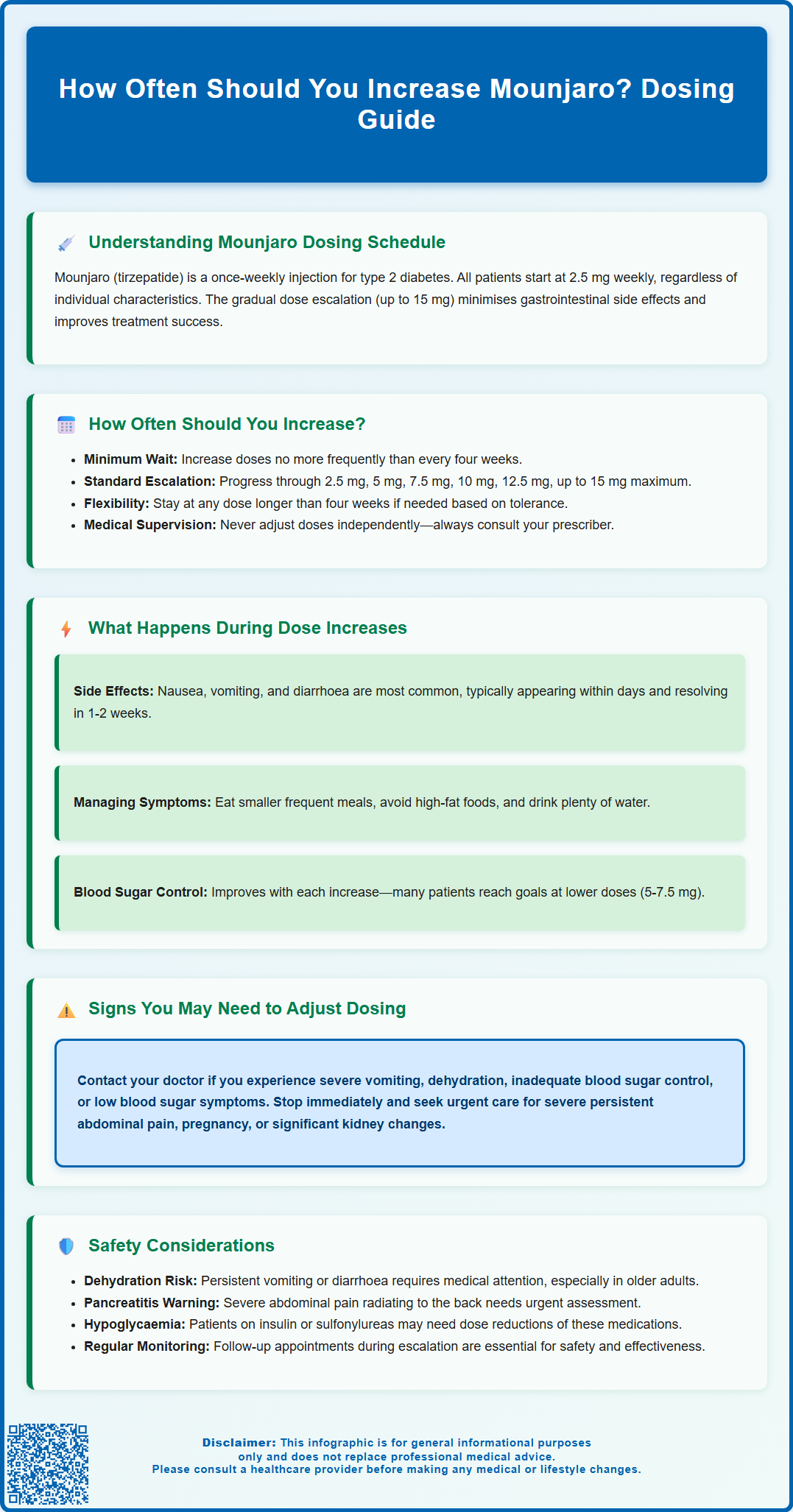
Mounjaro (tirzepatide) is a once-weekly injectable medication for type 2 diabetes that requires careful dose escalation to optimise effectiveness whilst minimising side effects. Understanding how often you should increase Mounjaro is essential for safe, successful treatment. According to MHRA-approved guidance, doses should be increased no more frequently than every four weeks, starting from 2.5 mg and potentially progressing to a maximum of 15 mg weekly. This structured approach balances therapeutic benefits with tolerability, allowing your body to adapt gradually. All dose adjustments must be made under medical supervision, with your prescriber monitoring your response, blood glucose control, and any adverse effects before authorising each increase.
Summary: Mounjaro doses should be increased no more frequently than every four weeks, as specified in MHRA-approved prescribing guidance.
- Mounjaro (tirzepatide) is a dual GIP/GLP-1 receptor agonist for type 2 diabetes, administered once weekly by subcutaneous injection.
- Treatment begins at 2.5 mg weekly, with potential escalation through 5 mg, 7.5 mg, 10 mg, 12.5 mg, to a maximum of 15 mg weekly.
- The four-week interval between dose increases minimises gastrointestinal side effects such as nausea, vomiting, and diarrhoea.
- Dose escalation requires medical supervision, with prescribers assessing glycaemic control, tolerability, and HbA1c levels before each increase.
- Patients should contact their healthcare provider for persistent vomiting, severe abdominal pain, signs of dehydration, or hypoglycaemia symptoms.
Table of Contents
Understanding Mounjaro Dosing Schedule
Mounjaro (tirzepatide) is a once-weekly injectable medication licensed in the UK for the treatment of type 2 diabetes mellitus. It is a dual glucose-dependent insulinotropic polypeptide (GIP) and glucagon-like peptide-1 (GLP-1) receptor agonist that works by enhancing insulin secretion when blood glucose levels are elevated, suppressing glucagon release, slowing gastric emptying, and reducing appetite.
The medication follows a structured dose escalation schedule designed to minimise gastrointestinal side effects whilst optimising therapeutic efficacy. Mounjaro is available in pre-filled pens containing 2.5 mg, 5 mg, 7.5 mg, 10 mg, 12.5 mg, or 15 mg doses. All patients begin treatment at the lowest dose of 2.5 mg once weekly, regardless of their treatment goals or baseline characteristics.
This gradual titration approach is not arbitrary—it reflects clinical trial evidence demonstrating that stepwise dose increases significantly reduce the incidence and severity of common adverse effects such as nausea, vomiting, diarrhoea, and abdominal discomfort. The MHRA-approved Summary of Product Characteristics (SmPC) emphasises this approach to balance tolerability with glycaemic control outcomes.
Understanding this dosing framework is essential for patients and prescribers alike, as deviations from the recommended schedule may compromise treatment adherence or increase the risk of discontinuation due to intolerable side effects. The structured approach also allows healthcare professionals to monitor individual patient responses and make informed decisions about dose progression.
How Often Should You Increase Mounjaro Dose?
According to the MHRA-approved Summary of Product Characteristics (SmPC), Mounjaro doses should be increased no more frequently than every four weeks. This means each dose level should be maintained for at least four weeks before considering an increase.
The typical dose escalation pathway may proceed as follows:
-
Weeks 1–4: 2.5 mg once weekly (starting dose)
-
Weeks 5–8: 5 mg once weekly
-
Weeks 9–12: 7.5 mg once weekly
-
Weeks 13–16: 10 mg once weekly
-
Weeks 17–20: 12.5 mg once weekly
-
Week 21 onwards: 15 mg once weekly (maximum licensed dose)
Importantly, this four-week interval represents the minimum time between dose increases. The SmPC allows for slower titration based on individual tolerability and clinical need. Some patients may benefit from remaining at a particular dose level for longer than four weeks before attempting further escalation, especially if experiencing significant side effects.
For patients using Mounjaro for type 2 diabetes, the maintenance dose should be individualised based on glycaemic response and tolerability. The maximum dose is 15 mg once weekly.
It is crucial that dose increases are made only under medical supervision. Your prescriber will review your response to treatment, tolerability, HbA1c levels, and any adverse effects before authorising each dose escalation. Never adjust your Mounjaro dose independently or attempt to accelerate the prescribed titration schedule.
What Happens During Each Mounjaro Dose Increase
Each dose escalation represents a stepwise increase in medication exposure, which intensifies both therapeutic effects and the potential for adverse reactions. Understanding what to expect during these transitions can help patients manage their treatment more effectively and recognise when medical advice is needed.
Gastrointestinal effects are the most commonly reported adverse reactions during dose increases. According to the SmPC, these may include nausea, vomiting, diarrhoea, constipation, abdominal pain, and reduced appetite. These symptoms typically emerge within the first few days following a dose increase and often diminish over 1–2 weeks as the body adapts. Eating smaller, more frequent meals, avoiding high-fat foods, and staying well-hydrated can help mitigate these effects.
Enhanced therapeutic effects also become more apparent with each dose increase. Patients with type 2 diabetes may notice improved blood glucose control, reflected in lower fasting glucose readings and reduced postprandial (after-meal) glucose excursions.
Some patients may experience injection site reactions—including redness, itching, or mild swelling—though these are generally mild and transient. Rotating injection sites (abdomen, thigh, or upper arm) can help minimise local reactions.
It is important to note that not all patients will progress to the maximum 15 mg dose. Your healthcare provider will determine your optimal maintenance dose based on treatment response, tolerability, and individual clinical circumstances. Some patients achieve their therapeutic goals at lower doses (5 mg or 7.5 mg) and may not require further escalation.
Patients should also be aware that rapid weight loss associated with GLP-1 receptor agonists may increase the risk of gallbladder problems. Contact your healthcare provider if you experience severe pain in the upper right abdomen, particularly if accompanied by fever or yellowing of the skin or eyes.
Signs You May Need to Adjust Your Mounjaro Dosing
Whilst the standard dose escalation schedule (no more frequently than every four weeks) is appropriate for most patients, certain clinical scenarios may warrant dose adjustment or temporary interruption of titration. Recognising these signs is essential for safe and effective treatment.
Persistent or severe gastrointestinal symptoms are the most common reason for dose modification. If you experience intractable nausea, repeated vomiting (more than once daily), severe diarrhoea, or signs of dehydration (dark urine, dizziness, reduced urination), contact your prescriber promptly. In such cases, your doctor may recommend remaining at your current dose for an additional period before attempting further escalation, or temporarily reducing to the previous dose level.
Inadequate therapeutic response may also prompt dosing discussions. For patients with type 2 diabetes, if HbA1c levels remain above individualised targets despite adherence to treatment and lifestyle modifications, your clinician may consider progressing to a higher maintenance dose. NICE guidance (NG28) recommends individualised HbA1c targets, often between 48-53 mmol/mol (6.5-7%), depending on your specific circumstances.
Hypoglycaemia risk requires particular attention in patients taking Mounjaro alongside insulin or sulfonylureas. If you experience symptoms of low blood glucose (trembling, sweating, confusion, palpitations), your prescriber may need to reduce doses of concomitant glucose-lowering medications rather than adjusting Mounjaro itself.
Other circumstances requiring medical review include:
-
Pregnancy or planning pregnancy (Mounjaro should be discontinued; use effective contraception during treatment and for 1 month after the last dose)
-
Breastfeeding (Mounjaro should be avoided)
-
Acute pancreatitis symptoms (severe, persistent abdominal pain radiating to the back)
-
Significant changes in renal function
-
Unexplained persistent abdominal pain or changes in bowel habits
If you miss a dose, take it within 4 days after the missed dose. If more than 4 days have passed, skip the missed dose and take your next dose on the regularly scheduled day. You can change the day of weekly administration if necessary, as long as the time between doses is at least 3 days.
Never adjust your Mounjaro dose independently. All dosing decisions should be made collaboratively with your healthcare provider based on comprehensive clinical assessment.
Safety Considerations When Increasing Mounjaro
Patient safety must remain paramount throughout Mounjaro dose escalation. Several important considerations apply to all patients undergoing titration.
Gastrointestinal adverse effects, whilst common, can occasionally lead to complications. Persistent vomiting or diarrhoea may cause dehydration and electrolyte disturbances, particularly in older adults or those with pre-existing renal impairment. Patients should maintain adequate fluid intake and seek medical attention if they cannot tolerate oral fluids or notice signs of dehydration. Severe, persistent, or unusual abdominal pain warrants immediate medical evaluation.
Acute pancreatitis has been reported with GLP-1 receptor agonists, including Mounjaro. Patients should be aware of symptoms of pancreatitis—severe, persistent abdominal pain often radiating to the back, sometimes accompanied by vomiting—and seek urgent medical attention if these occur. Mounjaro should be discontinued if pancreatitis is confirmed.
Hypoglycaemia risk increases when Mounjaro is used in combination with insulin or sulfonylureas. Patients on these concomitant medications may require dose reductions of their insulin or sulfonylurea when initiating or escalating Mounjaro. Regular blood glucose monitoring is essential, and patients should be educated about recognising and managing hypoglycaemia.
Thyroid considerations: The SmPC notes that in rodent studies, tirzepatide was associated with thyroid C-cell tumours, though the relevance to humans is unknown. Patients should report any neck swelling, hoarseness, or difficulty swallowing to their healthcare provider.
Gallbladder disease: Weight loss may increase the risk of gallbladder problems. Seek medical advice for symptoms such as severe upper abdominal pain, fever, or jaundice.
Diabetic retinopathy: Patients with a history of diabetic retinopathy should be monitored closely, as rapid improvement in glucose control has been associated with temporary worsening of retinopathy.
When to contact your GP or prescriber:
-
Persistent vomiting or inability to keep fluids down
-
Severe abdominal pain, especially if radiating to the back
-
Signs of dehydration (reduced urination, dizziness, dark urine)
-
Symptoms of hypoglycaemia that don't resolve with treatment
-
Unexplained neck swelling or difficulty swallowing
-
Any concerns about side effects or treatment response
Regular follow-up appointments are essential during dose escalation to monitor treatment response, assess tolerability, review blood glucose progress, and adjust concomitant medications as needed. This collaborative approach between patient and healthcare provider optimises both the safety and efficacy of Mounjaro treatment.
If you experience any suspected side effects, report them to the MHRA through the Yellow Card Scheme (yellowcard.mhra.gov.uk).
Frequently Asked Questions
Can I increase my Mounjaro dose faster than every four weeks?
No, Mounjaro doses should not be increased more frequently than every four weeks, as specified in MHRA-approved guidance. This minimum interval allows your body to adapt and reduces the risk of gastrointestinal side effects.
What should I do if I experience severe side effects during a Mounjaro dose increase?
Contact your prescriber immediately if you experience persistent vomiting, severe abdominal pain, signs of dehydration, or other concerning symptoms. Your doctor may recommend remaining at your current dose longer or temporarily reducing to the previous dose level.
Do all patients need to reach the maximum 15 mg Mounjaro dose?
No, not all patients require the maximum dose. Your healthcare provider will determine your optimal maintenance dose based on your glycaemic control, tolerability, and individual treatment goals—many patients achieve therapeutic targets at lower doses.
The health-related content published on this site is based on credible scientific sources and is periodically reviewed to ensure accuracy and relevance. Although we aim to reflect the most current medical knowledge, the material is meant for general education and awareness only.
The information on this site is not a substitute for professional medical advice. For any health concerns, please speak with a qualified medical professional. By using this information, you acknowledge responsibility for any decisions made and understand we are not liable for any consequences that may result.
Heading 1
Heading 2
Heading 3
Heading 4
Heading 5
Heading 6
Lorem ipsum dolor sit amet, consectetur adipiscing elit, sed do eiusmod tempor incididunt ut labore et dolore magna aliqua. Ut enim ad minim veniam, quis nostrud exercitation ullamco laboris nisi ut aliquip ex ea commodo consequat. Duis aute irure dolor in reprehenderit in voluptate velit esse cillum dolore eu fugiat nulla pariatur.
Block quote
Ordered list
- Item 1
- Item 2
- Item 3
Unordered list
- Item A
- Item B
- Item C
Bold text
Emphasis
Superscript
Subscript