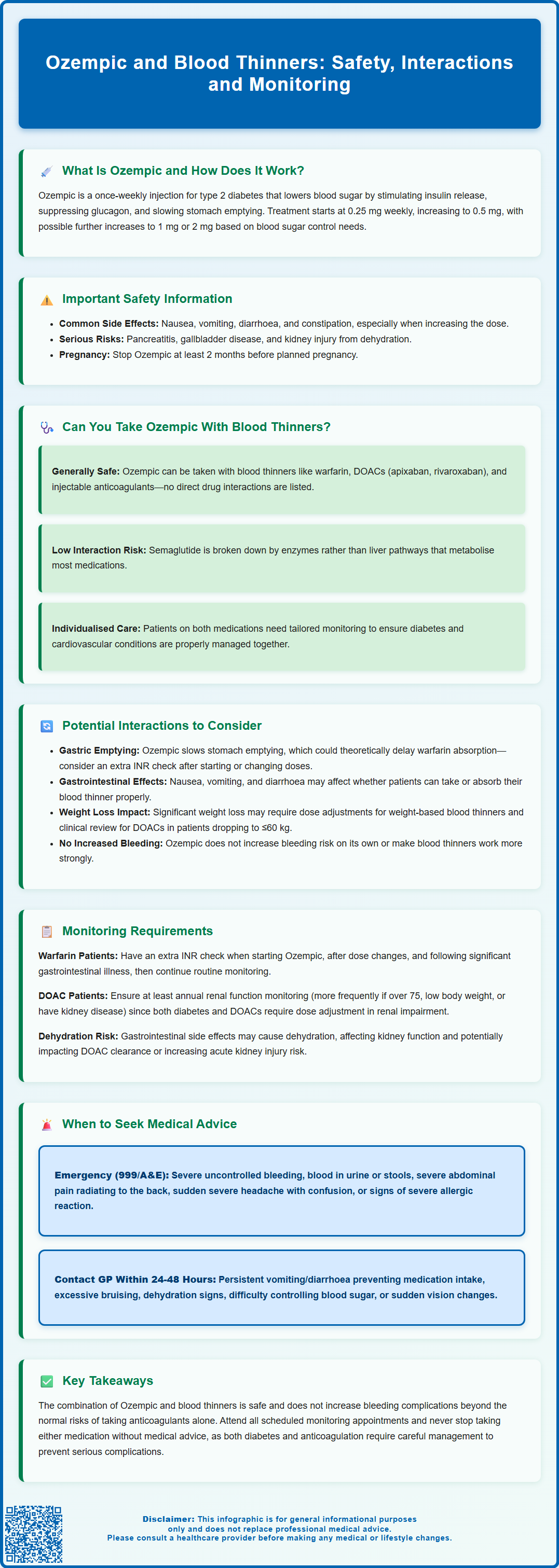
Many patients with type 2 diabetes require both glucose-lowering medication and anticoagulation therapy for conditions such as atrial fibrillation or previous cardiovascular events. Ozempic (semaglutide), a glucagon-like peptide-1 (GLP-1) receptor agonist, is commonly prescribed for type 2 diabetes management, whilst blood thinners prevent dangerous blood clots. Understanding whether Ozempic and blood thinners can be safely combined is essential for patients managing multiple conditions. This article examines the evidence on concurrent use, potential interactions, monitoring requirements, and safety considerations aligned with UK clinical guidance from NICE, the MHRA, and the BNF.
Summary: Ozempic can generally be taken safely alongside blood thinners, as no direct pharmacological interaction exists between semaglutide and anticoagulants.
- Ozempic (semaglutide) is a GLP-1 receptor agonist licensed in the UK for type 2 diabetes treatment, administered as a once-weekly subcutaneous injection.
- No contraindication exists for concurrent use with anticoagulants including warfarin, DOACs (apixaban, rivaroxaban, edoxaban, dabigatran), or low-molecular-weight heparins.
- Indirect effects warrant monitoring: gastric emptying may theoretically affect oral medication absorption, and weight loss may necessitate anticoagulant dose review.
- Patients taking warfarin should continue routine INR monitoring, with consideration of extra checks after initiating Ozempic or following dose changes.
- Seek immediate medical attention for severe bleeding, persistent abdominal pain radiating to the back, blood in urine or stools, or sudden neurological symptoms.
Table of Contents
What Is Ozempic and How Does It Work?
Ozempic (semaglutide) is a prescription medication licensed in the UK for the treatment of type 2 diabetes mellitus in adults. It belongs to a class of drugs known as glucagon-like peptide-1 (GLP-1) receptor agonists, which work by mimicking the action of a naturally occurring hormone that regulates blood glucose levels.
The mechanism of action of Ozempic involves several complementary pathways. Firstly, it stimulates insulin secretion from pancreatic beta cells in a glucose-dependent manner, meaning insulin is released only when blood glucose levels are elevated. This reduces the risk of hypoglycaemia compared to some other diabetes medications. Secondly, semaglutide suppresses glucagon release, a hormone that raises blood glucose by promoting hepatic glucose production. Thirdly, it slows gastric emptying, which moderates the rate at which glucose enters the bloodstream after meals.
Ozempic is administered as a once-weekly subcutaneous injection, starting at 0.25 mg for 4 weeks as an initiation dose (not for glycaemic control), then typically 0.5 mg weekly. The dose can be increased to 1 mg or 2 mg weekly if needed for improved glycaemic control. Ozempic is not licensed for weight loss alone in the UK, though many patients experience weight loss as a secondary benefit.
Common adverse effects include gastrointestinal symptoms such as nausea, vomiting, diarrhoea, and constipation, particularly during dose escalation. Important safety considerations include risk of pancreatitis (stop treatment and seek urgent care if severe persistent abdominal pain radiating to the back occurs), gallbladder disease, diabetic retinopathy complications (especially with rapid improvement in blood glucose control), and risk of acute kidney injury with dehydration. When used with insulin or sulfonylureas, there is an increased risk of hypoglycaemia.
Ozempic is not indicated for patients with type 1 diabetes or diabetic ketoacidosis. The medication should be discontinued at least 2 months before a planned pregnancy.
Can You Take Ozempic With Blood Thinners?
Yes, Ozempic can generally be taken alongside blood thinners (anticoagulants). No contraindication is listed in the UK Summary of Product Characteristics (SmPC), and no clinically relevant pharmacokinetic interactions are expected. Many patients with type 2 diabetes require anticoagulation therapy for conditions such as atrial fibrillation, venous thromboembolism, or following cardiovascular events, making this combination relatively common in clinical practice.
Blood thinners encompass several medication classes, including warfarin (a vitamin K antagonist), direct oral anticoagulants (DOACs) such as apixaban, rivaroxaban, edoxaban, and dabigatran, as well as injectable anticoagulants like low-molecular-weight heparins (enoxaparin, dalteparin). Each of these works through different mechanisms to prevent blood clot formation, and none have a direct pharmacological interaction with semaglutide's GLP-1 receptor activity.
The pharmacokinetic profile of Ozempic does not suggest significant interactions with anticoagulant metabolism. Semaglutide is primarily degraded by proteolytic enzymes rather than hepatic cytochrome P450 enzymes, which are responsible for metabolising many medications, including warfarin. This reduces the likelihood of drug-drug interactions at the metabolic level.
However, whilst there is no direct interaction, indirect effects warrant consideration. Ozempic's impact on gastric emptying and gastrointestinal function could theoretically affect the absorption of oral medications. Additionally, weight loss and dietary changes (vitamin K intake) can alter warfarin dose requirements. Patients with diabetes who are on anticoagulation require individualised assessment of their overall cardiovascular and metabolic risk profile, ensuring that both conditions are optimally managed in parallel.
Potential Interactions Between Ozempic and Anticoagulants
Whilst no direct pharmacological interaction exists between Ozempic and blood thinners, several indirect considerations merit clinical attention. Understanding these potential effects helps ensure safe and effective concurrent therapy.
Gastric emptying and medication absorption represent the primary theoretical concern. Ozempic slows gastric emptying, which could potentially delay the absorption of oral anticoagulants, particularly warfarin. However, clinically relevant effects on oral anticoagulants are not expected based on available data. For patients taking warfarin, it may be prudent to arrange an extra INR check after initiating Ozempic, after dose changes, or following significant gastrointestinal illness.
Gastrointestinal adverse effects associated with Ozempic, particularly nausea, vomiting, and diarrhoea, could theoretically impact medication adherence or absorption. Patients experiencing significant gastrointestinal symptoms should be monitored to ensure they continue taking their anticoagulant as prescribed and that absorption is not compromised. If unable to keep down DOAC doses due to vomiting, patients should contact their healthcare provider.
Weight loss induced by Ozempic may necessitate dose adjustments for weight-based anticoagulants, such as low-molecular-weight heparins. Substantial weight loss may also affect DOAC dose criteria for some agents (e.g., apixaban and edoxaban in patients ≤60 kg) and warrants clinical review. For warfarin users, significant weight changes can occasionally affect dosing requirements, managed through routine INR monitoring.
There is no evidence that Ozempic increases bleeding risk independently, nor does it potentiate the anticoagulant effects of blood thinners. The medication does not affect platelet function or coagulation cascade components. Patients can be reassured that the combination does not inherently increase haemorrhagic complications beyond the baseline risk associated with anticoagulation therapy alone.
Safety Considerations and Monitoring Requirements
When prescribing Ozempic to patients taking blood thinners, healthcare professionals should implement appropriate monitoring strategies to ensure optimal safety and therapeutic outcomes. These considerations align with NICE guidance on diabetes management and anticoagulation monitoring.
For patients taking warfarin, routine INR monitoring should continue as per established protocols. When initiating Ozempic, consider arranging an extra INR check after starting treatment, after dose changes, and following significant gastrointestinal illness. Continue routine INR monitoring thereafter.
Patients prescribed DOACs (apixaban, rivaroxaban, edoxaban, dabigatran) require renal function monitoring at least annually, and more frequently in those aged over 75, with low body weight, intercurrent illness, or chronic kidney disease. Both diabetes and some DOACs require dose adjustment in renal impairment. Ozempic is generally well-tolerated in patients with mild to moderate renal impairment, though caution is advised in severe renal disease.
Key safety considerations include:
-
Bleeding risk assessment: Ensure patients understand signs of bleeding (unusual bruising, blood in urine or stools, prolonged bleeding from cuts) and when to seek help
-
Medication adherence: Address any gastrointestinal side effects promptly to prevent non-adherence to either medication
-
Hydration status: Gastrointestinal adverse effects may cause dehydration, which can affect renal function and potentially impact DOAC clearance or increase risk of acute kidney injury
-
Injection site management: Patients should rotate Ozempic injection sites and avoid injecting into areas with bruising or active bleeding
-
Pancreatitis awareness: Stop Ozempic and seek urgent medical attention if severe persistent abdominal pain radiating to the back occurs
-
Diabetic retinopathy monitoring: Particularly important in patients with pre-existing retinopathy
-
Hypoglycaemia risk: Increased when Ozempic is used with insulin or sulfonylureas
Patient education is paramount. Individuals should be counselled about the importance of maintaining both medications as prescribed, recognising adverse effects, and understanding that whilst the combination is generally safe, vigilance for bleeding symptoms remains essential. Suspected side effects should be reported via the MHRA Yellow Card scheme (yellowcard.mhra.gov.uk).
When to Seek Medical Advice About This Combination
Patients taking both Ozempic and blood thinners should be aware of specific circumstances that warrant prompt medical attention. Clear guidance on when to contact healthcare services ensures timely intervention and prevents complications.
Seek immediate medical attention (call 999 or attend A&E) if you experience:
-
Severe bleeding that won't stop, including nosebleeds lasting more than 10 minutes, vomiting blood, or coughing up blood
-
Blood in urine (pink, red, or dark brown discolouration) or black, tarry stools
-
Severe, persistent abdominal pain radiating to the back, with or without vomiting (possible pancreatitis) – also stop taking Ozempic
-
Sudden severe headache, confusion, vision changes, or weakness, which could indicate intracranial bleeding
-
Signs of severe allergic reaction to Ozempic, including facial swelling, difficulty breathing, or widespread rash
Contact your GP or diabetes specialist nurse within 24–48 hours if:
-
Persistent gastrointestinal symptoms (nausea, vomiting, diarrhoea) that prevent you from taking medications or maintaining hydration
-
Unusual bruising or bleeding that seems excessive for minor trauma
-
Signs of dehydration including reduced urination, dizziness, or extreme thirst
-
Difficulty managing blood glucose levels or unexplained hypoglycaemia
-
Sudden visual changes or new floaters (possible retinopathy or vitreous haemorrhage)
For urgent but non-emergency concerns, contact NHS 111 for advice.
Routine follow-up should include discussion of this medication combination at your next scheduled appointment. If you're taking warfarin, attend all scheduled INR monitoring appointments. For patients on DOACs, ensure annual renal function testing is completed as recommended.
Before starting Ozempic, inform your prescriber about all medications you take, including over-the-counter products and supplements. Some herbal preparations can interact with anticoagulants, and comprehensive medication reconciliation ensures safe prescribing. If you're considering stopping either medication, never discontinue without medical advice, as both diabetes control and anticoagulation require careful management to prevent serious complications.
Frequently Asked Questions
Does Ozempic interact with warfarin or other blood thinners?
No direct pharmacological interaction exists between Ozempic and anticoagulants. However, patients taking warfarin should continue routine INR monitoring, with consideration of extra checks after starting Ozempic or following dose changes, as weight loss and dietary changes may occasionally affect warfarin requirements.
Can Ozempic increase bleeding risk when taken with anticoagulants?
Ozempic does not independently increase bleeding risk or potentiate anticoagulant effects. It does not affect platelet function or coagulation pathways, so the combination does not inherently increase haemorrhagic complications beyond the baseline risk of anticoagulation therapy alone.
What monitoring is required when taking Ozempic with blood thinners?
Continue routine anticoagulation monitoring as prescribed: INR checks for warfarin users and annual renal function testing for DOAC users. Monitor for gastrointestinal side effects that could affect medication adherence, maintain hydration, and remain vigilant for bleeding symptoms requiring prompt medical attention.
The health-related content published on this site is based on credible scientific sources and is periodically reviewed to ensure accuracy and relevance. Although we aim to reflect the most current medical knowledge, the material is meant for general education and awareness only.
The information on this site is not a substitute for professional medical advice. For any health concerns, please speak with a qualified medical professional. By using this information, you acknowledge responsibility for any decisions made and understand we are not liable for any consequences that may result.
Heading 1
Heading 2
Heading 3
Heading 4
Heading 5
Heading 6
Lorem ipsum dolor sit amet, consectetur adipiscing elit, sed do eiusmod tempor incididunt ut labore et dolore magna aliqua. Ut enim ad minim veniam, quis nostrud exercitation ullamco laboris nisi ut aliquip ex ea commodo consequat. Duis aute irure dolor in reprehenderit in voluptate velit esse cillum dolore eu fugiat nulla pariatur.
Block quote
Ordered list
- Item 1
- Item 2
- Item 3
Unordered list
- Item A
- Item B
- Item C
Bold text
Emphasis
Superscript
Subscript












