical concerns about bone density, whilst remaining vigilant about bone health in higher-risk individuals.
Monitoring Bone Health During Ozempic Treatment
Whilst routine bone density monitoring is not required for all patients commencing Ozempic, a risk-stratified approach to skeletal health assessment is prudent, particularly for individuals with additional risk factors for osteoporosis or fractures.
Baseline assessment should identify patients who may warrant closer monitoring:
-
Postmenopausal women and men over 50 years
-
Individuals with a previous fragility fracture
-
Patients with a family history of osteoporosis or hip fracture
-
Those with low body mass index (BMI <18.5 kg/m²) prior to treatment
-
Patients taking medications that affect bone metabolism (e.g., corticosteroids, aromatase inhibitors)
-
Individuals with conditions affecting bone health (e.g., coeliac disease, inflammatory bowel disease, chronic kidney disease)
-
Those with vitamin D deficiency or inadequate calcium intake
In line with NICE guidance (NG226), fracture risk evaluation using tools such as FRAX (Fracture Risk Assessment Tool) or QFracture should be performed to estimate 10-year fracture probability. DXA scanning (dual-energy X-ray absorptiometry) should be arranged if the results would influence management decisions, following National Osteoporosis Guideline Group (NOGG) intervention thresholds.
During treatment, monitoring should include:
-
Regular review of calcium and vitamin D status, with supplementation as needed (typically 20 micrograms [800 IU] vitamin D daily for those at risk; calcium supplementation only if dietary intake is inadequate)
-
Nutritional assessment to ensure adequate protein intake during weight loss (minimum 1.0-1.2g/kg body weight)
-
Encouragement of weight-bearing exercise and resistance training to maintain bone strength, in line with UK Chief Medical Officers' Physical Activity Guidelines
-
Medication review to identify and address other factors affecting bone health
-
Repeat fracture risk assessment in high-risk patients, with DXA scanning as clinically indicated based on NICE/NOGG guidance
Patients experiencing weight loss faster than planned (particularly if exceeding 0.5-1kg per week sustained over several weeks) should be reviewed to ensure nutritional adequacy and consider whether treatment adjustment is appropriate.
Red flags requiring urgent assessment include inability to weight-bear after a fall, sudden severe back pain, or height loss suggesting vertebral fracture. These symptoms require prompt clinical evaluation through appropriate local pathways.
Clinical Recommendations and Patient Considerations
Healthcare professionals prescribing Ozempic should adopt a holistic approach to patient care that addresses bone health within the broader context of diabetes management and cardiovascular risk reduction. The following recommendations support optimal outcomes:
Prescribing decisions should be individualised, weighing the substantial benefits of improved glycaemic control and weight reduction against any theoretical skeletal concerns. For the vast majority of patients with type 2 diabetes, the metabolic advantages clearly outweigh any potential bone-related risks. However, in patients with severe osteoporosis or very high fracture risk, discussion of alternative treatment options may be appropriate.
Patient education is essential. Individuals commencing Ozempic should understand:
-
The importance of adequate calcium and vitamin D intake through diet and supplementation if indicated
-
The value of regular physical activity in line with UK guidance (at least 150 minutes of moderate intensity activity weekly, plus strength exercises on 2 days per week)
-
The need to report any bone pain, fractures, or significant height loss
-
That gradual, sustained weight loss is preferable to rapid reduction
-
The overall safety profile of the medication and no evidence of direct bone toxicity
-
The importance of reporting suspected side effects via the MHRA Yellow Card Scheme
Lifestyle interventions should be emphasised as integral to treatment success. Patients should be encouraged to:
-
Consume a balanced diet rich in calcium (dairy products, fortified plant-based alternatives, leafy greens)
-
Ensure adequate protein intake to preserve lean muscle mass during weight loss
-
Engage in regular physical activity following UK Chief Medical Officers' guidelines
-
Limit alcohol consumption to no more than 14 units per week, spread over 3 or more days
-
Avoid smoking, which impairs bone health
-
Maintain safe home environments to reduce fall risk
When to seek medical advice: Patients should contact their GP or diabetes specialist nurse if they experience unexplained bone pain, sustain a fracture from minimal trauma, or have concerns about their bone health. Those with multiple risk factors for osteoporosis should discuss whether formal bone density assessment is appropriate. Patients with suspected vertebral fractures or inability to weight-bear after a fall should seek urgent assessment.
In summary, whilst vigilance regarding bone health is appropriate for all patients with diabetes, current evidence does not support withholding Ozempic due to bone density concerns in most individuals. A personalised, risk-stratified approach that optimises nutrition, encourages physical activity, and monitors high-risk patients ensures that the considerable benefits of GLP-1 receptor agonist therapy can be realised whilst maintaining skeletal health.
Scientific References
- Ozempic 0.5 mg solution for injection in pre-filled pen - Summary of Product Characteristics.
- Ozempic | European Medicines Agency.
- Ozempic, INN-semaglutide - EPAR Product Information (SUSTAIN trials).
- Osteoporosis: assessing the risk of fragility fracture. NICE guideline CG146 (NG226).
- Bone Mineral Density Response to Caloric Restriction–Induced Weight Loss.
- Bone Health After Exercise Alone, GLP-1 Receptor Agonist (Systematic Review).
Frequently Asked Questions
Does Ozempic cause bone loss or increase fracture risk?
Current evidence from large clinical trials shows no increased fracture risk with Ozempic. Whilst weight loss may lead to modest adaptive bone density changes, there is no evidence of direct bone toxicity from semaglutide when used as directed for type 2 diabetes.
Should I have a bone density scan before starting Ozempic?
Routine bone density scanning is not required for all patients starting Ozempic. However, individuals with additional risk factors such as postmenopausal status, previous fragility fractures, or corticosteroid use should undergo fracture risk assessment using FRAX or QFracture, with DXA scanning arranged if results would influence management.
How can I protect my bone health whilst taking Ozempic?
Maintain adequate calcium and vitamin D intake through diet or supplementation, engage in regular weight-bearing exercise and resistance training as per UK guidance, ensure sufficient protein intake during weight loss, and attend regular reviews with your healthcare team to monitor bone health if you have additional risk factors.
The health-related content published on this site is based on credible scientific sources and is periodically reviewed to ensure accuracy and relevance. Although we aim to reflect the most current medical knowledge, the material is meant for general education and awareness only.
The information on this site is not a substitute for professional medical advice. For any health concerns, please speak with a qualified medical professional. By using this information, you acknowledge responsibility for any decisions made and understand we are not liable for any consequences that may result.
Heading 1
Heading 2
Heading 3
Heading 4
Heading 5
Heading 6
Lorem ipsum dolor sit amet, consectetur adipiscing elit, sed do eiusmod tempor incididunt ut labore et dolore magna aliqua. Ut enim ad minim veniam, quis nostrud exercitation ullamco laboris nisi ut aliquip ex ea commodo consequat. Duis aute irure dolor in reprehenderit in voluptate velit esse cillum dolore eu fugiat nulla pariatur.
Block quote
Ordered list
- Item 1
- Item 2
- Item 3
Unordered list
- Item A
- Item B
- Item C
Bold text
Emphasis
Superscript
Subscript