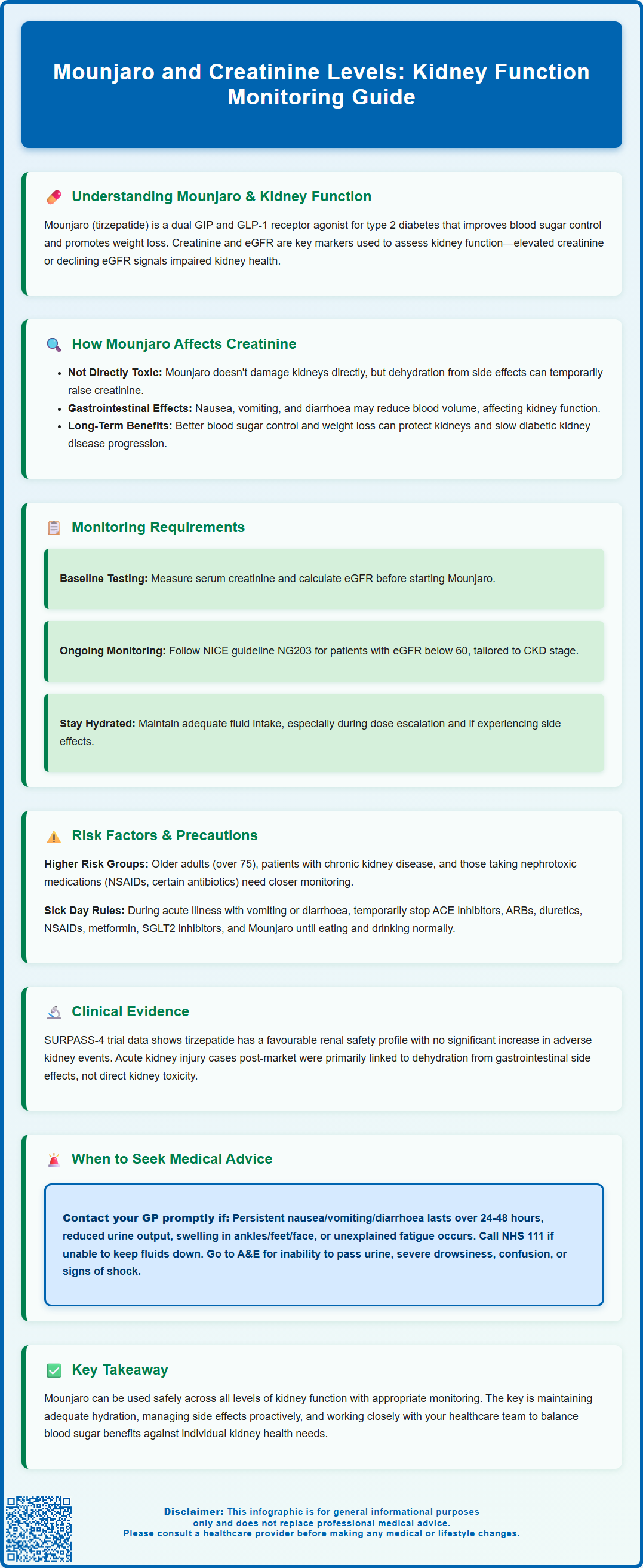
Mounjaro (tirzepatide) is a dual GIP and GLP-1 receptor agonist licensed in the UK for type 2 diabetes mellitus. Understanding the relationship between Mounjaro and creatinine levels is essential for safe prescribing and monitoring. Whilst tirzepatide is not directly nephrotoxic, gastrointestinal adverse effects—particularly nausea, vomiting, and diarrhoea—can lead to dehydration and transient rises in serum creatinine. This article examines how Mounjaro affects kidney function, monitoring requirements, risk factors, clinical evidence, and when to seek medical advice, ensuring healthcare professionals and patients can optimise treatment whilst safeguarding renal health.
Summary: Mounjaro (tirzepatide) does not directly damage the kidneys, but gastrointestinal side effects can cause dehydration leading to temporary rises in creatinine levels.
- Tirzepatide is a dual GIP/GLP-1 receptor agonist licensed for type 2 diabetes mellitus in the UK.
- Acute kidney injury has been reported post-marketing, mainly associated with dehydration from severe gastrointestinal adverse effects.
- No dose adjustment is required for renal impairment, but monitoring is advisable in patients with CKD experiencing severe gastrointestinal symptoms.
- Baseline serum creatinine and eGFR should be measured before initiating treatment, with repeat testing if clinical concerns arise.
- Patients should maintain adequate hydration and follow sick day rules during acute illness to prevent renal complications.
Table of Contents
- Understanding Mounjaro (Tirzepatide) and Kidney Function
- How Mounjaro May Affect Creatinine Levels
- Monitoring Kidney Function During Mounjaro Treatment
- Risk Factors and Precautions for Patients with Kidney Concerns
- Clinical Evidence on Mounjaro and Renal Safety
- When to Seek Medical Advice About Creatinine Changes
- Frequently Asked Questions
Understanding Mounjaro (Tirzepatide) and Kidney Function
Mounjaro (tirzepatide) is a dual glucose-dependent insulinotropic polypeptide (GIP) and glucagon-like peptide-1 (GLP-1) receptor agonist licensed in the UK for the treatment of type 2 diabetes mellitus. Approved by the Medicines and Healthcare products Regulatory Agency (MHRA) and recommended by NICE in technology appraisal guidance, Mounjaro works by enhancing insulin secretion in response to elevated blood glucose levels, suppressing glucagon release, and slowing gastric emptying (an effect that is most pronounced after initial doses and attenuates with continued use). These mechanisms collectively improve glycaemic control and may lead to weight loss.
Kidney function plays a vital role in maintaining overall metabolic health, particularly in patients with diabetes who face increased risk of diabetic nephropathy. Creatinine is a waste product generated from muscle metabolism and is filtered by the kidneys. Serum creatinine levels and estimated glomerular filtration rate (eGFR) are standard markers used to assess renal function. Elevated creatinine levels may indicate impaired kidney function, whilst a declining eGFR suggests progressive renal disease.
For patients prescribed Mounjaro, understanding the relationship between this medication and kidney function is essential. Whilst GLP-1 receptor agonists have generally demonstrated favourable renal outcomes in clinical trials, individual patient factors—such as pre-existing chronic kidney disease (CKD), dehydration, or concurrent nephrotoxic medications—can influence creatinine levels. Healthcare professionals must therefore consider baseline renal function and monitor patients appropriately throughout treatment to ensure both efficacy and safety.
How Mounjaro May Affect Creatinine Levels
Mounjaro's impact on creatinine levels is multifactorial and largely indirect. The medication itself is not directly nephrotoxic; however, acute kidney injury (AKI) has been reported in post-marketing surveillance, mainly associated with dehydration from severe gastrointestinal adverse effects. One of the most common adverse effects of Mounjaro is gastrointestinal disturbance, including nausea, vomiting, and diarrhoea, particularly during the initial titration phase. These symptoms can lead to dehydration and reduced intravascular volume, which may cause a rise in serum creatinine due to prerenal azotaemia.
Additionally, Mounjaro promotes weight loss and improved glycaemic control, both of which can have beneficial long-term effects on kidney health. Improved blood glucose levels reduce the risk of diabetic nephropathy progression, whilst weight reduction decreases glomerular hyperfiltration and intraglomerular pressure. However, rapid changes in body composition and fluid balance during the early treatment period may cause fluctuations in creatinine levels that require careful interpretation.
Patients with stable kidney function and adequate hydration typically experience fewer renal complications. Nevertheless, vigilance is warranted, particularly in vulnerable populations such as older adults or those with baseline CKD. Maintaining adequate hydration is essential, especially during the titration phase or if gastrointestinal side effects occur. Temporary interruption of treatment may be necessary during severe or prolonged gastrointestinal illness until hydration status and renal function can be reassessed.
Monitoring Kidney Function During Mounjaro Treatment
Baseline assessment of renal function is recommended before initiating Mounjaro therapy. This should include measurement of serum creatinine and calculation of eGFR using the CKD-EPI equation, which is the preferred method endorsed by NICE. According to the UK Summary of Product Characteristics (SmPC), no dose adjustment is required in patients with renal impairment, including those with end-stage renal disease. However, monitoring renal function is advisable in patients with renal impairment who experience severe gastrointestinal adverse effects.
During the titration phase, which typically involves dose escalation every four weeks, patients should be counselled about the importance of maintaining adequate hydration, especially if experiencing gastrointestinal side effects. Repeat renal function tests are not routinely required in patients with normal baseline kidney function unless clinical concerns arise. For individuals with pre-existing CKD, monitoring frequency should follow NICE guideline NG203 recommendations, tailored to their CKD stage and risk factors.
Key monitoring points include:
-
Serum creatinine and eGFR at baseline
-
Repeat testing if gastrointestinal symptoms are severe or persistent
-
Regular review in patients with eGFR <60 mL/min/1.73 m² as per NICE CKD guidance
-
Assessment of fluid status and hydration at each clinical encounter
Healthcare professionals should also review concomitant medications that may affect renal function, such as diuretics, ACE inhibitors, angiotensin receptor blockers (ARBs), SGLT2 inhibitors, and non-steroidal anti-inflammatory drugs (NSAIDs). Dose adjustments or temporary discontinuation of these agents may be necessary if signs of acute kidney injury develop.
Risk Factors and Precautions for Patients with Kidney Concerns
Certain patient groups are at higher risk of experiencing changes in creatinine levels whilst taking Mounjaro. Older adults, particularly those over 75 years, may have reduced renal reserve and are more susceptible to dehydration. Patients with established CKD require careful monitoring, especially if they experience severe gastrointestinal adverse effects.
Other important risk factors include:
-
Concurrent use of nephrotoxic medications: NSAIDs, certain antibiotics, and contrast agents can compound renal stress
-
Volume depletion: Patients on diuretics or with poor oral intake are at increased risk
-
Acute intercurrent illness: Conditions causing fever, vomiting, or diarrhoea can precipitate acute kidney injury (AKI)
-
Cardiovascular disease: Heart failure may impair renal perfusion
Precautionary measures should be implemented to minimise risk. Patients must be educated about the importance of adequate fluid intake, particularly during hot weather or illness. Gastrointestinal side effects should be managed proactively with antiemetics if necessary, and dose escalation may be slowed or paused if symptoms are severe.
Patients should follow UK 'sick day rules' during acute illness: temporarily pause medications that can worsen dehydration or impair renal function, including ACE inhibitors, ARBs, diuretics, NSAIDs, metformin, and SGLT2 inhibitors, until eating and drinking normally. Temporary discontinuation of Mounjaro is advisable during episodes of acute illness associated with dehydration.
If unable to maintain adequate hydration, patients should contact their GP or diabetes team promptly. NHS 111 should be contacted if unable to keep fluids down or if signs of AKI develop. Urgent medical care should be sought for red flag symptoms such as severe drowsiness, confusion, or inability to pass urine.
For patients with diabetic nephropathy, optimisation of blood pressure control and continuation of renoprotective agents such as ACE inhibitors or ARBs is essential when well. Regular monitoring by a multidisciplinary team, including input from nephrology services where appropriate, ensures comprehensive care and early detection of any renal deterioration.
Clinical Evidence on Mounjaro and Renal Safety
Clinical trial data from the SURPASS programme, which evaluated tirzepatide across multiple phase 3 studies, provide reassurance regarding renal safety. In the SURPASS-4 trial, which included patients with type 2 diabetes and increased cardiovascular risk, tirzepatide demonstrated a favourable renal safety profile with no significant increase in adverse renal events compared with insulin glargine. Improvements in glycaemic control and weight reduction observed with tirzepatide are associated with potential long-term renoprotective benefits, though definitive cardiovascular outcome trial data are still emerging.
Post-marketing surveillance and real-world evidence continue to support the general renal safety of GLP-1 receptor agonists, including tirzepatide. Systematic reviews of GLP-1 receptor agonists have found that these agents may reduce the risk of progression to macroalbuminuria and slow the decline in eGFR in patients with diabetic kidney disease. Whilst tirzepatide-specific long-term renal outcome trials are ongoing, extrapolation from the broader GLP-1 receptor agonist class suggests potential renoprotective effects.
However, it is important to acknowledge that acute kidney injury has been reported in post-marketing surveillance, predominantly in the context of severe gastrointestinal adverse effects leading to dehydration, as noted in the UK SmPC. The MHRA and European Medicines Agency (EMA) have highlighted the importance of monitoring renal function in at-risk patients and ensuring adequate hydration. These cases underscore the need for patient education and clinical vigilance rather than indicating direct nephrotoxicity.
Overall, the evidence supports the use of Mounjaro across all categories of renal function, with appropriate monitoring and precautions in place. The medication's benefits in improving glycaemic control must be balanced against individual patient factors and renal status.
Patients are encouraged to report any suspected adverse reactions to Mounjaro via the MHRA Yellow Card scheme.
When to Seek Medical Advice About Creatinine Changes
Patients taking Mounjaro should be aware of warning signs that may indicate changes in kidney function requiring medical attention. Whilst routine blood tests will detect asymptomatic rises in creatinine, certain symptoms warrant prompt evaluation. These include:
-
Persistent nausea, vomiting, or diarrhoea lasting more than 24–48 hours
-
Reduced urine output (passing less than 0.5 mL/kg/hour for more than 6 hours)
-
Swelling of the ankles, feet, or face (oedema)
-
Unexplained fatigue or confusion
-
Difficulty maintaining adequate fluid intake
Patients experiencing severe gastrointestinal symptoms should contact their GP or diabetes specialist nurse promptly. In some cases, temporary discontinuation of Mounjaro may be necessary until symptoms resolve and hydration status is restored. If dehydration is suspected, healthcare professionals should assess renal function and consider intravenous fluid replacement if oral rehydration is insufficient.
Healthcare professionals should arrange urgent renal function testing if there are signs of acute kidney injury (AKI) according to NICE guideline NG148 criteria:
-
Increase in serum creatinine of ≥26 µmol/L within 48 hours
-
Increase in serum creatinine to ≥1.5 times baseline within the previous 7 days
-
Urine output <0.5 mL/kg/hour for >6 hours
Patients should contact NHS 111 if they are unable to maintain hydration or have signs suggesting AKI. They should attend A&E if they become anuric (unable to pass urine), severely drowsy or confused, or show signs of shock.
For patients with pre-existing CKD, regular monitoring as per NICE guideline NG203 should continue alongside Mounjaro therapy. Any significant deterioration in renal function should prompt review by a nephrologist and consideration of alternative diabetes management strategies if necessary.
In summary, whilst Mounjaro can be used across all categories of renal function, awareness of potential risks, proactive monitoring, and patient education are essential to ensure optimal outcomes. Early recognition and management of dehydration or other precipitating factors can prevent serious renal complications and allow patients to benefit from this effective diabetes treatment.
Frequently Asked Questions
Does Mounjaro damage the kidneys?
Mounjaro (tirzepatide) is not directly nephrotoxic. However, gastrointestinal side effects such as nausea, vomiting, and diarrhoea can cause dehydration, which may lead to temporary increases in creatinine levels and, rarely, acute kidney injury if hydration is not maintained.
Do I need kidney function tests before starting Mounjaro?
Yes, baseline assessment of renal function is recommended before initiating Mounjaro therapy. This includes measurement of serum creatinine and calculation of eGFR to establish a baseline for monitoring throughout treatment.
Can I take Mounjaro if I have chronic kidney disease?
Yes, Mounjaro can be used across all stages of chronic kidney disease without dose adjustment. However, patients with CKD require careful monitoring, especially if experiencing severe gastrointestinal adverse effects, and should maintain adequate hydration throughout treatment.
The health-related content published on this site is based on credible scientific sources and is periodically reviewed to ensure accuracy and relevance. Although we aim to reflect the most current medical knowledge, the material is meant for general education and awareness only.
The information on this site is not a substitute for professional medical advice. For any health concerns, please speak with a qualified medical professional. By using this information, you acknowledge responsibility for any decisions made and understand we are not liable for any consequences that may result.
Heading 1
Heading 2
Heading 3
Heading 4
Heading 5
Heading 6
Lorem ipsum dolor sit amet, consectetur adipiscing elit, sed do eiusmod tempor incididunt ut labore et dolore magna aliqua. Ut enim ad minim veniam, quis nostrud exercitation ullamco laboris nisi ut aliquip ex ea commodo consequat. Duis aute irure dolor in reprehenderit in voluptate velit esse cillum dolore eu fugiat nulla pariatur.
Block quote
Ordered list
- Item 1
- Item 2
- Item 3
Unordered list
- Item A
- Item B
- Item C
Bold text
Emphasis
Superscript
Subscript