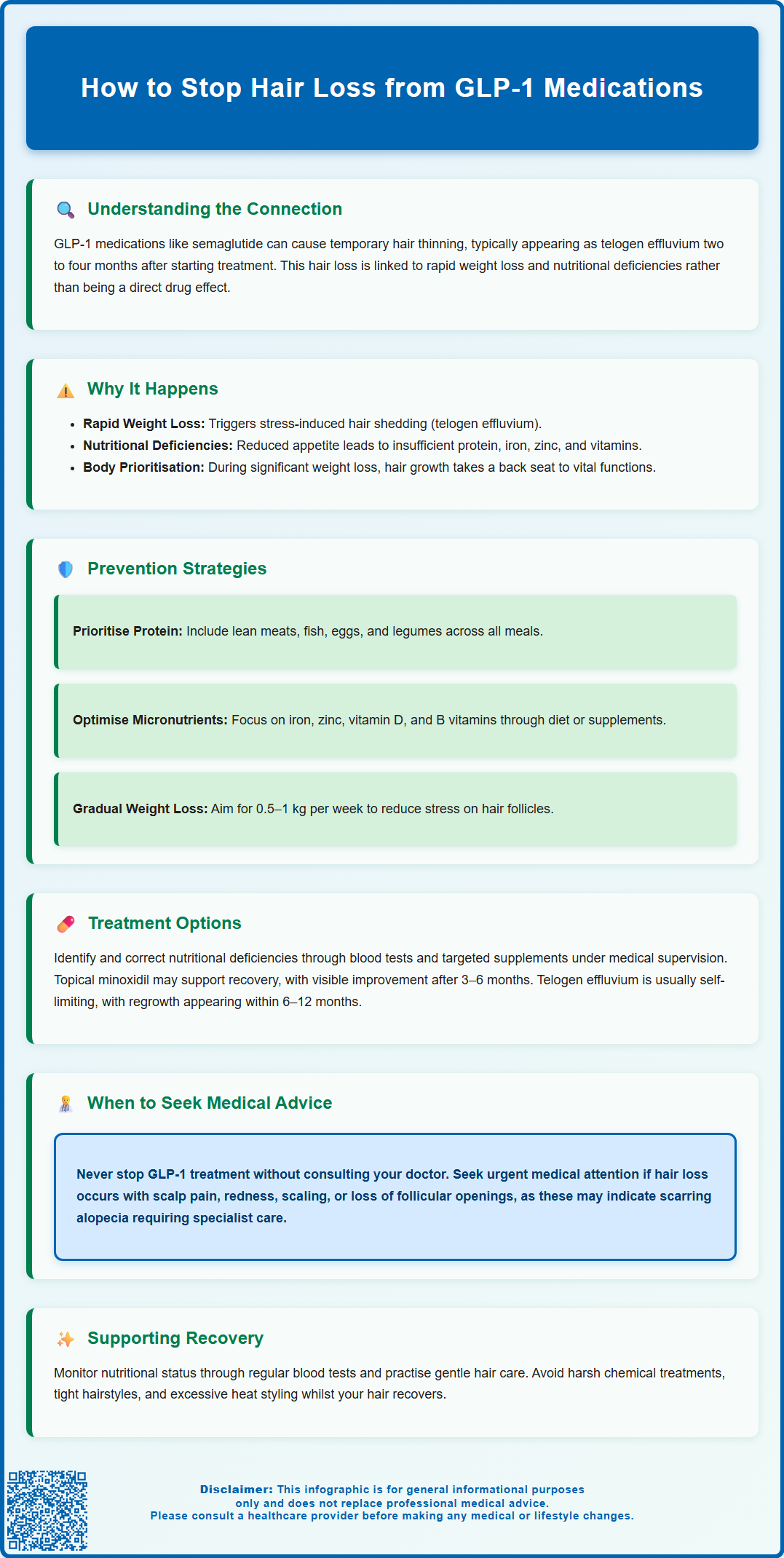
Hair thinning whilst taking GLP-1 receptor agonists such as semaglutide (Ozempic, Wegovy) or liraglutide (Saxenda) can be distressing, though it is typically temporary and manageable. This hair loss, often presenting as telogen effluvium, usually results from rapid weight reduction and nutritional changes rather than direct drug effects. Understanding the underlying mechanisms and implementing preventative strategies—including optimising protein and micronutrient intake—can significantly reduce risk. This article provides evidence-based guidance on preventing and managing hair loss during GLP-1 treatment, helping patients maintain both metabolic health and hair quality.
Summary: Hair loss from GLP-1 medications is typically temporary telogen effluvium caused by rapid weight loss and nutritional changes, manageable through adequate protein intake, micronutrient optimisation, and moderating weight reduction rate.
- GLP-1-related hair loss usually manifests as telogen effluvium 2–4 months after starting treatment or significant weight loss.
- The mechanism is indirect, primarily driven by rapid weight reduction and nutritional deficiencies rather than direct drug effects.
- Prevention requires adequate protein intake, micronutrient optimisation (iron, zinc, vitamin D, B vitamins), and gradual weight loss of 0.5–1 kg weekly.
- Treatment includes correcting identified nutritional deficiencies through supplementation and, in some cases, topical minoxidil.
- Hair regrowth typically occurs within 3–6 months once nutritional status improves and weight loss stabilises.
- Patients should seek urgent medical advice if hair loss is accompanied by scalp pain, redness, scaling, or complete bald patches.
Table of Contents
Understanding Hair Loss with GLP-1 Medications
GLP-1 receptor agonists — including semaglutide (Ozempic, Wegovy), liraglutide (Saxenda, Victoza), and dulaglutide (Trulicity) — have become widely prescribed for type 2 diabetes management and weight loss. Whilst these medications are generally well-tolerated, some patients report experiencing hair thinning or increased shedding during treatment. It's important to note that hair loss (alopecia) is listed as an adverse reaction in the Summary of Product Characteristics (SmPC) for semaglutide 2.4 mg (Wegovy), though it is not listed as a common side effect for other GLP-1 medications such as Ozempic, Saxenda, or Trulicity.
Clinical observations suggest the hair loss typically manifests as telogen effluvium — a form of diffuse hair shedding that occurs when a significant number of hair follicles enter the resting (telogen) phase prematurely. This condition is usually temporary and reversible, though it can be distressing for patients. The shedding often becomes noticeable two to four months after starting treatment or after significant weight loss, which is a key distinguishing feature.
Understanding the context is essential for both patients and healthcare professionals. Hair loss associated with GLP-1 medications appears to be multifactorial rather than a direct drug effect. Factors such as rapid weight reduction, caloric restriction, nutritional deficiencies, and metabolic changes all play contributory roles. Initial investigations for diffuse hair loss should include full blood count, ferritin, thyroid function tests, vitamin B12, folate, and vitamin D levels to rule out common underlying causes. Patients experiencing hair thinning should be encouraged to discuss their concerns with their GP or prescribing clinician rather than discontinuing treatment abruptly, as the underlying condition being treated (diabetes or obesity) requires ongoing management. Any suspected adverse drug reactions should be reported via the MHRA Yellow Card scheme (yellowcard.mhra.gov.uk).
Why GLP-1 Treatments May Cause Hair Thinning
The mechanism behind hair loss in patients taking GLP-1 medications is not directly related to the drug's pharmacological action on GLP-1 receptors. Instead, it appears to be an indirect consequence of the metabolic and physiological changes that occur during treatment. The most significant factor is rapid weight loss, which is a well-established trigger for telogen effluvium. When the body experiences sudden weight reduction, it can interpret this as physiological stress, prompting hair follicles to shift prematurely into the resting phase.
Nutritional deficiencies represent another important mechanism. Patients taking GLP-1 agonists often experience reduced appetite and early satiety, which are therapeutic effects of the medication. However, this can lead to inadequate intake of essential nutrients required for healthy hair growth, including protein, iron, zinc, and vitamins B12 and D. Hair follicles are metabolically active structures with high nutritional demands, and deficiencies in these micronutrients can compromise the hair growth cycle. Additionally, the caloric restriction associated with weight loss may result in insufficient protein intake, depriving hair follicles of the amino acids needed for keratin synthesis.
Metabolic changes during significant weight loss may also contribute. The body's adaptive response to caloric restriction may prioritise essential physiological functions over non-essential processes like hair growth. It is worth noting that telogen effluvium can occur with any form of rapid weight loss, whether achieved through medication, bariatric surgery, or restrictive dieting. This suggests that the hair loss is primarily a consequence of the weight reduction itself rather than a specific drug effect.
Importantly, other medical conditions can cause similar patterns of hair loss, particularly hypothyroidism and iron deficiency, which should be excluded through appropriate testing. Understanding these mechanisms helps clinicians provide appropriate counselling and implement preventative strategies.
How to Prevent Hair Loss While Taking GLP-1
Preventing hair loss whilst taking GLP-1 medications requires a proactive, multifaceted approach focused on optimising nutrition and moderating the rate of weight loss. The most important strategy is ensuring adequate protein intake, as hair is primarily composed of keratin, a structural protein. Patients should aim for sufficient protein from a variety of sources including lean meats, fish, eggs, dairy products, legumes, and plant-based proteins. Distributing protein intake across meals helps maintain a steady supply of amino acids for hair follicle function.
Micronutrient optimisation is equally crucial. Patients should be encouraged to consume a varied, nutrient-dense diet rich in:
-
Iron — found in red meat, poultry, fish, lentils, and fortified cereals
-
Zinc — present in shellfish, meat, seeds, and nuts
-
Vitamin D — obtained through sunlight exposure, oily fish, and fortified foods
-
B vitamins, particularly B12 — found in animal products and fortified alternatives
For patients struggling to meet nutritional requirements through diet alone, a standard multivitamin supplement within recommended daily allowance (RDA) limits may be considered after discussion with a healthcare professional. Supplements should only be used to correct confirmed deficiencies, and high-dose formulations should be avoided unless specifically prescribed.
Moderating the rate of weight loss can significantly reduce the risk of telogen effluvium. Whilst GLP-1 medications are effective for weight reduction, aiming for a gradual loss of 0.5–1 kg per week is generally safer and more sustainable, in line with NHS guidance. Patients should work with their prescriber to titrate the medication dose appropriately and avoid excessively restrictive eating patterns. Very low-calorie diets should only be followed under medical supervision.
Regular monitoring of nutritional status through blood tests — including full blood count, ferritin, thyroid function tests, vitamin B12, folate, and vitamin D — allows early detection and correction of deficiencies. Patients with significant dietary restrictions or ongoing nutritional concerns may benefit from referral to a registered dietitian. Maintaining good overall health through adequate sleep, stress management, and gentle scalp care also supports hair follicle function during treatment.
Treatment Options for GLP-1 Related Hair Loss
When hair loss occurs despite preventative measures, several evidence-based treatment options can help manage the condition and support hair regrowth. The first step is identifying and correcting any nutritional deficiencies through blood tests. If deficiencies are detected, targeted supplementation under medical supervision is appropriate. For example, iron deficiency should be treated with oral iron supplements (ferrous sulphate or ferrous fumarate), whilst vitamin B12 deficiency may require oral or intramuscular replacement depending on the underlying cause.
Topical minoxidil (available over-the-counter as Regaine in the UK) is licensed for androgenetic alopecia (male and female pattern hair loss). The 5% solution or foam for men and 2% solution for women can be applied to the scalp according to product instructions. While primarily used for pattern hair loss, some clinicians may suggest minoxidil for telogen effluvium to support recovery, though this would be an off-label use and evidence is less established for this indication. Patients should be advised that initial shedding may occur in the first few weeks, and visible improvement typically takes 3–6 months of consistent use. For male androgenetic alopecia, oral finasteride 1 mg is another licensed treatment option, though it is not indicated for telogen effluvium or for use in women.
Reassurance and watchful waiting are often appropriate, as telogen effluvium is typically self-limiting. Once the triggering factor (rapid weight loss) stabilises and nutritional status improves, hair follicles usually return to normal cycling within 3–6 months, with visible regrowth apparent by 6–12 months. During this time, patients may benefit from gentle hair care practices, avoiding harsh chemical treatments, tight hairstyles, and excessive heat styling.
Patients should be advised to contact their GP urgently if hair loss is accompanied by scalp pain, redness, scaling, or loss of follicular openings, as these may indicate scarring alopecia requiring prompt dermatological assessment. Other reasons to seek medical advice include severe or progressive hair loss, patches of complete baldness, or signs of systemic illness. In cases where hair loss significantly impacts quality of life or fails to improve after 6 months, referral to a dermatologist for specialist assessment may be warranted. The decision to continue or modify GLP-1 treatment should be made collaboratively, weighing the benefits of metabolic control against the distress caused by hair loss.
Scientific References
- Wegovy 0.25 mg, FlexTouch solution for injection in pre-filled pen - Summary of Product Characteristics (SmPC).
- GLP-1 receptor agonists: reminder of the potential side effects and to be aware of the potential for misuse.
- Lose weight - Better Health.
- Ozempic EPAR - Public Assessment Report.
- GLP-1 agonists and hair loss: a call for further investigation.
Frequently Asked Questions
Is hair loss from GLP-1 medications permanent?
No, hair loss from GLP-1 medications is typically temporary telogen effluvium that resolves within 3–6 months once weight loss stabilises and nutritional deficiencies are corrected. Visible regrowth usually becomes apparent within 6–12 months.
What vitamins should I take to prevent hair loss on GLP-1?
Focus on adequate intake of iron, zinc, vitamin D, and B vitamins (particularly B12) through a varied, nutrient-dense diet. A standard multivitamin within RDA limits may be considered if dietary intake is insufficient, but supplements should ideally target confirmed deficiencies identified through blood tests.
Should I stop taking my GLP-1 medication if I experience hair loss?
Do not stop GLP-1 medication without consulting your prescriber, as the underlying condition (diabetes or obesity) requires ongoing management. Discuss your concerns with your GP or prescribing clinician, who can assess nutritional status, implement preventative strategies, and determine whether treatment modification is appropriate.
The health-related content published on this site is based on credible scientific sources and is periodically reviewed to ensure accuracy and relevance. Although we aim to reflect the most current medical knowledge, the material is meant for general education and awareness only.
The information on this site is not a substitute for professional medical advice. For any health concerns, please speak with a qualified medical professional. By using this information, you acknowledge responsibility for any decisions made and understand we are not liable for any consequences that may result.
Heading 1
Heading 2
Heading 3
Heading 4
Heading 5
Heading 6
Lorem ipsum dolor sit amet, consectetur adipiscing elit, sed do eiusmod tempor incididunt ut labore et dolore magna aliqua. Ut enim ad minim veniam, quis nostrud exercitation ullamco laboris nisi ut aliquip ex ea commodo consequat. Duis aute irure dolor in reprehenderit in voluptate velit esse cillum dolore eu fugiat nulla pariatur.
Block quote
Ordered list
- Item 1
- Item 2
- Item 3
Unordered list
- Item A
- Item B
- Item C
Bold text
Emphasis
Superscript
Subscript