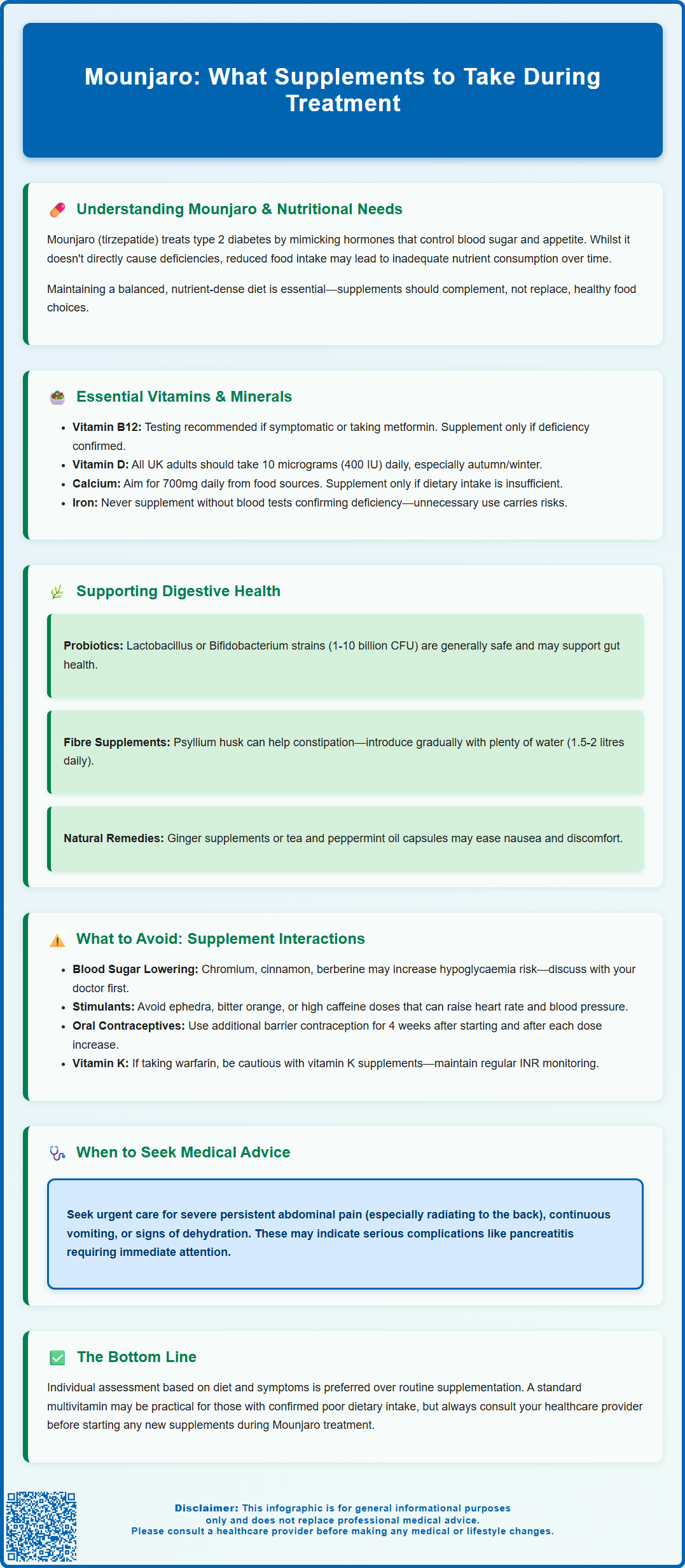
Mounjaro (tirzepatide) is a dual GLP-1 and GIP receptor agonist licensed in the UK for type 2 diabetes management, with significant effects on appetite and gastric emptying. Many patients wonder what supplements to take with Mounjaro to support nutritional health during treatment. Whilst the medication doesn't directly cause deficiencies, reduced food intake may affect vitamin and mineral status over time. This guide examines evidence-based supplementation strategies, focusing on maintaining nutritional adequacy, managing gastrointestinal symptoms, and avoiding potential interactions. A balanced, nutrient-dense diet remains paramount, with supplements serving as targeted support rather than routine additions for all patients.
Summary: Mounjaro patients should prioritise a balanced diet, with supplements considered only for confirmed deficiencies or insufficient dietary intake, focusing on vitamin B12, vitamin D, and calcium when clinically indicated.
- Tirzepatide is a dual GLP-1/GIP receptor agonist that slows gastric emptying and reduces appetite, potentially affecting nutritional intake.
- Vitamin B12 testing is recommended for symptomatic patients, particularly those also taking metformin, rather than routine supplementation.
- Standard vitamin D supplementation (10 micrograms daily) follows NHS guidance for UK adults, especially during autumn and winter months.
- Probiotics and fibre supplements may support digestive comfort, though evidence specifically for GLP-1/GIP agonist-related symptoms remains limited.
- Supplements affecting blood glucose or gastric emptying require medical discussion to avoid interactions with diabetes management or oral contraceptives.
- Patients should report severe abdominal pain, persistent vomiting, or dehydration urgently, as these may indicate serious complications requiring medical assessment.
Table of Contents
Understanding Mounjaro and Nutritional Needs
Mounjaro (tirzepatide) is a glucagon-like peptide-1 (GLP-1) and glucose-dependent insulinotropic polypeptide (GIP) receptor agonist licensed in the UK for the treatment of type 2 diabetes mellitus. For weight management in adults with obesity or overweight with weight-related comorbidities, the same molecule is marketed under the brand name Zepbound, with specific NICE eligibility criteria for use within specialist services.
The medication works by mimicking naturally occurring incretin hormones, which enhance insulin secretion, suppress glucagon release, slow gastric emptying, and reduce appetite. These mechanisms contribute to improved glycaemic control and significant weight loss in many patients.
Whilst Mounjaro is generally well-tolerated, its effects on the gastrointestinal system can influence nutritional intake and absorption. The slowed gastric emptying and reduced appetite often lead to decreased food consumption, which may result in lower intake of essential vitamins and minerals. Patients frequently report feeling fuller for longer periods and may struggle to consume adequate portions at mealtimes. This reduction in dietary variety and volume raises important considerations regarding nutritional adequacy during treatment.
It is essential to recognise that Mounjaro itself does not directly cause vitamin or mineral deficiencies. However, the secondary effects of reduced caloric intake and altered eating patterns may predispose some individuals to suboptimal nutritional status over time. Patients with type 2 diabetes taking metformin may be at particular risk of vitamin B12 deficiency and should discuss screening with their healthcare provider if symptomatic.
Healthcare professionals should assess individual dietary habits and consider baseline nutritional screening, particularly in patients with pre-existing deficiencies or those at higher risk due to restrictive eating patterns. Maintaining a balanced, nutrient-dense diet remains the cornerstone of nutritional health during Mounjaro therapy, with supplementation serving as an adjunct rather than a replacement for wholesome food choices.
Importantly, patients should seek urgent medical advice if they experience severe, persistent abdominal pain (particularly if radiating to the back), persistent vomiting, or signs of dehydration, as these may indicate serious conditions such as pancreatitis or gallbladder disease.
Essential Vitamins and Minerals During Mounjaro Treatment
Patients taking Mounjaro should focus primarily on maintaining a balanced diet, with supplementation considered only when dietary intake is insufficient or specific deficiencies are identified through clinical assessment or blood tests.
Vitamin B12 deserves attention, particularly in patients also taking metformin, as both reduced food intake and altered gastric function may affect absorption of this essential nutrient. B12 deficiency can develop insidiously, leading to fatigue, neurological symptoms, and macrocytic anaemia. Rather than routine supplementation, targeted testing is recommended for symptomatic patients or those at risk. If deficiency is confirmed, a standard oral B12 supplement (typically 25–100 micrograms daily) or a comprehensive B-complex vitamin may be appropriate, though those with confirmed deficiency may require higher doses or intramuscular administration as directed by their GP.
Vitamin D supplementation is recommended for most UK adults, particularly during autumn and winter months when sunlight exposure is insufficient for adequate synthesis. The NHS advises 10 micrograms (400 IU) daily for the general population. While patients with obesity may have lower vitamin D levels, supplementation should generally follow standard NHS guidance unless otherwise directed by a healthcare professional, with a safe upper limit of 100 micrograms (4,000 IU) daily unless clinically indicated. Adequate vitamin D status supports bone health, immune function, and may play a role in metabolic health.
Calcium intake deserves attention, especially if dairy consumption decreases due to reduced appetite or gastrointestinal symptoms. Adults typically require 700 milligrams daily, ideally from dietary sources such as dairy products, fortified plant-based alternatives, or leafy green vegetables. If dietary assessment confirms insufficient intake, calcium supplementation (500–600 milligrams daily) may be warranted, preferably taken separately from iron supplements to optimise absorption. Patients should be aware that calcium supplements can contribute to constipation and, rarely, kidney stones.
Iron supplementation should only be initiated after appropriate testing (ferritin, full blood count) confirms deficiency. Patients experiencing fatigue should discuss iron assessment with their healthcare provider, as deficiency anaemia can be mistaken for medication side effects. Unnecessary iron supplementation carries risks and should be avoided without clinical indication.
A standard multivitamin and mineral supplement providing approximately 100% of reference nutrient intakes may offer a practical foundation for patients with confirmed poor dietary intake, though individual needs should be assessed based on dietary patterns, symptoms, and blood test results where clinically indicated.
Supplements to Support Digestive Health on Mounjaro
Gastrointestinal side effects represent the most commonly reported adverse reactions to Mounjaro, with nausea, vomiting, diarrhoea, constipation, and abdominal discomfort affecting a substantial proportion of patients, particularly during dose escalation. Whilst these symptoms typically diminish over time as tolerance develops, certain supplements may help support digestive comfort and gut health during treatment.
Probiotics have gained attention for their potential role in supporting gastrointestinal function, though evidence specifically in patients taking GLP-1/GIP receptor agonists remains limited. These live microorganisms may help maintain a healthy gut microbiome, which can be disrupted by changes in dietary patterns, medication effects, or gastrointestinal symptoms. Probiotic strains such as Lactobacillus and Bifidobacterium species are generally considered safe for most people and may offer modest benefits for digestive regularity and comfort. Patients should select products with clearly stated colony-forming units (typically 1–10 billion CFU daily) and specific strains with evidence for their intended use. Storage requirements vary by product; many UK probiotics are shelf-stable while others require refrigeration. Immunocompromised patients should consult their healthcare provider before taking probiotics. There is no established link between probiotic supplementation and improved outcomes specifically for Mounjaro-related gastrointestinal symptoms.
Fibre supplementation may assist patients experiencing constipation, a common side effect of slowed gastric emptying. Soluble fibre supplements such as psyllium husk or methylcellulose can promote regular bowel movements when taken with adequate fluid intake. Patients should introduce fibre gradually to avoid exacerbating bloating or discomfort, starting with small doses and increasing as tolerated. Those experiencing significant upper gastrointestinal symptoms or gastroparesis should be cautious with bulking agents, which may worsen symptoms in some cases. Adequate hydration is essential when using fibre supplements, with at least 1.5–2 litres of fluid daily recommended for most adults.
Ginger supplements or ginger tea may provide natural relief from nausea for some individuals, though evidence is largely based on other contexts such as pregnancy-related or postoperative nausea. Peppermint oil capsules have been studied for irritable bowel syndrome and may help with abdominal discomfort, though patients should choose enteric-coated formulations to prevent oesophageal irritation.
Patients should seek medical advice promptly if they experience severe or persistent gastrointestinal symptoms, signs of dehydration, or significant abdominal pain, as these may require dose adjustment, medical management, or investigation for complications such as pancreatitis or gallbladder disease.
What to Avoid: Supplement Interactions with Mounjaro
Whilst Mounjaro has relatively few direct drug interactions compared to some other diabetes medications, patients should exercise caution with certain supplements and be aware of potential indirect effects on their treatment regimen. The most significant consideration relates to supplements that may affect blood glucose levels, as Mounjaro is prescribed specifically for glycaemic control in type 2 diabetes. Supplements marketed for blood sugar support, such as chromium, cinnamon, berberine, or alpha-lipoic acid, may theoretically enhance glucose-lowering effects, potentially increasing the risk of hypoglycaemia, particularly in patients taking concurrent insulin or sulfonylureas. Whilst Mounjaro alone carries a low intrinsic risk of hypoglycaemia due to its glucose-dependent mechanism, patients should discuss any glucose-modulating supplements with their healthcare provider and monitor blood glucose levels more frequently when starting such supplements.
Herbal supplements with stimulant properties or those marketed for weight loss should be approached with caution. Products containing ephedra (which is prohibited in the UK), bitter orange (synephrine), or high doses of caffeine may cause cardiovascular effects such as elevated heart rate or blood pressure, which could be concerning in patients with pre-existing cardiovascular conditions. Given that Mounjaro is often prescribed to patients with metabolic syndrome or cardiovascular risk factors, adding stimulant supplements may be inadvisable. Many 'weight loss' herbal products are unlicensed and potentially unsafe.
Patients should be aware that the delayed gastric emptying caused by Mounjaro affects the absorption of oral contraceptives. According to the MHRA Summary of Product Characteristics, additional contraceptive precautions (such as barrier methods or non-oral contraception) are recommended for 4 weeks after starting tirzepatide and for 4 weeks after each dose increase. Severe vomiting or diarrhoea from any cause may further affect contraceptive efficacy.
Patients taking warfarin should be cautious with supplements containing vitamin K (such as some multivitamins or green tea extracts), as these may affect anticoagulation control. Regular INR monitoring is advised if starting or changing supplement regimens.
The delayed gastric emptying caused by Mounjaro may also affect the absorption timing of other oral medications requiring precise timing or rapid absorption, such as levothyroxine for thyroid conditions. These should be taken as directed by the prescribing physician, typically on an empty stomach and separated from other supplements.
Before starting any new supplement regimen, patients should inform their GP or diabetes specialist nurse, particularly if they have multiple comorbidities or take several medications. The MHRA Yellow Card scheme (yellowcard.mhra.gov.uk) allows reporting of suspected side effects or interactions, contributing to ongoing medication safety surveillance. A cautious, individualised approach to supplementation, guided by clinical need rather than marketing claims, remains the most prudent strategy for patients taking Mounjaro.
Frequently Asked Questions
Do I need to take supplements whilst on Mounjaro?
Supplements are not routinely required for all Mounjaro patients. Focus on maintaining a balanced, nutrient-dense diet, with supplementation considered only when dietary intake is insufficient or specific deficiencies are identified through clinical assessment or blood tests.
Should I take vitamin B12 with Mounjaro?
Vitamin B12 supplementation should be based on testing rather than routine use. Patients taking metformin alongside Mounjaro or those experiencing fatigue or neurological symptoms should discuss B12 screening with their healthcare provider.
Can I take probiotics to help with Mounjaro side effects?
Probiotics are generally safe and may support digestive comfort, though evidence specifically for GLP-1/GIP receptor agonist-related symptoms is limited. Choose products with clearly stated strains and colony-forming units, and consult your healthcare provider if immunocompromised.
The health-related content published on this site is based on credible scientific sources and is periodically reviewed to ensure accuracy and relevance. Although we aim to reflect the most current medical knowledge, the material is meant for general education and awareness only.
The information on this site is not a substitute for professional medical advice. For any health concerns, please speak with a qualified medical professional. By using this information, you acknowledge responsibility for any decisions made and understand we are not liable for any consequences that may result.
Heading 1
Heading 2
Heading 3
Heading 4
Heading 5
Heading 6
Lorem ipsum dolor sit amet, consectetur adipiscing elit, sed do eiusmod tempor incididunt ut labore et dolore magna aliqua. Ut enim ad minim veniam, quis nostrud exercitation ullamco laboris nisi ut aliquip ex ea commodo consequat. Duis aute irure dolor in reprehenderit in voluptate velit esse cillum dolore eu fugiat nulla pariatur.
Block quote
Ordered list
- Item 1
- Item 2
- Item 3
Unordered list
- Item A
- Item B
- Item C
Bold text
Emphasis
Superscript
Subscript












