Missing your Ozempic injection can feel concerning, but understanding the correct steps to take helps you maintain effective diabetes management safely. Ozempic (semaglutide) is a once-weekly GLP-1 receptor agonist used for type 2 diabetes mellitus in the UK. The timing of when you remember your missed dose determines whether you should take it late or wait for your next scheduled injection. This guide explains the five-day rule, how missed doses affect blood glucose control, and practical strategies to prevent future lapses in adherence.
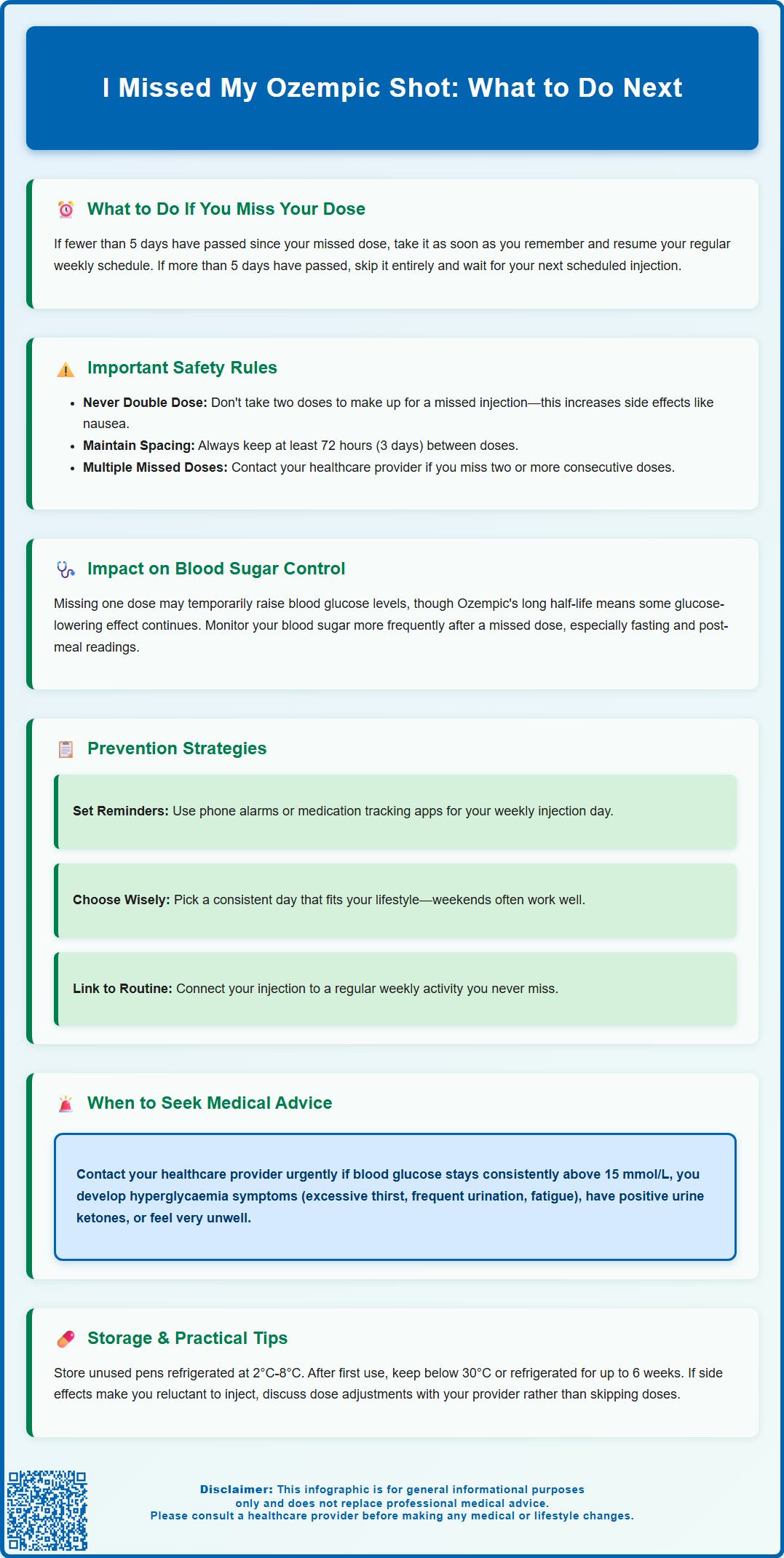
Summary: If you missed your Ozempic injection and fewer than five days have passed, take it as soon as you remember; if more than five days have elapsed, skip the missed dose and resume your regular weekly schedule.
- Ozempic (semaglutide) is a once-weekly GLP-1 receptor agonist injection for type 2 diabetes mellitus.
- The medication has a one-week half-life, providing extended therapeutic action and some flexibility with missed doses.
- Never double your dose to compensate for a missed injection, and ensure at least 72 hours between any two doses.
- A single missed dose may cause temporary blood glucose elevation, though the extent varies between individuals.
- Contact your GP urgently if blood glucose remains consistently above 15 mmol/L or you develop symptoms of hyperglycaemia.
- Repeatedly missing doses may require restarting at a lower dose under healthcare provider supervision.
Table of Contents
What to Do If You Miss Your Ozempic Dose
Missing a dose of Ozempic (semaglutide) is not uncommon, and knowing how to respond appropriately can help you maintain effective diabetes management without unnecessary anxiety. Ozempic is a once-weekly subcutaneous injection used primarily for type 2 diabetes mellitus. Semaglutide is also available as Wegovy, which is the licensed product specifically for weight management in the UK. Ozempic belongs to the glucagon-like peptide-1 (GLP-1) receptor agonist class, which works by enhancing insulin secretion in response to meals, suppressing glucagon release, and slowing gastric emptying.
If you realise you have missed your scheduled injection, the timing of when you remember is crucial to determining your next step. According to the manufacturer's guidance and MHRA-approved prescribing information, if fewer than five days have passed since your missed dose, you should administer the injection as soon as you remember. You should then return to your regular weekly schedule from your original injection day.
If more than five days have elapsed since your missed dose, you should skip the missed injection entirely and wait until your next regularly scheduled dose day. Taking the injection after this window could result in receiving two doses too close together, potentially increasing the risk of adverse effects such as nausea or vomiting. If you decide to change your regular injection day, always ensure there are at least 3 days (72 hours) between doses. Never attempt to double your dose to compensate for the missed injection.
Practical steps to prevent future missed doses include setting mobile phone reminders, using a medication tracking app, or linking your injection day to a specific weekly activity. If you frequently struggle with adherence, discuss this openly with your GP or diabetes specialist nurse, as they may suggest strategies tailored to your lifestyle or consider whether alternative treatment regimens might be more suitable for your circumstances.
How Long Can You Safely Delay an Ozempic Injection?
Understanding the pharmacokinetic properties of Ozempic helps clarify why specific timing recommendations exist for missed doses. Semaglutide has a half-life of approximately one week, which means the medication remains active in your system for an extended period after each injection. This prolonged duration of action provides some flexibility when doses are missed, but also necessitates careful timing to avoid overlapping therapeutic effects.
The five-day window represents the critical threshold for decision-making when you miss an Ozempic dose, as stated in the official Summary of Product Characteristics (SmPC). Within this timeframe, administering the missed dose maintains relatively consistent drug levels and preserves the medication's glucose-lowering effects. The once-weekly dosing schedule is designed to achieve steady-state concentrations, and minor delays within five days typically do not significantly disrupt this equilibrium. However, as you approach and exceed this five-day mark, the risk-benefit balance shifts, and it becomes safer to wait for your next scheduled dose rather than risk having two injections too close together.
Delaying beyond five days without taking action means you should simply resume with your next planned injection on the original schedule. While this creates a longer gap than usual between doses, it is the recommended approach to prevent potential adverse effects. During this extended interval, you may experience some reduction in glycaemic control, though the medication's long half-life means you will still have some circulating semaglutide providing therapeutic benefit.
It is important to note that repeatedly missing doses or frequently delaying injections can compromise the overall effectiveness of your diabetes management plan. If you miss two or more consecutive doses, contact your healthcare provider as you may need to restart at a lower dose and gradually increase again. If you find yourself regularly unable to adhere to the weekly schedule, this should prompt a conversation with your healthcare provider about potential barriers to adherence, whether practical, psychological, or related to side effects that may be making you reluctant to continue treatment as prescribed.
Will Missing Ozempic Affect Your Blood Sugar Control?
The impact of a missed Ozempic dose on blood glucose levels varies depending on individual factors, including your overall diabetes control, concurrent medications, diet, and physical activity levels. Ozempic works through multiple mechanisms to lower blood glucose: it stimulates insulin secretion in a glucose-dependent manner, reduces inappropriate glucagon secretion, and slows gastric emptying, all of which contribute to improved glycaemic control throughout the day and particularly after meals.
A single missed dose may cause a temporary rise in blood glucose readings, though the extent of this increase differs considerably between individuals. Some patients may notice minimal change, particularly if their diabetes is well-controlled and they are taking other glucose-lowering medications such as metformin. Others might observe more pronounced elevations in their home blood glucose monitoring results, especially in the fasting state or after carbohydrate-rich meals. The medication's long half-life means that some therapeutic effect persists even after missing one weekly dose, providing a degree of metabolic protection.
If you are monitoring your blood glucose at home, you may wish to check more frequently during the period when you have missed your dose, particularly if you typically experience significant glucose fluctuations. This information can be valuable for your healthcare team and helps you understand your individual response. However, there is no need for alarm if readings are slightly elevated; this is an expected physiological response to reduced medication levels and should normalise once you resume your regular dosing schedule.
Contact your GP or diabetes specialist nurse urgently if you experience persistently high blood glucose readings (consistently above 15 mmol/L), symptoms of hyperglycaemia such as excessive thirst, frequent urination, or unexplained fatigue, or if you have positive ketones in your urine. Seek same-day medical advice if you cannot keep fluids down or feel very unwell. It's worth noting that hypoglycaemia (low blood sugar) is uncommon with Ozempic alone, but the risk increases if you also take insulin or sulfonylurea medications. If you take these medications alongside Ozempic, discuss with your healthcare provider how to manage them when you miss an Ozempic dose.
Getting Back on Track with Your Ozempic Schedule
Re-establishing your regular Ozempic routine after a missed dose requires a clear understanding of when to administer your next injection and how to prevent future lapses in adherence. Once you have either taken the missed dose (if within five days) or skipped it (if beyond five days), the key is to return to your original day of the week for subsequent injections. If you need to change your weekly injection day, always ensure there are at least 3 days (72 hours) between doses. This consistency helps maintain stable drug levels and makes the routine easier to remember long-term.
Practical strategies to improve medication adherence include choosing an injection day that aligns with your weekly schedule and is least likely to be disrupted by travel, work commitments, or social activities. Many patients find that weekend days work well, as they allow time to manage any injection-related side effects such as mild nausea without work pressures. Store your Ozempic pen correctly: before first use, keep refrigerated (2°C to 8°C); after first use, you can store it either below 30°C or in a refrigerator for up to 6 weeks. Always keep the pen cap on when not in use, do not store with a needle attached, protect from light, and never freeze the medication. Use a proper sharps bin for needle disposal, which you can obtain from your GP surgery or pharmacy.
If you are experiencing side effects that make you reluctant to continue treatment, such as persistent nausea, vomiting, or gastrointestinal discomfort, discuss these openly with your healthcare provider rather than simply missing doses. These adverse effects often improve with time or can be managed through dose adjustments, dietary modifications, or symptomatic treatment. Your prescriber may recommend a slower dose escalation schedule or suggest taking the injection at a different time of day to minimise discomfort.
For patients who frequently miss doses despite good intentions, it may be worth exploring whether there are underlying concerns about the medication, practical barriers to administration, or whether an alternative treatment approach might be more suitable. NICE recommends a patient-centred approach to diabetes management, and your healthcare team should work collaboratively with you to find a regimen that is both clinically effective and practically sustainable. Remember that consistent adherence to your prescribed treatment plan is essential for achieving optimal glycaemic control and reducing the long-term complications associated with type 2 diabetes mellitus. If you experience any suspected side effects from Ozempic, report them through the MHRA Yellow Card Scheme.
Frequently Asked Questions
Can I take two Ozempic injections in one week if I missed a dose?
No, you should never take two Ozempic injections close together. If more than five days have passed since your missed dose, skip it entirely and wait for your next regularly scheduled injection day. Always ensure at least 72 hours between any two doses.
Will my blood sugar spike if I miss one Ozempic injection?
You may experience a temporary rise in blood glucose levels, though the extent varies between individuals. Ozempic's long half-life means some therapeutic effect persists even after missing one dose, providing continued metabolic protection.
Do I need to restart Ozempic at a lower dose after missing injections?
If you miss two or more consecutive doses, contact your healthcare provider as you may need to restart at a lower dose and gradually increase again. A single missed dose typically does not require dose adjustment when resuming your regular schedule.
The health-related content published on this site is based on credible scientific sources and is periodically reviewed to ensure accuracy and relevance. Although we aim to reflect the most current medical knowledge, the material is meant for general education and awareness only.
The information on this site is not a substitute for professional medical advice. For any health concerns, please speak with a qualified medical professional. By using this information, you acknowledge responsibility for any decisions made and understand we are not liable for any consequences that may result.
Heading 1
Heading 2
Heading 3
Heading 4
Heading 5
Heading 6
Lorem ipsum dolor sit amet, consectetur adipiscing elit, sed do eiusmod tempor incididunt ut labore et dolore magna aliqua. Ut enim ad minim veniam, quis nostrud exercitation ullamco laboris nisi ut aliquip ex ea commodo consequat. Duis aute irure dolor in reprehenderit in voluptate velit esse cillum dolore eu fugiat nulla pariatur.
Block quote
Ordered list
- Item 1
- Item 2
- Item 3
Unordered list
- Item A
- Item B
- Item C
Bold text
Emphasis
Superscript
Subscript