Achieving optimal results from Ozempic (semaglutide) requires more than simply administering the weekly injection. This GLP-1 receptor agonist, licensed in the UK for type 2 diabetes management, works most effectively when combined with proper injection technique, gradual dose titration, evidence-based dietary modifications, and regular physical activity. Understanding how to use Ozempic correctly, managing potential side effects, and maintaining close communication with your healthcare team are essential components of successful treatment. This comprehensive guide provides practical, clinically grounded advice to help you maximise the therapeutic benefits of Ozempic whilst minimising risks and ensuring safe, sustainable diabetes management.
Summary: Best results from Ozempic are achieved through correct weekly injection technique, gradual dose escalation, combining treatment with a balanced diet and regular physical activity, managing gastrointestinal side effects appropriately, and attending regular monitoring appointments with your healthcare team.
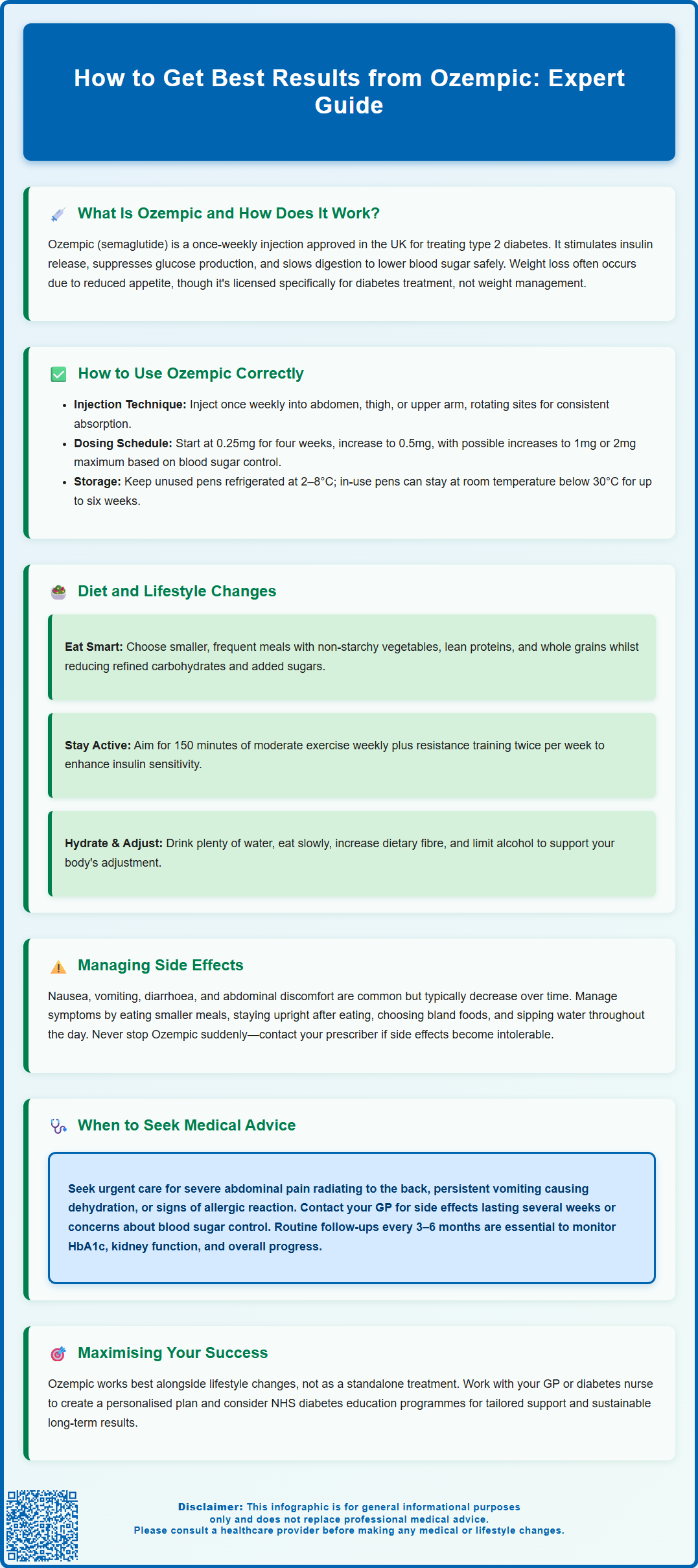
- Ozempic is a GLP-1 receptor agonist licensed in the UK for type 2 diabetes, administered as a once-weekly subcutaneous injection with gradual dose increases from 0.25mg to a maximum of 2mg.
- Proper injection technique includes rotating sites (abdomen, thigh, or upper arm), using a new needle each time, and storing unused pens refrigerated at 2–8°C.
- Combining Ozempic with a balanced diet rich in vegetables, lean proteins, and whole grains, plus at least 150 minutes weekly of moderate-intensity exercise, maximises effectiveness.
- Common gastrointestinal side effects (nausea, vomiting, diarrhoea) typically diminish over time and can be managed with smaller, frequent meals and avoiding fatty or spicy foods.
- Regular monitoring of HbA1c, renal function, body weight, and diabetic retinopathy screening is essential, with urgent medical attention required for severe abdominal pain or signs of pancreatitis.
- Ozempic should be discontinued at least two months before planned pregnancy and is not recommended during breastfeeding or for patients with type 1 diabetes.
Table of Contents
What Is Ozempic and How Does It Work?
Ozempic (semaglutide) is a prescription medication licensed in the UK for the treatment of type 2 diabetes mellitus in adults, as an adjunct to diet and exercise. It belongs to a class of medicines called glucagon-like peptide-1 (GLP-1) receptor agonists, which mimic the action of a naturally occurring hormone that regulates blood glucose levels and appetite.
The mechanism of action involves several complementary pathways. Ozempic stimulates insulin secretion from pancreatic beta cells in a glucose-dependent manner, meaning it primarily promotes insulin release when blood sugar levels are elevated. This reduces the risk of hypoglycaemia when used alone, though this risk increases when combined with insulin or sulphonylureas. Simultaneously, it suppresses glucagon secretion—a hormone that raises blood glucose—thereby preventing excessive glucose production by the liver. Additionally, Ozempic slows gastric emptying, which moderates the rate at which nutrients enter the bloodstream after meals.
Many patients also experience weight loss whilst taking Ozempic, which occurs through reduced appetite and increased satiety. This effect has led to significant interest in the medication beyond diabetes management, though it is important to note that in the UK, Ozempic is specifically licensed for type 2 diabetes. A related formulation (Wegovy, containing higher-dose semaglutide) is licensed separately for weight management.
Ozempic is administered as a once-weekly subcutaneous injection using a pre-filled pen device. It is typically initiated at a low dose and gradually increased over several weeks to minimise gastrointestinal side effects. Ozempic is not indicated for patients with type 1 diabetes or diabetic ketoacidosis. It should not be used during pregnancy or breastfeeding, and should be discontinued at least two months before a planned pregnancy. Caution is needed in patients with diabetic retinopathy, as rapid improvement in glucose control may temporarily worsen this condition.
How to Use Ozempic Correctly for Best Results
Achieving optimal results with Ozempic requires correct administration technique and adherence to the prescribed dosing schedule. The medication is supplied in a pre-filled, multi-dose pen that delivers subcutaneous injections. Patients should inject into areas with adequate subcutaneous tissue: the abdomen (avoiding a 5cm radius around the navel), thigh, or upper arm. Rotating injection sites within these areas helps prevent lipodystrophy (changes in fat tissue) and ensures consistent absorption.
The standard dosing regimen begins with 0.25mg once weekly for the first four weeks. This initial dose is primarily for tolerability rather than glycaemic control. After four weeks, the dose is increased to 0.5mg weekly. If additional blood glucose control is needed after at least four weeks at this dose, it may be increased to 1mg weekly, and subsequently to a maximum of 2mg weekly if required. These gradual increases allow the gastrointestinal system to adapt and reduce the likelihood of nausea and vomiting.
Timing and consistency are important factors. Ozempic can be administered at any time of day, with or without meals, but should be given on the same day each week. If a dose is missed, it should be administered as soon as possible within five days of the missed dose. If more than five days have passed, skip the missed dose and resume the regular schedule. Never double up doses to compensate.
Proper pen storage is essential: unused pens should be refrigerated (2–8°C) with the cap on to protect from light, and must never be frozen. Pens in use can be kept at room temperature (below 30°C) for up to six weeks. Always check the solution before injecting—it should be clear and colourless. Discard the pen if the solution appears cloudy, discoloured, or contains particles, or if it has been frozen.
Important safety measures include using a new needle for each injection, never sharing pens with others (even if the needle is changed), and disposing of used needles in a proper sharps container. If you are also taking insulin or sulphonylureas, your doctor may reduce these doses when starting Ozempic to minimise the risk of hypoglycaemia. Refer to the Patient Information Leaflet and Instructions for Use provided with your medication for detailed guidance, and consider asking your healthcare professional for a demonstration before your first injection.
Diet and Lifestyle Changes to Maximise Ozempic Effectiveness
Ozempic is most effective when combined with evidence-based dietary modifications and increased physical activity. The medication is not a standalone solution but rather one component of comprehensive diabetes management. NICE guidelines emphasise that pharmacological interventions should complement, not replace, lifestyle measures.
Dietary recommendations focus on achieving sustainable, gradual weight loss (if appropriate) and improving glycaemic control. A balanced diet rich in non-starchy vegetables, lean proteins, whole grains, and healthy fats supports both objectives. Patients should aim to:
-
Reduce portion sizes gradually, as Ozempic naturally decreases appetite—forcing large meals may exacerbate nausea
-
Limit refined carbohydrates and added sugars, which cause rapid blood glucose spikes
-
Increase dietary fibre through vegetables, pulses, and whole grains to improve satiety and glycaemic control
-
Stay well hydrated, particularly as reduced food intake may decrease fluid consumption
-
Eat slowly and mindfully, allowing time for satiety signals to register
-
Moderate alcohol intake in line with UK guidelines, as alcohol affects blood glucose and can interact with diabetes medications
Many patients find that smaller, more frequent meals are better tolerated than three large meals, especially during dose escalation. Avoiding high-fat, greasy foods can also reduce gastrointestinal discomfort.
Physical activity enhances insulin sensitivity and contributes to weight management. The UK Chief Medical Officers' guidelines and NICE recommend that adults with type 2 diabetes aim for at least 150 minutes of moderate-intensity aerobic activity weekly, spread across several days, plus resistance training twice weekly. This might include brisk walking, cycling, swimming, or structured exercise classes. Even modest increases in activity—such as taking the stairs or gardening—provide metabolic benefits.
Patients should work with their GP or diabetes specialist nurse to develop an individualised plan that considers their current fitness level, comorbidities, and personal preferences. Many NHS areas offer structured education programmes for diabetes self-management (such as DESMOND). Referral to a dietitian may be beneficial for tailored nutritional guidance. For those who smoke, cessation support should be offered as smoking increases cardiovascular risk. Sustainable lifestyle changes, rather than restrictive diets, produce the best long-term outcomes when combined with Ozempic therapy.
Managing Side Effects While Taking Ozempic
Gastrointestinal side effects are the most commonly reported adverse reactions with Ozempic, particularly during initiation and dose escalation. These include nausea, vomiting, diarrhoea, constipation, and abdominal discomfort. According to the SmPC, these effects are dose-dependent and typically diminish over time as tolerance develops. The gradual dose titration schedule is specifically designed to minimise these effects.
To manage nausea and related symptoms:
-
Eat smaller, more frequent meals rather than large portions
-
Avoid lying down immediately after eating—remain upright for 1–2 hours
-
Choose bland, easily digestible foods during symptomatic periods (toast, rice, bananas)
-
Avoid triggers such as spicy, fatty, or heavily seasoned foods
-
Stay hydrated, taking small sips throughout the day if drinking larger amounts causes discomfort
If constipation develops, increase dietary fibre gradually, maintain adequate hydration, and consider discussing appropriate laxatives with your pharmacist or GP. Conversely, if diarrhoea or vomiting persists, ensure adequate fluid and electrolyte replacement to prevent dehydration. Severe or persistent vomiting or diarrhoea can lead to dehydration and potential kidney problems—seek medical advice if you have reduced urination, dizziness, or extreme thirst.
Injection site reactions—including redness, itching, or mild swelling—occasionally occur but are usually self-limiting. Rotating injection sites and ensuring the medication reaches room temperature before injecting can reduce discomfort.
More serious adverse effects require prompt medical attention. These include:
-
Severe, persistent abdominal pain (potentially indicating pancreatitis)—if suspected, stop taking Ozempic and seek urgent medical assessment
-
Right upper abdominal pain, fever, or yellowing of skin/eyes (possible gallbladder disease, which occurs more frequently in patients losing weight)
-
Signs of thyroid issues (neck lump, persistent hoarseness, difficulty swallowing)
-
Symptoms of hypoglycaemia when used with insulin or sulphonylureas (tremor, sweating, confusion, palpitations)
-
Allergic reactions (rash, difficulty breathing, facial swelling)
-
Changes in vision or signs of diabetic retinopathy worsening
Patients should never discontinue Ozempic abruptly without medical guidance. If side effects become intolerable, contact your prescriber to discuss dose adjustment or alternative management strategies. Report suspected side effects to the MHRA Yellow Card scheme (yellowcard.mhra.gov.uk or via the Yellow Card app).
Monitoring Your Progress and When to Seek Medical Advice
Regular monitoring is essential to assess treatment response and identify any complications early. Patients taking Ozempic should have routine follow-up appointments with their GP or diabetes care team, typically every 3–6 months initially, then at least annually once stable.
Key monitoring parameters include:
-
HbA1c levels (glycated haemoglobin)—the primary measure of long-term glucose control, with targets individualised according to NICE guidance, considering factors such as age, comorbidities, and hypoglycaemia risk
-
Body weight and BMI—to track weight changes and adjust dietary advice accordingly
-
Blood pressure—as improved glycaemic control and weight loss may affect cardiovascular risk
-
Renal function (eGFR and urine albumin-to-creatinine ratio)—to monitor kidney health
-
Lipid profile—to assess cardiovascular risk factors
-
Diabetic retinopathy screening—particularly important as rapid improvement in glucose control may temporarily worsen retinopathy in those with pre-existing disease
Many patients also benefit from home blood glucose monitoring, particularly if taking other diabetes medications that increase hypoglycaemia risk. Your healthcare team will advise on appropriate testing frequency based on individual circumstances.
When to seek urgent medical advice:
-
Severe, persistent abdominal pain radiating to the back, with or without vomiting (possible pancreatitis)
-
Symptoms of dehydration from persistent vomiting or diarrhoea (dizziness, reduced urination, extreme thirst)
-
Signs of hypoglycaemia that don't resolve with usual measures
-
Right upper abdominal pain, fever, or yellowing of skin/eyes (possible gallbladder disease)
-
Neck swelling or lump, persistent hoarseness, or difficulty swallowing
-
Sudden vision changes or eye pain
-
Signs of severe allergic reaction (difficulty breathing, facial swelling, widespread rash)
Contact your GP or diabetes nurse if you:
-
Experience persistent side effects that don't improve after several weeks
-
Have difficulty adhering to the medication schedule
-
Are concerned about inadequate glucose control despite treatment
-
Notice significant unexplained weight loss or gain
-
Become pregnant or are planning pregnancy (Ozempic should be discontinued at least two months before planned conception)
-
Are breastfeeding (Ozempic is not recommended during breastfeeding)
-
Have any new symptoms that worry you
If you drive and take Ozempic with medications that can cause hypoglycaemia (insulin or sulphonylureas), follow DVLA guidance on monitoring blood glucose before driving and take precautions to avoid hypoglycaemia while driving.
Optimal outcomes with Ozempic require a collaborative approach between patient and healthcare team. Attend scheduled appointments, communicate openly about challenges or concerns, and actively participate in your diabetes management plan. This partnership approach, combined with correct medication use and lifestyle modifications, provides the best opportunity for achieving and maintaining treatment goals whilst minimising risks.
Frequently Asked Questions
What is the correct way to inject Ozempic for best results?
Inject Ozempic subcutaneously once weekly into the abdomen (avoiding 5cm around the navel), thigh, or upper arm, rotating sites to prevent tissue changes. Use a new needle each time, administer on the same day each week, and follow the gradual dose escalation schedule starting at 0.25mg for four weeks.
What diet changes should I make whilst taking Ozempic?
Focus on a balanced diet rich in non-starchy vegetables, lean proteins, whole grains, and healthy fats, whilst reducing refined carbohydrates and added sugars. Eat smaller, more frequent meals to manage appetite changes and minimise gastrointestinal side effects, and stay well hydrated throughout the day.
When should I contact my doctor whilst taking Ozempic?
Seek urgent medical advice for severe persistent abdominal pain (possible pancreatitis), signs of dehydration from vomiting or diarrhoea, symptoms of hypoglycaemia that don't resolve, right upper abdominal pain with fever, neck swelling, sudden vision changes, or signs of severe allergic reaction. Contact your GP for persistent side effects, difficulty adhering to treatment, or if planning pregnancy.
The health-related content published on this site is based on credible scientific sources and is periodically reviewed to ensure accuracy and relevance. Although we aim to reflect the most current medical knowledge, the material is meant for general education and awareness only.
The information on this site is not a substitute for professional medical advice. For any health concerns, please speak with a qualified medical professional. By using this information, you acknowledge responsibility for any decisions made and understand we are not liable for any consequences that may result.
Heading 1
Heading 2
Heading 3
Heading 4
Heading 5
Heading 6
Lorem ipsum dolor sit amet, consectetur adipiscing elit, sed do eiusmod tempor incididunt ut labore et dolore magna aliqua. Ut enim ad minim veniam, quis nostrud exercitation ullamco laboris nisi ut aliquip ex ea commodo consequat. Duis aute irure dolor in reprehenderit in voluptate velit esse cillum dolore eu fugiat nulla pariatur.
Block quote
Ordered list
- Item 1
- Item 2
- Item 3
Unordered list
- Item A
- Item B
- Item C
Bold text
Emphasis
Superscript
Subscript












