GLP-1 receptor agonists such as semaglutide (Ozempic, Wegovy) and liraglutide (Saxenda, Victoza) are increasingly prescribed for type 2 diabetes and weight management. Whilst these medications offer significant clinical benefits, many patients wonder: do GLP-1 make you gassy? Gastrointestinal side effects, including gas, bloating, and flatulence, are recognised adverse effects of this medication class. Understanding why these symptoms occur, how common they are, and what can be done to manage them is essential for patients starting or considering GLP-1 therapy. This article explores the relationship between GLP-1 medications and digestive symptoms, offering practical guidance on managing discomfort whilst continuing treatment.
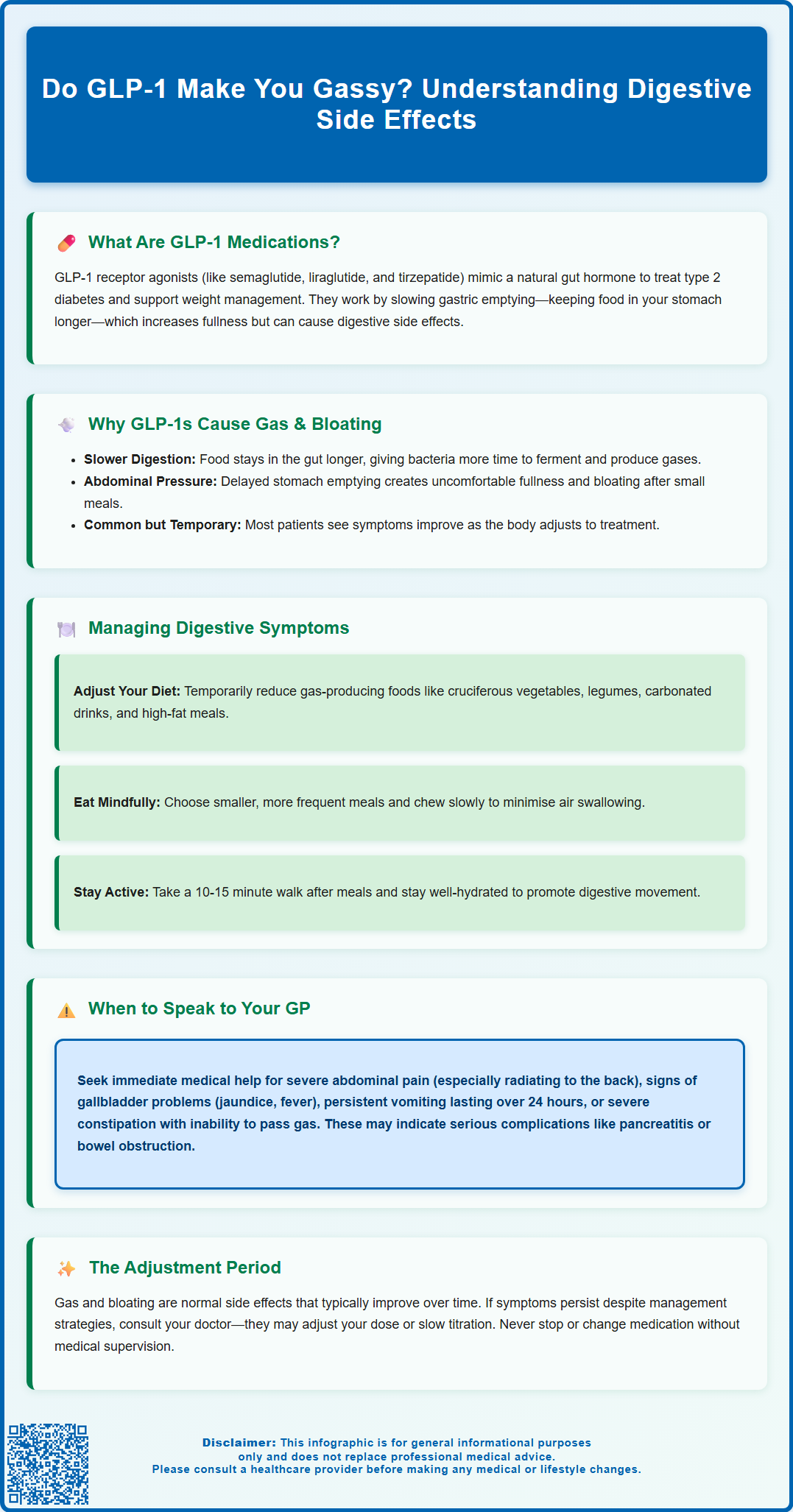
Summary: GLP-1 receptor agonists can cause gas and bloating by slowing gastric emptying, which prolongs food transit through the digestive tract and increases bacterial fermentation.
- GLP-1 medications slow gastric emptying, allowing intestinal bacteria more time to ferment food and produce gas
- Gas, bloating, and flatulence are classified as common side effects, though frequency varies between products and individuals
- Symptoms typically emerge during initial treatment or dose escalation and often improve as the body adapts
- Dietary modifications, smaller meals, and gradual fibre adjustment can help manage gastrointestinal symptoms
- Severe abdominal pain, persistent vomiting, or signs of pancreatitis or gallbladder disease require prompt medical attention
Table of Contents
What Are GLP-1 Medications and How Do They Work?
GLP-1 receptor agonists are a class of medications originally developed for type 2 diabetes management and now some are also licensed for weight management. These medicines include semaglutide (Ozempic, Wegovy, Rybelsus), liraglutide (Victoza, Saxenda), dulaglutide (Trulicity), and tirzepatide (Mounjaro)—though tirzepatide is technically a dual GIP/GLP-1 receptor agonist rather than a pure GLP-1 agonist. They work by mimicking the action of glucagon-like peptide-1, a naturally occurring hormone produced in the intestine.
The mechanism of action involves several physiological effects. GLP-1 receptor agonists stimulate insulin secretion from the pancreas when blood glucose levels are elevated, helping to control blood sugar. Simultaneously, they suppress glucagon release, which prevents the liver from producing excess glucose. These medications also act on the brain's appetite centres, promoting feelings of fullness and reducing hunger signals.
Crucially for understanding gastrointestinal side effects, GLP-1 medications slow gastric emptying—the rate at which food moves from the stomach into the small intestine. This delayed emptying contributes to prolonged satiety and improved glycaemic control, but it also affects digestive processes. The slowed transit time means food remains in the digestive tract longer, which can influence gas production and bowel habits.
According to NICE guidance, GLP-1 receptor agonists are recommended for specific patient groups with type 2 diabetes (NG28) and, in some formulations like Wegovy (semaglutide 2.4mg) and Saxenda (liraglutide 3mg), for weight management in adults with obesity or overweight with weight-related comorbidities. These medications are typically administered via subcutaneous injection, either daily or weekly depending on the specific formulation, though oral semaglutide (Rybelsus) is available for type 2 diabetes. Understanding how these medications work helps explain why certain gastrointestinal symptoms may occur during treatment.
Do GLP-1 Medications Cause Gas and Bloating?
Yes, gastrointestinal side effects including gas, bloating, and flatulence can occur with GLP-1 receptor agonist therapy. Clinical trial data and post-marketing surveillance identify these symptoms among the adverse effects, though their frequency varies considerably between products and individuals.
The primary reason GLP-1 medications can make you gassy relates to their effect on gastric motility. By slowing the movement of food through the digestive system, these medications alter the normal fermentation processes in the gut. When food remains in the gastrointestinal tract longer, intestinal bacteria have extended time to break down carbohydrates and fibre, producing gases such as hydrogen, methane, and carbon dioxide as by-products. This increased gas production can lead to bloating, abdominal distension, and flatulence.
Additionally, the delayed gastric emptying may cause a sensation of fullness and abdominal pressure that patients often describe as bloating. This isn't always due to excess gas but rather the physical presence of food remaining in the stomach and upper intestine for prolonged periods. Some patients report feeling uncomfortably full even after small meals, which can be accompanied by belching or the need to pass wind more frequently.
Prevalence varies by medication and dose. According to the Summaries of Product Characteristics (SmPCs), nausea is very common with most GLP-1 medications, while abdominal distension, eructation (belching), and flatulence are typically classified as common side effects, though frequencies differ between products. These symptoms typically emerge during the initial weeks of treatment or following dose escalation. For many patients, gastrointestinal side effects gradually improve as the body adapts to the medication, though the timeline varies by product and individual. However, some individuals experience persistent symptoms that may require management strategies or, occasionally, treatment discontinuation. While often uncomfortable, it's important to distinguish normal side effects from warning signs of more serious conditions like pancreatitis or gallbladder disease, which require prompt medical attention.
Managing Gas and Bloating While Taking GLP-1 Medications
Dietary modifications represent the first-line approach to managing gas and bloating during GLP-1 therapy. Reducing intake of gas-producing foods can significantly alleviate symptoms. These include cruciferous vegetables (broccoli, cauliflower, Brussels sprouts, cabbage), legumes (beans, lentils, chickpeas), onions, garlic, and carbonated beverages. Whilst these foods are nutritious, temporarily limiting them during the adjustment period may provide relief. Foods containing sugar alcohols (sorbitol, mannitol, xylitol) and very high-fat meals can also worsen bloating and may be best avoided during the initial adjustment period.
Eating smaller, more frequent meals rather than large portions works synergistically with the medication's mechanism. Since GLP-1 agonists already slow gastric emptying, consuming smaller quantities reduces the burden on the digestive system and minimises the sensation of uncomfortable fullness. Eating slowly and chewing food thoroughly also helps, as swallowing less air during meals reduces gas accumulation. Avoiding drinking through straws and limiting chewing gum can further decrease air intake.
Fibre intake requires careful consideration. Whilst dietary fibre is essential for overall health, rapidly increasing fibre consumption whilst on GLP-1 medications can exacerbate bloating. If you need to increase fibre, do so gradually over several weeks, allowing your digestive system to adapt. Soluble fibre sources like oats and psyllium may be better tolerated than insoluble fibre during the initial treatment phase.
Physical activity can promote gastrointestinal motility and help relieve bloating. A gentle walk after meals, even for 10–15 minutes, encourages digestive movement and gas passage. Staying well-hydrated throughout the day supports digestive function.
Over-the-counter remedies may provide symptomatic relief. Simethicone-containing products can help break up gas bubbles. Peppermint tea or capsules may ease bloating for some individuals, though should be avoided if you experience reflux or heartburn, which can also occur with GLP-1 medications. Always inform your GP or pharmacist about any additional medications or supplements you're considering, as interactions are possible. If symptoms persist despite these measures, your healthcare provider may consider adjusting your medication dose or slowing the titration schedule to improve tolerability.
When to Speak to Your GP About GLP-1 Side Effects
Whilst gas and bloating are common side effects, certain symptoms warrant prompt medical attention. Contact your GP immediately or call NHS 111 if you experience severe or persistent abdominal pain, particularly if it's sharp, localised, or worsening. This could indicate complications such as pancreatitis, a rare but serious adverse effect associated with GLP-1 medications. If you suspect pancreatitis (intense upper abdominal pain radiating to the back, accompanied by nausea and vomiting), stop taking your medication and seek urgent medical help.
Be alert for signs of gallbladder problems, which can occur with GLP-1 medications and weight loss. Symptoms include sudden pain in the upper right abdomen, fever, yellowing of the skin or eyes (jaundice), pale stools, or dark urine. These require prompt medical assessment.
Seek medical advice if gastrointestinal symptoms significantly impact your quality of life or prevent you from maintaining adequate nutrition and hydration. Persistent nausea, repeated vomiting, or inability to tolerate food and fluids can lead to dehydration and nutritional deficiencies. If you're unable to keep down medications or fluids for more than 24 hours, contact your healthcare provider promptly.
Changes in bowel habits beyond typical bloating should be discussed with your GP. Severe constipation lasting more than three days, particularly if accompanied by abdominal distension and inability to pass gas, requires same-day evaluation as this could indicate bowel obstruction. Conversely, persistent diarrhoea or the presence of blood in stools warrants immediate medical assessment.
You should also consult your GP if side effects don't improve after the expected adjustment period, or if they worsen despite implementing management strategies. Your doctor may consider dose adjustment, slower titration, or switching to an alternative formulation. In some cases, temporarily reducing the dose and then re-escalating more gradually can improve tolerability.
NICE guidance emphasises individualised treatment approaches. If gastrointestinal side effects are intolerable despite optimal management, discontinuation may be appropriate, and your healthcare team can discuss alternative treatment options. Never stop or adjust your medication without medical supervision, as this may affect your diabetes control or weight management goals. Report suspected side effects via the MHRA Yellow Card scheme (yellowcard.mhra.gov.uk).
Frequently Asked Questions
How long does gas and bloating last with GLP-1 medications?
Gas and bloating typically emerge during the first few weeks of treatment or after dose increases. For many patients, these symptoms gradually improve over several weeks as the body adapts, though the timeline varies individually and some people may experience persistent symptoms requiring management strategies.
Can I take anything to reduce gas whilst on GLP-1 medications?
Over-the-counter remedies such as simethicone-containing products may help relieve gas symptoms. Peppermint tea can ease bloating for some individuals, though it should be avoided if you experience reflux. Always inform your GP or pharmacist before taking additional medications or supplements to check for potential interactions.
When should I contact my GP about GLP-1 side effects?
Contact your GP immediately if you experience severe or persistent abdominal pain, signs of pancreatitis (intense upper abdominal pain radiating to the back with nausea), symptoms of gallbladder problems (upper right abdominal pain, jaundice, fever), persistent vomiting preventing adequate hydration, or if side effects significantly impact your quality of life despite management strategies.
The health-related content published on this site is based on credible scientific sources and is periodically reviewed to ensure accuracy and relevance. Although we aim to reflect the most current medical knowledge, the material is meant for general education and awareness only.
The information on this site is not a substitute for professional medical advice. For any health concerns, please speak with a qualified medical professional. By using this information, you acknowledge responsibility for any decisions made and understand we are not liable for any consequences that may result.
Heading 1
Heading 2
Heading 3
Heading 4
Heading 5
Heading 6
Lorem ipsum dolor sit amet, consectetur adipiscing elit, sed do eiusmod tempor incididunt ut labore et dolore magna aliqua. Ut enim ad minim veniam, quis nostrud exercitation ullamco laboris nisi ut aliquip ex ea commodo consequat. Duis aute irure dolor in reprehenderit in voluptate velit esse cillum dolore eu fugiat nulla pariatur.
Block quote
Ordered list
- Item 1
- Item 2
- Item 3
Unordered list
- Item A
- Item B
- Item C
Bold text
Emphasis
Superscript
Subscript










