Saxenda (liraglutide) is a GLP-1 receptor agonist licensed in the UK for weight management, but some patients experience acid reflux or gastro-oesophageal reflux disease (GORD) during treatment. This occurs because Saxenda delays gastric emptying, which can increase the likelihood of stomach contents refluxing into the oesophagus. Understanding why reflux occurs and implementing practical dietary and lifestyle modifications can significantly reduce symptoms whilst maintaining the benefits of treatment. This article explores evidence-based strategies to avoid reflux on Saxenda, when to seek medical advice, and alternative management options if symptoms persist.
Summary: Reflux on Saxenda can be avoided through dietary modifications (smaller, frequent meals; avoiding trigger foods and late-night eating), lifestyle adjustments (elevating the bed head, remaining upright after meals), and pharmacological support such as proton pump inhibitors if needed.
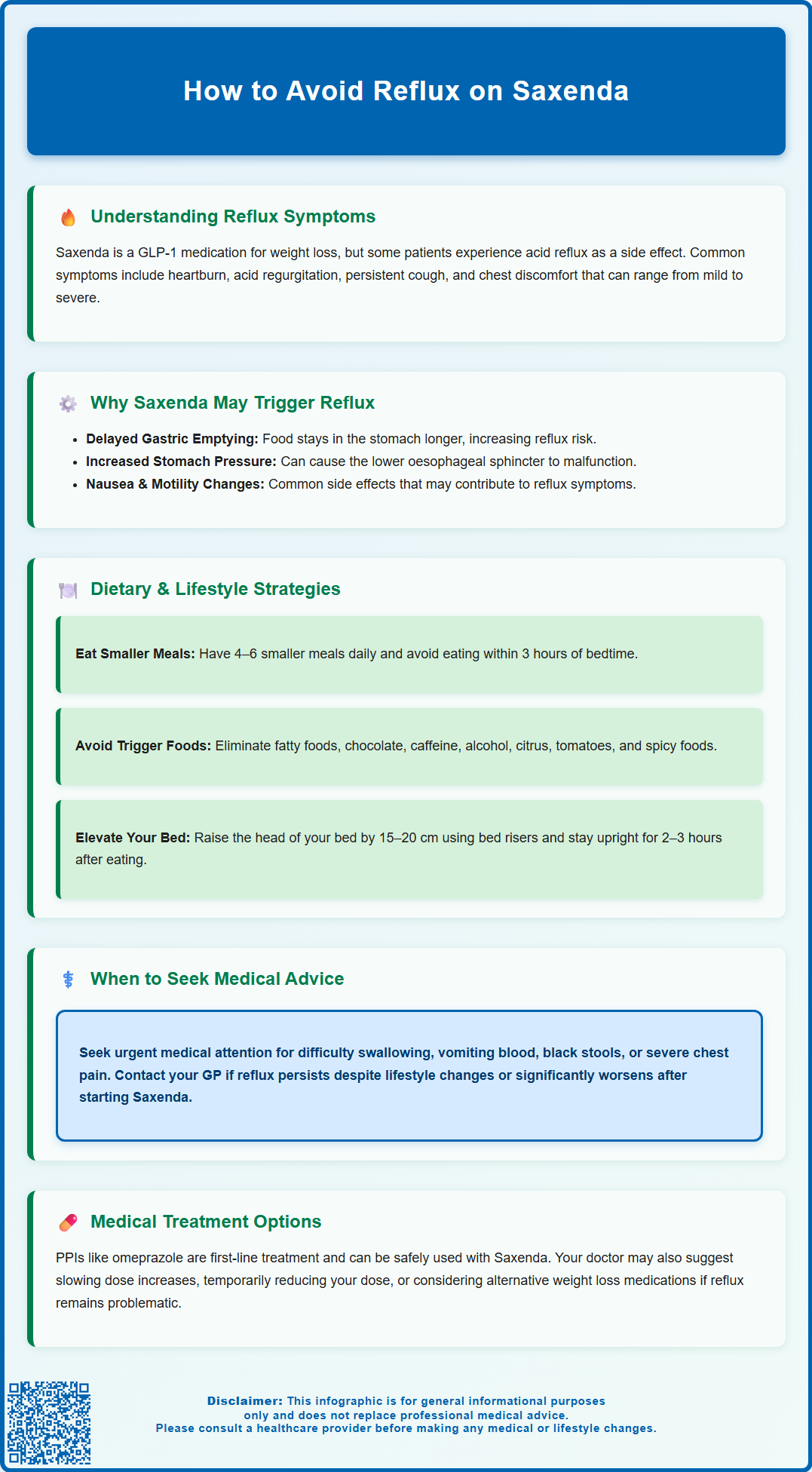
- Saxenda delays gastric emptying as a GLP-1 receptor agonist, which can increase reflux risk by prolonging stomach distension and raising gastric pressure.
- Eating smaller, more frequent meals and avoiding fatty foods, caffeine, alcohol, and late-night eating reduces gastric pressure and reflux symptoms.
- Elevating the head of the bed by 15–20 cm and remaining upright for 2–3 hours after meals helps prevent nocturnal reflux.
- Red flag symptoms including dysphagia, persistent vomiting, haematemesis, or unintentional weight loss require urgent medical assessment.
- Proton pump inhibitors such as omeprazole are first-line pharmacological treatment for GORD and can be used alongside Saxenda.
- Dose adjustment or alternative weight management medications may be considered if reflux symptoms remain intolerable despite optimisation.
Table of Contents
Understanding Reflux Symptoms While Taking Saxenda
Saxenda (liraglutide) is a glucagon-like peptide-1 (GLP-1) receptor agonist licensed in the UK for weight management in adults with a body mass index (BMI) of 30 kg/m² or greater, or 27 kg/m² or greater with weight-related comorbidities. While Saxenda can be effective for weight loss as demonstrated in clinical trials, some patients report experiencing gastrointestinal symptoms, including acid reflux or gastro-oesophageal reflux disease (GORD).
Common reflux symptoms that patients may notice include:
-
Heartburn — a burning sensation in the chest, often after eating
-
Regurgitation of stomach contents or acid into the throat or mouth
-
Persistent cough, hoarseness, or throat clearing
-
Chest discomfort that may mimic cardiac pain
It is important to recognise that reflux symptoms can vary considerably between individuals. Some patients may experience mild, occasional discomfort, whilst others report more persistent or troublesome symptoms that affect quality of life. The onset of reflux symptoms may coincide with starting Saxenda or increasing the dose, though there is no official link established as a direct causal relationship in all cases.
Understanding the nature and timing of your symptoms is essential for effective management. Keeping a symptom diary — noting when reflux occurs, its severity, and any potential triggers such as specific foods or meal timing — can help you and your healthcare provider identify patterns and develop an appropriate management strategy. If you experience new or worsening reflux symptoms after starting Saxenda, it is advisable to discuss these with your GP or prescribing clinician.
Why Saxenda May Trigger or Worsen Acid Reflux
The mechanism by which Saxenda may contribute to reflux symptoms relates to its pharmacological action on the gastrointestinal tract. As a GLP-1 receptor agonist, liraglutide works by mimicking the action of the naturally occurring incretin hormone GLP-1. This leads to several physiological effects that support weight loss, including enhanced satiety, reduced appetite, and — crucially — delayed gastric emptying.
Delayed gastric emptying means that food remains in the stomach for a longer period before passing into the small intestine. Whilst this contributes to feelings of fullness and reduced calorie intake, it can also increase the likelihood of gastric contents refluxing back into the oesophagus, particularly when the stomach is distended. The lower oesophageal sphincter (LOS), which normally acts as a barrier between the stomach and oesophagus, may be more prone to relaxation or incompetence when gastric pressure is elevated.
Additionally, patients taking Saxenda may experience nausea, which is one of the most commonly reported adverse effects according to the Summary of Product Characteristics (SmPC). Nausea can be associated with altered gastric motility, which may contribute to reflux symptoms. Gastrointestinal side effects, including nausea and dyspepsia, are well-documented in the SmPC for Saxenda, though the precise incidence of reflux is not always clearly delineated.
Other contributing factors may include:
-
Dietary changes — patients may alter eating patterns or food choices during weight loss
-
Increased abdominal pressure — though this typically improves with weight loss over time
-
Individual susceptibility — pre-existing GORD or hiatus hernia may predispose patients to worsening symptoms
It's important to note that individual responses vary, and not all patients taking Saxenda will experience reflux symptoms.
Practical Ways to Avoid Reflux on Saxenda
There are several evidence-based lifestyle and dietary modifications that can help minimise reflux symptoms whilst taking Saxenda. These strategies focus on reducing gastric pressure, supporting normal oesophageal function, and avoiding known reflux triggers.
Dietary modifications:
-
Eat smaller, more frequent meals — large meals increase gastric distension and pressure, raising the risk of reflux. Aim for 4–6 smaller meals throughout the day rather than 2–3 large ones.
-
Avoid late-night eating — finish your last meal at least 3 hours before lying down to allow time for gastric emptying.
-
Identify and avoid trigger foods — common culprits include fatty or fried foods, chocolate, caffeine, alcohol, citrus fruits, tomatoes, spicy foods, and carbonated beverages. Keep a food diary to identify personal triggers.
-
Choose low-fat options — high-fat meals delay gastric emptying further, compounding the effect of Saxenda.
-
Stay well hydrated — sip water throughout the day, but avoid drinking large volumes with meals, which can increase gastric volume.
Lifestyle adjustments:
-
Elevate the head of your bed — raising the head by 15–20 cm (using bed risers, not just pillows) can reduce nocturnal reflux by using gravity to keep stomach contents down.
-
Maintain good posture — avoid slouching or bending over immediately after eating, as this increases abdominal pressure.
-
Wear loose-fitting clothing — tight waistbands or belts can compress the abdomen and promote reflux.
-
Avoid lying down after meals — remain upright for at least 2–3 hours post-meal.
-
Consider smoking cessation — smoking weakens the lower oesophageal sphincter and should be avoided.
-
Avoid or minimise NSAIDs — non-steroidal anti-inflammatory drugs can exacerbate reflux symptoms; seek medical advice if you require regular pain relief.
Medication timing:
- Administer Saxenda at a consistent time each day. Some patients find that the timing of injection affects their symptoms, though there is no official guidance on optimal timing for reflux prevention. Discuss any timing adjustments with your prescriber if symptoms are troublesome.
These practical measures can significantly reduce reflux symptoms and improve tolerability of Saxenda treatment.
When to Seek Medical Advice About Reflux Symptoms
Whilst mild, occasional reflux symptoms can often be managed with lifestyle modifications, certain symptoms warrant prompt medical evaluation. It is important to recognise red flag symptoms that may indicate more serious underlying pathology or complications.
Seek urgent medical attention if you experience:
-
Dysphagia — difficulty swallowing or sensation of food sticking (this requires urgent assessment at any age)
-
Odynophagia — painful swallowing
-
Unintentional weight loss — beyond that expected from Saxenda treatment
-
Persistent vomiting — especially if containing blood or resembling coffee grounds
-
Haematemesis or melaena — vomiting blood or passing black, tarry stools, which may indicate gastrointestinal bleeding
-
Severe, persistent chest pain — particularly if new or different from typical reflux, as this requires exclusion of cardiac causes
-
Anaemia — unexplained iron deficiency or low haemoglobin
According to NICE guideline NG12, urgent specialist referral (within 2 weeks) should be considered for people aged 55 and over with weight loss AND upper abdominal pain, reflux, or dyspepsia.
Contact your GP or prescribing clinician if:
-
Reflux symptoms persist despite lifestyle modifications and over-the-counter antacids
-
Symptoms significantly worsen after starting or increasing Saxenda dose
-
You require regular use of proton pump inhibitors (PPIs) or H2-receptor antagonists
-
Symptoms interfere with daily activities, sleep, or quality of life
-
You have a history of Barrett's oesophagus, peptic ulcer disease, or previous gastrointestinal surgery
Your GP may consider investigations such as:
-
Testing for Helicobacter pylori — often recommended before starting empirical PPI therapy for uninvestigated dyspepsia
-
Trial of PPI therapy — typically a 4-week course of full-dose PPI for uninvestigated dyspepsia, with extension based on response
-
Upper gastrointestinal endoscopy (gastroscopy) — to visualise the oesophagus and stomach directly if symptoms persist or red flags are present
Early medical review ensures appropriate investigation and management, and helps determine whether Saxenda remains a suitable treatment option for you.
If you suspect an adverse reaction to Saxenda, you can report this through the MHRA Yellow Card scheme (yellowcard.mhra.gov.uk).
Alternative Approaches and Medication Adjustments
If reflux symptoms remain problematic despite lifestyle modifications, several pharmacological and alternative management strategies may be considered in consultation with your healthcare provider.
Pharmacological management of reflux:
-
Proton pump inhibitors (PPIs) — medications such as omeprazole, lansoprazole, or esomeprazole reduce gastric acid production and are first-line treatment for GORD. They are generally well-tolerated and can be used alongside Saxenda. NICE guidance typically recommends an initial 4-week trial of full-dose PPI for uninvestigated dyspepsia, with extension or step-down based on response.
-
H2-receptor antagonists — famotidine is available in the UK and may be an alternative for those who cannot tolerate PPIs, though these are generally less effective than PPIs for acid suppression.
-
Antacids and alginates — over-the-counter preparations (e.g., Gaviscon) provide symptomatic relief by neutralising acid and forming a protective barrier. These can be used as needed for breakthrough symptoms.
Saxenda dose adjustment:
If reflux symptoms are severe or persistent, your prescriber may consider:
-
Slowing dose escalation — Saxenda is typically titrated weekly from 0.6 mg to the maintenance dose of 3.0 mg. A slower titration schedule may improve gastrointestinal tolerability.
-
Temporary dose reduction — if symptoms are severe, reducing to a previously tolerated dose may be appropriate.
According to the Saxenda SmPC, the recommended maintenance dose is 3.0 mg once daily. Treatment should be discontinued after 12 weeks on the 3.0 mg dose if patients have not lost at least 5% of their initial body weight. Treatment should also be reconsidered if the 3.0 mg dose is not tolerated.
Alternative weight management medications:
If reflux symptoms remain intolerable despite optimisation, alternative pharmacological options for weight management may be discussed:
-
Orlistat — a lipase inhibitor that reduces fat absorption. It has a different side effect profile (primarily gastrointestinal, but not typically reflux).
-
Other GLP-1 receptor agonists — such as semaglutide (Wegovy), though these share a similar mechanism and may cause comparable symptoms.
-
Combination approaches — integrating dietary support, psychological interventions, and increased physical activity alongside or instead of pharmacotherapy.
Non-pharmacological support:
Referral to specialist services may be beneficial:
-
Dietitian — for personalised dietary advice and meal planning
-
Tier 3 weight management services — multidisciplinary support available through NHS pathways
-
Gastroenterology — if reflux symptoms are severe, refractory, or associated with red flag features
The decision to continue, adjust, or discontinue Saxenda should be made collaboratively between you and your healthcare provider, weighing the benefits of weight loss against the impact of side effects on quality of life.
Frequently Asked Questions
Why does Saxenda cause acid reflux?
Saxenda delays gastric emptying as part of its mechanism to promote satiety, which means food remains in the stomach longer. This increases gastric pressure and the likelihood of stomach contents refluxing into the oesophagus, particularly when the stomach is distended.
What foods should I avoid to reduce reflux whilst taking Saxenda?
Common reflux triggers include fatty or fried foods, chocolate, caffeine, alcohol, citrus fruits, tomatoes, spicy foods, and carbonated beverages. Keeping a food diary can help identify your personal triggers.
When should I see a doctor about reflux symptoms on Saxenda?
Seek urgent medical attention for red flag symptoms including difficulty swallowing, persistent vomiting, vomiting blood, black stools, or severe chest pain. Contact your GP if symptoms persist despite lifestyle changes or significantly worsen after starting Saxenda.
The health-related content published on this site is based on credible scientific sources and is periodically reviewed to ensure accuracy and relevance. Although we aim to reflect the most current medical knowledge, the material is meant for general education and awareness only.
The information on this site is not a substitute for professional medical advice. For any health concerns, please speak with a qualified medical professional. By using this information, you acknowledge responsibility for any decisions made and understand we are not liable for any consequences that may result.
Heading 1
Heading 2
Heading 3
Heading 4
Heading 5
Heading 6
Lorem ipsum dolor sit amet, consectetur adipiscing elit, sed do eiusmod tempor incididunt ut labore et dolore magna aliqua. Ut enim ad minim veniam, quis nostrud exercitation ullamco laboris nisi ut aliquip ex ea commodo consequat. Duis aute irure dolor in reprehenderit in voluptate velit esse cillum dolore eu fugiat nulla pariatur.
Block quote
Ordered list
- Item 1
- Item 2
- Item 3
Unordered list
- Item A
- Item B
- Item C
Bold text
Emphasis
Superscript
Subscript










