Saxenda (liraglutide 3.0 mg) is a GLP-1 receptor agonist licensed by the MHRA for weight management in adults and adolescents meeting specific criteria. Whilst the medication enhances satiety and reduces appetite, choosing the best foods to eat on Saxenda is crucial for achieving optimal outcomes. Because patients typically consume smaller portions, every meal must be nutrient-dense to meet daily requirements for protein, fibre, vitamins, and minerals. This article explores evidence-based dietary strategies that complement Saxenda's mechanism of action, support sustainable weight loss, and minimise common gastrointestinal side effects whilst maintaining overall health and wellbeing throughout treatment.
Summary: The best foods to eat on Saxenda include high-protein sources (lean meats, fish, eggs, legumes), fibre-rich wholegrains, vegetables, fruits, and adequate hydration to support weight loss whilst maintaining nutrition and minimising side effects.
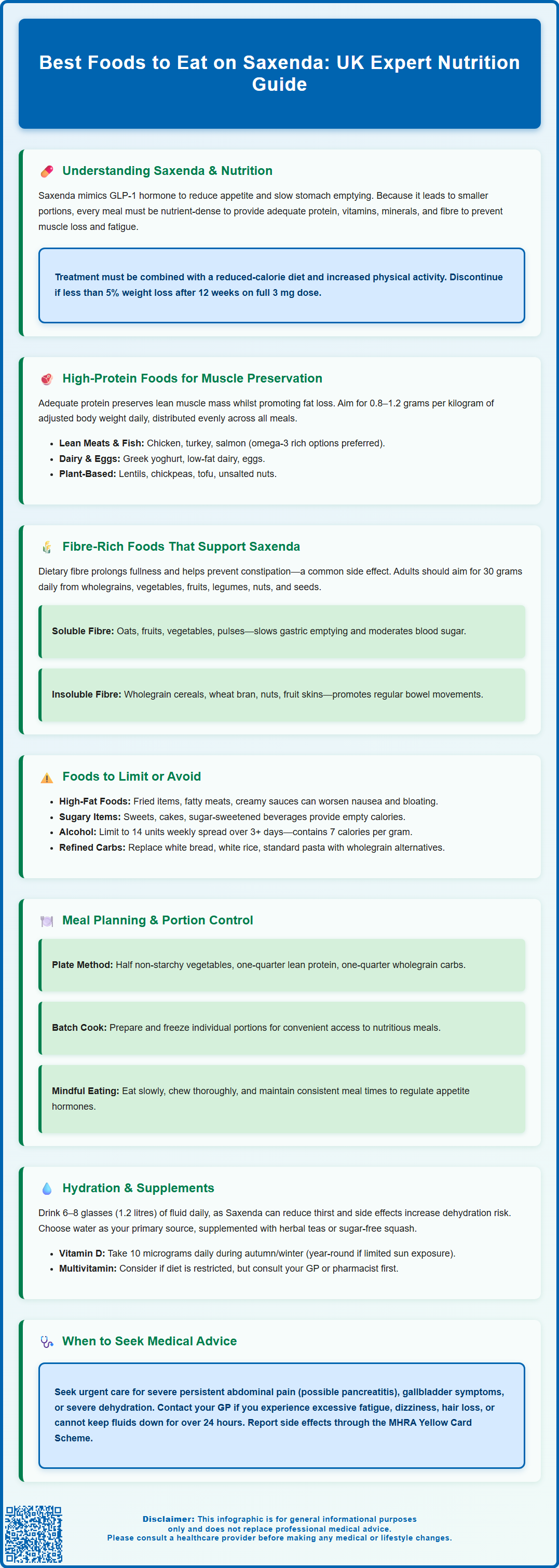
- Saxenda (liraglutide) is a GLP-1 receptor agonist that slows gastric emptying and enhances satiety, requiring nutrient-dense food choices due to reduced portion sizes.
- High-quality protein (0.8–1.2 g/kg daily) from lean meats, fish, eggs, dairy, and plant sources preserves muscle mass during weight loss.
- Fibre-rich foods (targeting 30 g daily) including wholegrains, vegetables, fruits, and legumes support digestive health and complement Saxenda's satiety effects.
- Foods high in saturated fat, refined sugars, and alcohol should be limited as they may worsen gastrointestinal side effects and undermine weight loss efforts.
- Adequate hydration (6–8 glasses daily) is essential, particularly as nausea, vomiting, or diarrhoea can increase dehydration risk during Saxenda therapy.
Table of Contents
- Understanding Saxenda and Nutritional Requirements
- High-Protein Foods to Support Weight Loss on Saxenda
- Fibre-Rich Foods That Complement Saxenda Treatment
- Foods to Limit or Avoid While Taking Saxenda
- Meal Planning and Portion Control Strategies
- Hydration and Nutritional Supplements During Saxenda Therapy
- Frequently Asked Questions
Understanding Saxenda and Nutritional Requirements
Saxenda (liraglutide 3.0 mg) is a glucagon-like peptide-1 (GLP-1) receptor agonist licensed by the MHRA for weight management in adults with a body mass index (BMI) of 30 kg/m² or greater, or 27 kg/m² or greater in the presence of weight-related comorbidities such as prediabetes, type 2 diabetes, hypertension, dyslipidaemia or obstructive sleep apnoea. It is also licensed for weight management in adolescents aged 12-<18 years with body weight above 60 kg and obesity (specific criteria are detailed in the SmPC).
The medication works by mimicking the action of the naturally occurring hormone GLP-1, which regulates appetite and food intake by slowing gastric emptying, enhancing satiety signals to the brain, and reducing hunger between meals.
When prescribed Saxenda, patients must understand that the medication is not a standalone solution but rather an adjunct to a comprehensive weight management programme. NICE Technology Appraisal (TA664) emphasises that pharmacological interventions should be combined with a reduced-calorie diet and increased physical activity for optimal outcomes. Treatment should be discontinued if at least 5% weight loss has not been achieved after 12 weeks on the full 3 mg daily dose.
Nutritional requirements during Saxenda therapy remain fundamentally unchanged from general healthy eating principles, but the quality and composition of food choices become particularly important. Because patients typically consume smaller portions due to enhanced satiety, every meal must be nutrient-dense to meet daily requirements for essential vitamins, minerals, protein, and fibre. Inadequate nutrition can lead to muscle loss, fatigue, and other adverse health outcomes that may compromise the benefits of weight reduction.
Patients should ideally work with a registered dietitian or healthcare professional to develop an individualised eating plan that accounts for their specific health conditions, medication regimen, and weight loss goals. This collaborative approach ensures that dietary modifications support both the pharmacological action of Saxenda and the patient's overall health and wellbeing throughout the treatment period.
Important safety note: Patients should seek urgent medical attention if they experience severe, persistent abdominal pain (especially if radiating to the back) which could indicate pancreatitis, symptoms of gallbladder disease, or signs of severe dehydration. Suspected side effects should be reported via the MHRA Yellow Card Scheme.
High-Protein Foods to Support Weight Loss on Saxenda
Adequate protein intake is essential during Saxenda therapy to preserve lean muscle mass whilst promoting fat loss. Protein has the highest thermic effect of all macronutrients, meaning the body expends more energy digesting it, and it provides superior satiety compared to carbohydrates or fats. This complementary effect works synergistically with Saxenda's appetite-suppressing mechanism to help patients feel satisfied with smaller portions.
Recommended high-quality protein sources include:
-
Lean meats and poultry: Skinless chicken breast, turkey, lean cuts of beef and pork (trimmed of visible fat)
-
Fish and seafood: Salmon, mackerel, sardines (rich in omega-3 fatty acids), white fish such as cod and haddock, prawns
-
Eggs: A complete protein source providing all essential amino acids, versatile and economical
-
Dairy products: Greek yoghurt, cottage cheese, skimmed or semi-skimmed milk, reduced-fat cheese
-
Plant-based proteins: Lentils, chickpeas, black beans, tofu, tempeh, edamame beans, quinoa
Protein requirements during weight loss typically range from approximately 0.8–1.2 grams of protein per kilogram of adjusted body weight daily, though individual needs vary based on age, activity level, and existing muscle mass. Patients with chronic kidney disease should discuss appropriate protein intake with their GP or dietitian, as higher protein levels may not be suitable for them.
Distributing protein intake across all meals, rather than concentrating it in one sitting, optimises muscle protein synthesis and helps maintain satiety throughout the day.
Practical implementation might involve including a palm-sized portion of protein with each main meal and incorporating protein-rich snacks such as a small handful of unsalted nuts, a boiled egg, or a pot of Greek yoghurt. Patients who struggle to meet protein requirements through food alone may benefit from discussing protein supplementation with their healthcare provider, though whole food sources are generally preferable as they provide additional nutrients and fibre.
Fibre-Rich Foods That Complement Saxenda Treatment
Dietary fibre plays a crucial role in supporting the therapeutic effects of Saxenda whilst promoting digestive health and glycaemic control. Fibre slows the absorption of nutrients, prolongs feelings of fullness, and helps regulate bowel function—particularly important as gastrointestinal side effects such as constipation are commonly reported with GLP-1 receptor agonists. The NHS recommends adults consume approximately 30 grams of fibre daily, a target that becomes especially relevant during weight management therapy.
Soluble fibre, found in oats, barley, fruits, vegetables, and pulses, forms a gel-like substance in the digestive tract that slows gastric emptying and helps moderate blood sugar spikes after meals. This mechanism complements Saxenda's own effect on gastric motility. Insoluble fibre, present in wholegrain cereals, wheat bran, nuts, and the skins of fruits and vegetables, adds bulk to stools and promotes regular bowel movements, potentially mitigating constipation associated with the medication.
Excellent fibre-rich food choices include:
-
Wholegrains: Porridge oats, brown rice, wholemeal bread, wholewheat pasta, bulgur wheat, pearl barley
-
Vegetables: Broccoli, Brussels sprouts, carrots, sweet potatoes (with skin), leafy greens, peas
-
Fruits: Apples and pears (with skin), berries, oranges, bananas
-
Legumes: All varieties of beans, lentils, and chickpeas—these provide both fibre and protein
-
Nuts and seeds: Almonds, chia seeds, flaxseeds, pumpkin seeds
Incorporating a variety of these foods also helps meet the NHS '5 A Day' recommendation for fruit and vegetable consumption.
Gradual introduction of fibre is advisable to allow the digestive system to adapt and minimise bloating or discomfort. Patients should increase fibre intake slowly over several weeks whilst ensuring adequate fluid consumption, as fibre requires water to function effectively. Those experiencing persistent constipation despite adequate fibre and fluid intake should consult their GP or prescribing clinician, as dose adjustment or additional management strategies may be necessary.
Foods to Limit or Avoid While Taking Saxenda
Whilst no foods are strictly prohibited during Saxenda therapy, certain dietary choices can undermine treatment effectiveness or exacerbate common side effects. The medication's mechanism of slowing gastric emptying means that high-fat, heavily processed, or very rich foods may worsen nausea, bloating, and indigestion—adverse effects reported by a significant proportion of patients, particularly during dose escalation phases.
Foods that warrant limitation include:
-
Foods high in saturated fat: Deep-fried items, fatty cuts of meat, full-fat dairy products, pastries, and creamy sauces can delay gastric emptying further and trigger or worsen nausea
-
Foods high in salt and free sugars: Items with minimal nutritional value whilst contributing excess calories that counteract weight loss efforts
-
Sugary foods and beverages: Sweets, biscuits, cakes, sugar-sweetened drinks, and fruit juices cause rapid blood glucose fluctuations and provide empty calories
-
Alcohol: Contains 7 calories per gram with no nutritional benefit, may impair judgement regarding food choices, and can affect blood glucose control. The UK Chief Medical Officers advise no more than 14 units per week, spread over 3 or more days with several alcohol-free days. It's particularly important to avoid alcohol during significant gastrointestinal side effects or when at risk of dehydration
-
Large portion sizes: Even of healthy foods, as overeating can cause significant discomfort given Saxenda's effect on gastric emptying
Refined carbohydrates such as white bread, white rice, and standard pasta should be replaced with wholegrain alternatives that provide better satiety and nutritional value. Highly spicy or acidic foods may aggravate gastrointestinal symptoms in sensitive individuals, though there is no official link requiring universal avoidance.
It is important to emphasise that occasional consumption of less optimal foods within an overall balanced diet is acceptable and may support long-term adherence to healthy eating patterns. Overly restrictive approaches can lead to feelings of deprivation and potentially trigger disordered eating behaviours. The focus should remain on establishing sustainable, nutritious eating habits that can be maintained beyond the treatment period, rather than adhering to rigid dietary rules that prove difficult to sustain.
Meal Planning and Portion Control Strategies
Effective meal planning is fundamental to maximising Saxenda's therapeutic benefits whilst ensuring adequate nutrition despite reduced appetite and smaller portion sizes. Structured planning helps patients make intentional food choices, reduces reliance on convenience foods, and ensures balanced macronutrient distribution throughout the day. Given that Saxenda enhances satiety signals, patients often find they require significantly less food than previously, making the quality of each meal paramount.
Practical meal planning strategies include:
-
The plate method: Fill half the plate with non-starchy vegetables, one-quarter with lean protein, and one-quarter with wholegrain carbohydrates—this visual guide ensures balanced nutrition without complex calculations
-
Batch cooking: Preparing multiple portions of healthy meals when energy levels are good, then freezing individual servings for convenient access
-
Regular meal timing: Eating at consistent times helps regulate appetite hormones and prevents excessive hunger that might lead to poor food choices
-
Mindful eating practices: Eating slowly, chewing thoroughly, and paying attention to satiety signals—particularly important as Saxenda affects the rate of gastric emptying
Portion control becomes naturally easier with Saxenda due to enhanced fullness, but patients should remain mindful of minimum nutritional requirements. Using smaller plates and bowls can help portions appear more substantial, whilst measuring tools or visual guides (such as comparing portions to everyday objects) support appropriate serving sizes without obsessive weighing.
Meal frequency may need adjustment based on individual response to the medication. Some patients thrive on three moderate meals daily, whilst others prefer smaller, more frequent eating occasions. There is no official link between specific meal timing patterns and superior outcomes—the optimal approach is one that the patient finds sustainable and that meets their nutritional needs.
Patients experiencing significant appetite suppression should prioritise nutrient-dense foods at each eating occasion and consider whether they are meeting minimum calorie requirements. The NHS advises that a safe rate of weight loss is about 0.5-1 kg per week after the initial period. Excessively rapid weight loss, symptoms such as fatigue, dizziness, or hair loss may indicate inadequate nutrition and warrant discussion with a healthcare professional. If unable to keep fluids down for more than 24 hours, experiencing worsening vomiting, dizziness or fainting, patients should contact their GP or NHS 111; their prescriber may advise temporarily holding the medication.
Hydration and Nutritional Supplements During Saxenda Therapy
Adequate hydration is essential during Saxenda treatment, particularly as gastrointestinal side effects such as nausea, vomiting, and diarrhoea can increase fluid losses and risk of dehydration. The medication's effect on appetite may also reduce the natural drive to drink, making conscious fluid intake especially important. The NHS recommends approximately 6–8 glasses (1.2 litres) of fluid daily, though individual requirements vary based on body size, activity level, climate, and the presence of fluid-losing conditions.
Optimal hydration choices include:
-
Water: The best choice for hydration without added calories, sugars, or artificial ingredients
-
Herbal and fruit teas: Provide variety without caffeine or calories (unsweetened)
-
Diluted sugar-free squash: Can make water more palatable for those who struggle with plain water
-
Milk: Contributes to both fluid and calcium intake (choose lower-fat options)
Caffeinated drinks such as tea and coffee do contribute to daily fluid intake, though moderation is advised (no more than 400 mg caffeine daily, equivalent to about four cups of coffee) if they affect sleep or anxiety. Alcohol should be minimised both for its caloric content and its potential to impair judgement regarding food choices and medication adherence. The UK Chief Medical Officers advise no more than 14 units of alcohol per week, spread over 3 or more days with several alcohol-free days.
Nutritional supplementation may be appropriate for some patients, particularly those with restricted dietary intake or specific deficiencies. A daily multivitamin and mineral supplement can provide insurance against micronutrient gaps, though it should not replace a varied, balanced diet. Patients following very low-calorie diets (under medical supervision) or those with malabsorption conditions may require specific supplementation protocols.
Vitamin D supplementation of 10 micrograms (400 IU) daily is recommended for all UK adults during autumn and winter months, as per UK government and NHS guidance. Some groups, including those with limited sun exposure or darker skin, may need year-round supplementation. Calcium intake should be monitored, especially in patients avoiding dairy products, as adequate calcium is essential for bone health during weight loss.
People with type 2 diabetes who are taking insulin or sulfonylureas should monitor for hypoglycaemia and discuss medication adjustments with their clinician if their appetite or food intake is significantly reduced.
Patients should consult their GP or pharmacist before starting any supplements, as some may interact with medications or be contraindicated in certain health conditions. Signs of dehydration (dark urine, dizziness, dry mouth, reduced urination) or suspected nutritional deficiencies (unusual fatigue, weakness, changes in skin or hair) warrant prompt medical review to ensure safe and effective treatment outcomes.
Frequently Asked Questions
What protein foods should I eat whilst taking Saxenda?
Prioritise lean meats (chicken, turkey), fish (salmon, cod), eggs, Greek yoghurt, cottage cheese, and plant-based options such as lentils, chickpeas, and tofu. Aim for approximately 0.8–1.2 grams of protein per kilogram of body weight daily, distributed across meals to preserve muscle mass during weight loss.
Should I avoid any specific foods whilst on Saxenda?
No foods are strictly prohibited, but limit high-fat, heavily processed, and sugary foods that may worsen nausea and gastrointestinal side effects. Reduce alcohol consumption and replace refined carbohydrates with wholegrain alternatives for better satiety and nutritional value.
How much water should I drink on Saxenda?
Aim for approximately 6–8 glasses (1.2 litres) of fluid daily, primarily water, herbal teas, or diluted sugar-free squash. Adequate hydration is particularly important as gastrointestinal side effects such as nausea, vomiting, or diarrhoea can increase dehydration risk during Saxenda treatment.
The health-related content published on this site is based on credible scientific sources and is periodically reviewed to ensure accuracy and relevance. Although we aim to reflect the most current medical knowledge, the material is meant for general education and awareness only.
The information on this site is not a substitute for professional medical advice. For any health concerns, please speak with a qualified medical professional. By using this information, you acknowledge responsibility for any decisions made and understand we are not liable for any consequences that may result.
Heading 1
Heading 2
Heading 3
Heading 4
Heading 5
Heading 6
Lorem ipsum dolor sit amet, consectetur adipiscing elit, sed do eiusmod tempor incididunt ut labore et dolore magna aliqua. Ut enim ad minim veniam, quis nostrud exercitation ullamco laboris nisi ut aliquip ex ea commodo consequat. Duis aute irure dolor in reprehenderit in voluptate velit esse cillum dolore eu fugiat nulla pariatur.
Block quote
Ordered list
- Item 1
- Item 2
- Item 3
Unordered list
- Item A
- Item B
- Item C
Bold text
Emphasis
Superscript
Subscript