Ozempic (semaglutide) is a once-weekly GLP-1 receptor agonist widely prescribed in the UK for type 2 diabetes management. Clinical trials demonstrate that Ozempic typically reduces HbA1c by 1.0–1.8% (11–20 mmol/mol), depending on the dose and individual factors. This substantial reduction helps many patients achieve NICE-recommended glycaemic targets whilst also supporting weight loss and cardiovascular health. Understanding how much Ozempic lowers HbA1c, the factors influencing response, and what to expect during treatment enables informed discussions between patients and healthcare professionals about optimising diabetes control.
Summary: Ozempic typically lowers HbA1c by 1.0–1.8% (11–20 mmol/mol) in adults with type 2 diabetes, with greater reductions at higher doses.
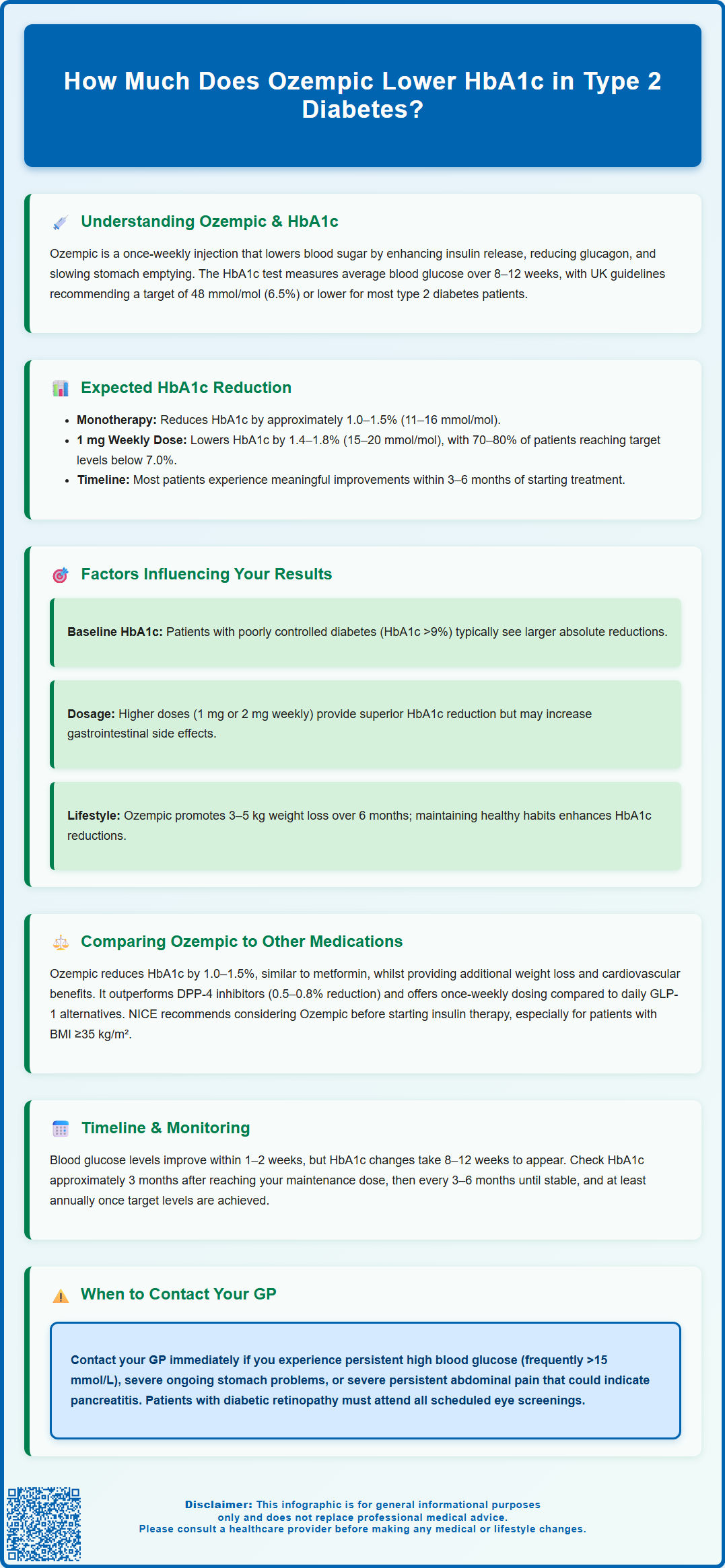
- Ozempic is a GLP-1 receptor agonist administered as a once-weekly subcutaneous injection for type 2 diabetes.
- The 0.5 mg weekly dose reduces HbA1c by approximately 1.0–1.5% (11–16 mmol/mol), whilst the 1 mg dose achieves 1.4–1.8% (15–20 mmol/mol) reductions.
- Individual response varies based on baseline HbA1c, dosage, adherence, concomitant medications, and lifestyle factors.
- Measurable HbA1c reduction typically occurs 8–12 weeks after reaching therapeutic dose, with NICE recommending monitoring every 3–6 months until stable.
- Ozempic demonstrates superior or equivalent HbA1c reduction compared to most other diabetes medications, including other GLP-1 receptor agonists.
- Common adverse effects include nausea and gastrointestinal symptoms; patients should report severe abdominal pain or visual changes promptly to their healthcare team.
Table of Contents
- Understanding Ozempic and Its Effect on HbA1c Levels
- Clinical Evidence: Expected HbA1c Reduction with Ozempic
- Factors That Influence How Much Ozempic Lowers Your HbA1c
- Comparing Ozempic's HbA1c Reduction to Other Diabetes Medications
- What to Expect: Timeline and Monitoring Your HbA1c on Ozempic
- Frequently Asked Questions
Understanding Ozempic and Its Effect on HbA1c Levels
Ozempic (semaglutide) is a glucagon-like peptide-1 receptor agonist (GLP-1 RA) licensed in the UK for the treatment of type 2 diabetes mellitus. It works by mimicking the action of the naturally occurring hormone GLP-1, which plays a crucial role in glucose regulation. When administered as a once-weekly subcutaneous injection, Ozempic enhances insulin secretion in a glucose-dependent manner, suppresses inappropriate glucagon release, slows gastric emptying, and promotes satiety.
The HbA1c test (glycated haemoglobin) measures average blood glucose levels over the preceding 8–12 weeks and serves as the gold standard for assessing long-term glycaemic control. In the UK, NICE recommends targeting an HbA1c level of 48 mmol/mol (6.5%) or lower for most adults with type 2 diabetes managed with lifestyle interventions or a single antidiabetic drug not associated with hypoglycaemia. For those on medications that may cause hypoglycaemia or where tighter control is inappropriate, a target of 53 mmol/mol (7.0%) may be more suitable.
Ozempic's mechanism of action directly addresses several pathophysiological defects in type 2 diabetes, making it particularly effective at lowering HbA1c. By enhancing the body's own insulin response only when blood glucose is elevated, it reduces the risk of hypoglycaemia compared to some other glucose-lowering therapies. The medication is typically initiated at 0.25 mg once weekly for four weeks (a non-therapeutic dose intended to improve gastrointestinal tolerability), then increased to 0.5 mg weekly. Depending on glycaemic response and tolerability, the dose may be further increased to 1 mg weekly after at least four weeks, with a maximum licensed dose of 2 mg weekly available for those requiring additional glycaemic control after at least four weeks at the 1 mg dose.
Importantly, Ozempic is not indicated for type 1 diabetes or diabetic ketoacidosis. It should be avoided in pregnancy and breastfeeding unless specifically advised by a specialist. Patients with pre-existing diabetic retinopathy should be monitored closely, as rapid improvements in blood glucose control may temporarily worsen retinopathy, particularly in those also using insulin.
Clinical Evidence: Expected HbA1c Reduction with Ozempic
The efficacy of Ozempic in reducing HbA1c has been extensively evaluated in the SUSTAIN clinical trial programme, a series of phase 3 studies involving thousands of participants with type 2 diabetes. These trials provide robust evidence for the magnitude of HbA1c reduction patients can expect at different doses.
In the SUSTAIN 1 trial, which examined Ozempic as monotherapy, participants achieved mean HbA1c reductions of approximately 1.0–1.5% (11–16 mmol/mol) from baseline after 30 weeks of treatment, depending on the dose used. The SUSTAIN 6 cardiovascular outcomes trial demonstrated similar reductions, with participants on 0.5 mg weekly achieving a mean reduction of 1.1% (12 mmol/mol) and those on 1 mg weekly achieving 1.4% (15 mmol/mol) at 104 weeks.
When used in combination with other antidiabetic medications, Ozempic has shown even more substantial benefits. The SUSTAIN 7 head-to-head trial comparing Ozempic with dulaglutide (another GLP-1 RA) found that Ozempic 0.5 mg reduced HbA1c by 1.5% (16 mmol/mol) and the 1 mg dose by 1.8% (20 mmol/mol) from baseline. Importantly, a significantly higher proportion of participants achieved the therapeutic target of HbA1c below 53 mmol/mol (7.0%)—approximately 70–80% of those on the 1 mg dose.
The SUSTAIN FORTE trial specifically evaluated the 2 mg dose compared to 1 mg, demonstrating additional HbA1c lowering benefit for patients requiring intensification beyond the 1 mg dose.
It is worth noting that baseline HbA1c influences absolute reduction: individuals starting with higher HbA1c levels typically experience greater absolute reductions, though percentage reductions remain relatively consistent. Clinical experience in UK practice generally aligns with these trial findings, with most patients experiencing clinically meaningful HbA1c reductions within 3–6 months of initiating therapy.
Factors That Influence How Much Ozempic Lowers Your HbA1c
While clinical trials provide average HbA1c reductions, individual responses to Ozempic can vary considerably based on several patient-specific and treatment-related factors. Understanding these variables helps set realistic expectations and optimise therapeutic outcomes.
Baseline HbA1c level is perhaps the most significant predictor of absolute reduction. Patients with poorly controlled diabetes (HbA1c >75 mmol/mol or 9%) typically experience larger absolute decreases than those with near-target levels. However, this does not diminish the clinical value for those with moderately elevated HbA1c, as achieving and maintaining target levels significantly reduces long-term complications.
Dosage and dose escalation directly impact efficacy. The 1 mg weekly dose consistently demonstrates superior HbA1c reduction compared to 0.5 mg, and the 2 mg dose (where appropriate) may provide additional benefit for some individuals. However, dose escalation must be balanced against tolerability, particularly gastrointestinal adverse effects such as nausea, which affect approximately 15–20% of users according to clinical trials.
Adherence to treatment is crucial. As a once-weekly injection, Ozempic offers advantages over daily medications, but missed doses can compromise glycaemic control. Concomitant medications also matter—Ozempic works synergistically with metformin and may be combined with SGLT2 inhibitors or insulin, potentially enhancing overall HbA1c reduction. When adding Ozempic to insulin or sulfonylureas, consider reducing the doses of these medications to mitigate hypoglycaemia risk, with increased glucose monitoring during treatment changes.
Lifestyle factors including diet, physical activity, and weight management significantly influence outcomes. Ozempic promotes weight loss (typically 3–5 kg over 6 months), which independently improves insulin sensitivity and glycaemic control. Patients who engage with structured diabetes education programmes and maintain healthy lifestyle behaviours generally achieve better HbA1c reductions.
Finally, duration of diabetes and residual beta-cell function affect response. Those with longstanding diabetes and significant beta-cell exhaustion may experience more modest improvements, though Ozempic remains effective across the disease spectrum. No dose adjustment is required at any stage of renal impairment, though maintaining adequate hydration is important, especially if gastrointestinal side effects occur.
Comparing Ozempic's HbA1c Reduction to Other Diabetes Medications
When considering treatment options for type 2 diabetes, understanding how Ozempic compares to other glucose-lowering medications helps inform shared decision-making between patients and healthcare professionals.
Metformin typically reduces HbA1c by approximately 1.0–1.5% (11–16 mmol/mol) and remains the usual first-line treatment recommended by NICE for most people with type 2 diabetes. Ozempic demonstrates comparable or slightly superior efficacy, with the added benefits of weight loss and cardiovascular risk reduction as demonstrated in the SUSTAIN 6 trial.
SGLT2 inhibitors (such as dapagliflozin, empagliflozin, and canagliflozin) generally reduce HbA1c by 0.5–1.0% (5–11 mmol/mol), somewhat less than Ozempic. However, they offer complementary benefits including cardiovascular and renal protection. NICE now recommends SGLT2 inhibitors as first-line therapy for people with established or high risk of cardiovascular disease, heart failure, or chronic kidney disease. They are often used in combination with GLP-1 RAs for patients requiring intensified therapy.
DPP-4 inhibitors (such as sitagliptin and linagliptin) provide modest HbA1c reductions of approximately 0.5–0.8% (5–9 mmol/mol), considerably less than Ozempic. They are weight-neutral and well-tolerated but lack the weight loss and cardiovascular benefits of GLP-1 RAs.
Compared to other GLP-1 receptor agonists, Ozempic demonstrates superior or equivalent efficacy. The SUSTAIN 7 trial showed Ozempic 0.5 mg and 1 mg provided significantly greater HbA1c reductions than dulaglutide 0.75 mg and 1.5 mg respectively. Compared to liraglutide (Victoza), another once-daily GLP-1 RA, Ozempic offers similar or slightly better glycaemic control with the convenience of once-weekly dosing.
Insulin therapy can achieve substantial HbA1c reductions but carries risks of hypoglycaemia and weight gain. NICE guidance suggests considering GLP-1 RAs like Ozempic before intensifying to insulin in many patients, particularly those with BMI ≥35 kg/m² or for whom weight gain or hypoglycaemia would be problematic. When insulin is necessary, Ozempic can be used in combination, often allowing for lower insulin doses and better overall metabolic control.
What to Expect: Timeline and Monitoring Your HbA1c on Ozempic
Understanding the expected timeline for HbA1c improvement and appropriate monitoring schedules helps patients and clinicians assess treatment response and make informed decisions about ongoing management.
Initial response to Ozempic begins within days of the first injection, with improvements in fasting and post-prandial glucose levels typically evident within 1–2 weeks. However, because HbA1c reflects average glucose over the preceding 8–12 weeks, measurable changes in this parameter lag behind actual glycaemic improvements. Most patients will not see significant HbA1c reduction until they have been on a therapeutic dose (0.5 mg or higher) for at least 8–12 weeks.
NICE recommends reviewing HbA1c every 3–6 months until stable, then at least annually once target levels are achieved. For patients initiating Ozempic, a practical approach involves checking HbA1c approximately 3 months after reaching the maintenance dose. This allows sufficient time to assess response whilst avoiding unnecessary delays in treatment optimisation. If HbA1c remains above target, dose escalation (from 0.5 mg to 1 mg, or 1 mg to 2 mg where appropriate) should be considered, provided the medication is well-tolerated.
Self-monitoring of blood glucose may be recommended for some patients, particularly those on combination therapy with insulin or sulphonylureas, or those experiencing symptoms of hypo- or hyperglycaemia. Increased monitoring is especially important when starting Ozempic alongside these medications, as dose reductions may be needed to prevent hypoglycaemia. Routine self-monitoring is not necessary for all patients on Ozempic monotherapy or in combination with metformin.
Patients should be advised to contact their GP or diabetes team if they experience persistent hyperglycaemia (frequent blood glucose readings >15 mmol/L), severe or persistent gastrointestinal symptoms, or signs of pancreatitis (severe, persistent abdominal pain). While diabetic ketoacidosis (DKA) is not typically associated with GLP-1 RAs alone, patients using Ozempic with SGLT2 inhibitors or after significant insulin dose reductions should be alert to DKA symptoms and seek urgent care if these develop.
Patients with pre-existing diabetic retinopathy should attend all scheduled eye screening appointments and report any sudden visual changes promptly. Regular monitoring also includes assessment of renal function, though no dose adjustment is required at any stage of renal impairment. Weight, blood pressure, and cardiovascular risk factors should be reviewed as part of comprehensive diabetes care.
If you experience any suspected side effects from Ozempic, report them to the MHRA Yellow Card Scheme (yellowcard.mhra.gov.uk or via the Yellow Card app).
Frequently Asked Questions
How long does it take for Ozempic to lower HbA1c?
Measurable HbA1c reduction typically occurs 8–12 weeks after reaching a therapeutic dose (0.5 mg or higher), as HbA1c reflects average blood glucose over the preceding 8–12 weeks. Most patients see clinically meaningful improvements within 3–6 months of initiating therapy.
Is Ozempic more effective than metformin at lowering HbA1c?
Ozempic demonstrates comparable or slightly superior HbA1c reduction to metformin (both typically reduce HbA1c by 1.0–1.5%), with additional benefits including weight loss and cardiovascular risk reduction. Metformin remains the usual first-line treatment recommended by NICE for most people with type 2 diabetes.
What HbA1c target should I aim for on Ozempic?
NICE recommends targeting an HbA1c of 48 mmol/mol (6.5%) or lower for most adults with type 2 diabetes managed with lifestyle interventions or a single antidiabetic drug not associated with hypoglycaemia. For those on medications that may cause hypoglycaemia or where tighter control is inappropriate, a target of 53 mmol/mol (7.0%) may be more suitable.
The health-related content published on this site is based on credible scientific sources and is periodically reviewed to ensure accuracy and relevance. Although we aim to reflect the most current medical knowledge, the material is meant for general education and awareness only.
The information on this site is not a substitute for professional medical advice. For any health concerns, please speak with a qualified medical professional. By using this information, you acknowledge responsibility for any decisions made and understand we are not liable for any consequences that may result.
Heading 1
Heading 2
Heading 3
Heading 4
Heading 5
Heading 6
Lorem ipsum dolor sit amet, consectetur adipiscing elit, sed do eiusmod tempor incididunt ut labore et dolore magna aliqua. Ut enim ad minim veniam, quis nostrud exercitation ullamco laboris nisi ut aliquip ex ea commodo consequat. Duis aute irure dolor in reprehenderit in voluptate velit esse cillum dolore eu fugiat nulla pariatur.
Block quote
Ordered list
- Item 1
- Item 2
- Item 3
Unordered list
- Item A
- Item B
- Item C
Bold text
Emphasis
Superscript
Subscript










