Hiccups during Ozempic (semaglutide) treatment can be troublesome, though they are not listed as an official adverse reaction in UK product information. How to stop Ozempic hiccups involves understanding the potential link between GLP-1 receptor agonists and gastrointestinal effects that may trigger the hiccup reflex. Delayed gastric emptying, a key mechanism of semaglutide, can lead to gastric distension and diaphragmatic irritation. This article explores immediate relief techniques, preventative dietary strategies, and when to seek medical advice for persistent hiccups whilst taking Ozempic for type 2 diabetes.
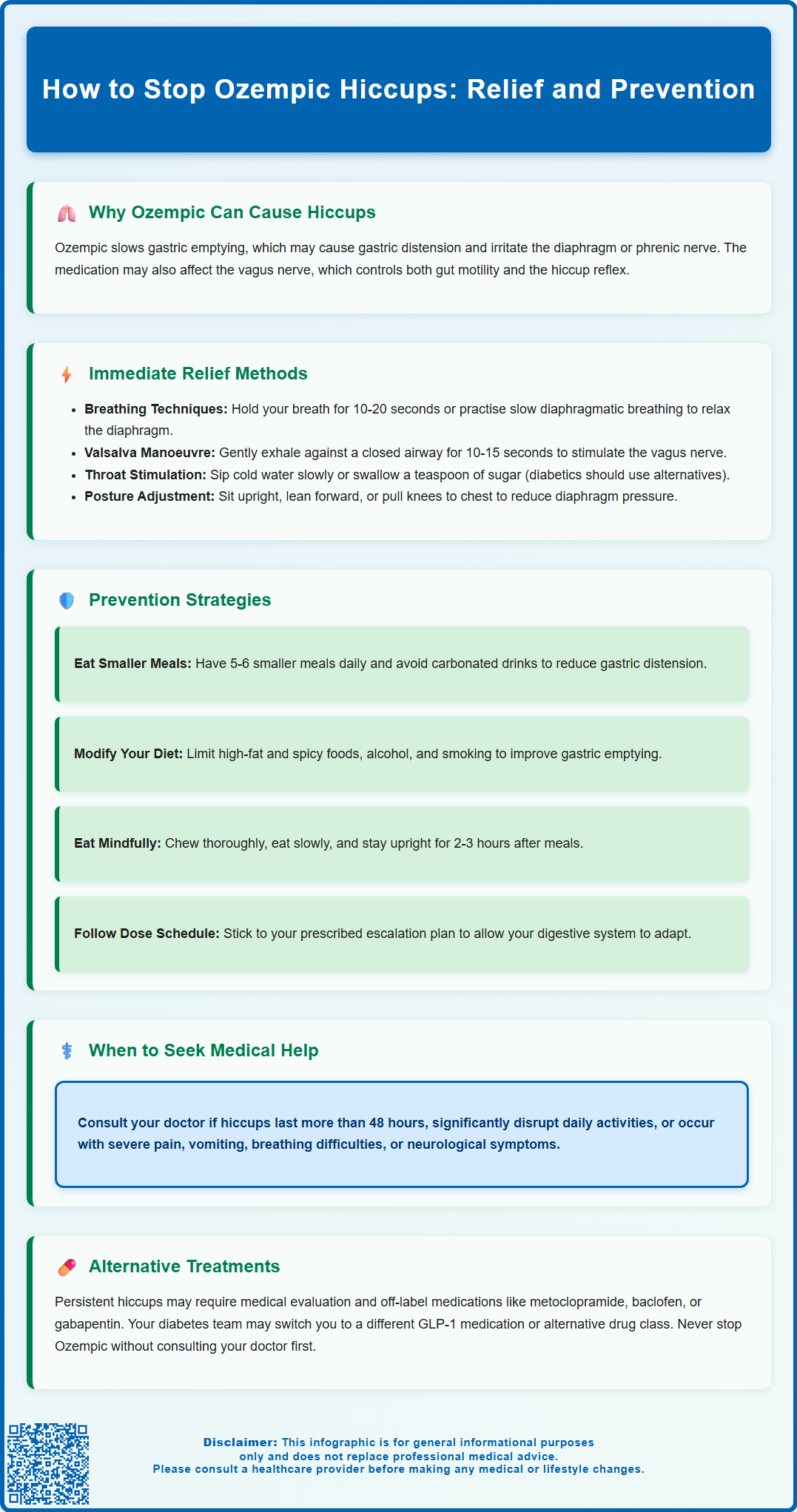
Summary: Ozempic hiccups can be stopped using breathing techniques (breath-holding, slow diaphragmatic breathing), physical manoeuvres (Valsalva, sipping cold water), dietary modifications (smaller meals, avoiding carbonated drinks), and medical treatments if symptoms persist beyond 48 hours.
- Ozempic (semaglutide) is a GLP-1 receptor agonist licensed in the UK for type 2 diabetes treatment; hiccups are not listed as an official adverse reaction in the Summary of Product Characteristics.
- Delayed gastric emptying caused by semaglutide may lead to gastric distension and diaphragmatic irritation, potentially triggering the hiccup reflex through vagal nerve stimulation.
- Immediate relief methods include breath-holding for 10–20 seconds, Valsalva manoeuvre, sipping cold water slowly, and postural adjustments to reduce gastric pressure on the diaphragm.
- Preventative strategies involve eating smaller frequent meals, avoiding carbonated beverages and high-fat foods, remaining upright after eating, and following the prescribed dose escalation schedule.
- Persistent hiccups lasting more than 48 hours require medical evaluation; pharmacological options include metoclopramide (≤5 days per MHRA guidance), baclofen, or proton pump inhibitors if reflux is contributing.
- Seek urgent medical attention if hiccups are accompanied by severe abdominal pain, chest pain, vomiting, difficulty breathing, neurological symptoms, or difficulty swallowing; report suspected side effects via the MHRA Yellow Card scheme.
Table of Contents
Why Ozempic Can Cause Hiccups
Ozempic (semaglutide) is a glucagon-like peptide-1 (GLP-1) receptor agonist licensed in the UK for the treatment of type 2 diabetes mellitus. A different semaglutide product, Wegovy, is licensed for weight management. Hiccups are not listed as an adverse reaction in the Summary of Product Characteristics (SmPC) for either medication, though some patients have reported experiencing persistent or troublesome hiccups during treatment.
The mechanism by which semaglutide might trigger hiccups is not fully established, but several pharmacological factors have been hypothesised. GLP-1 receptor agonists slow gastric emptying, which is central to their glucose-lowering and appetite-suppressing effects. This delayed transit could potentially lead to gastric distension, increased intra-abdominal pressure, and irritation of the diaphragm or phrenic nerve—known triggers for hiccup reflex activation. Additionally, some patients experience gastrointestinal side effects such as nausea, bloating, and reflux, all of which may indirectly stimulate the hiccup reflex arc.
Another hypothesis involves vagal nerve stimulation. The vagus nerve plays a critical role in both gastrointestinal motility and the hiccup reflex. Ozempic's effects on gut motility and gastric tone may alter vagal signalling, potentially predisposing certain individuals to hiccups. It is also worth noting that hiccups can occur as part of a broader constellation of upper gastrointestinal symptoms, particularly during dose escalation phases when the body is adjusting to the medication.
There is no established causal link between Ozempic and hiccups in large-scale clinical trials, and the evidence is limited to case reports and patient experiences. If you experience persistent hiccups lasting more than 48 hours, or if they are accompanied by severe abdominal pain, chest pain, vomiting, difficulty breathing, neurological symptoms, or difficulty swallowing, contact your GP, NHS 111, or in emergencies, call 999 for further assessment.
Suspected side effects can be reported via the MHRA Yellow Card scheme at yellowcard.mhra.gov.uk.
How to Stop Ozempic Hiccups: Immediate Relief Methods
When hiccups occur during Ozempic treatment, several commonly used techniques may provide relief by interrupting the hiccup reflex arc. These methods aim to stimulate the vagus or phrenic nerves, alter diaphragmatic contraction patterns, or increase carbon dioxide levels in the blood.
Breathing and respiratory techniques that may help include:
-
Breath-holding: Inhale deeply and hold your breath for 10–20 seconds before exhaling slowly. This increases blood CO₂ levels, which can suppress the hiccup reflex.
-
Slow, controlled breathing: Practise diaphragmatic breathing—inhale slowly through the nose for a count of four, hold briefly, then exhale through the mouth for a count of six. This promotes relaxation of the diaphragm.
-
Breathing into a paper bag: This technique may raise CO₂ concentration but should be used with extreme caution, for very brief periods only, and never with a plastic bag. Avoid completely if you have heart or lung conditions, and stop immediately if you feel lightheaded or short of breath.
Physical manoeuvres can also interrupt the reflex:
-
Valsalva manoeuvre: Exhale against a closed airway by pinching your nose and closing your mouth while attempting to breathe out gently for 10-15 seconds. This increases intrathoracic pressure and stimulates the vagus nerve.
-
Sipping cold water slowly: Small, deliberate sips can stimulate the pharynx and oesophagus, potentially resetting the hiccup cycle.
-
Swallowing a teaspoon of granulated sugar: This may stimulate vagal pathways. However, if you have diabetes, be aware this will affect your blood glucose levels—consider alternative methods or account for this in your glucose monitoring.
Postural adjustments such as sitting upright, leaning forward slightly, or pulling your knees to your chest can reduce gastric distension and relieve pressure on the diaphragm. If hiccups persist beyond a few hours despite these measures, or if they interfere significantly with eating, sleeping, or daily activities, seek medical advice. Persistent hiccups (lasting >48 hours) warrant clinical evaluation to exclude other underlying causes.
Preventing Hiccups While Taking Ozempic
Preventative strategies focus on minimising gastrointestinal disturbances and optimising medication tolerance, thereby reducing the likelihood of hiccup episodes during Ozempic therapy.
Dietary modifications are particularly important given Ozempic's effect on gastric emptying:
-
Eat smaller, more frequent meals: Large meals can exacerbate gastric distension and delay emptying. Aim for five to six smaller portions throughout the day rather than three large meals.
-
Avoid carbonated beverages: Fizzy drinks introduce gas into the stomach, increasing bloating and diaphragmatic irritation.
-
Limit high-fat and spicy foods: These can slow gastric emptying further and worsen reflux symptoms, both potential hiccup triggers.
-
Avoid alcohol and smoking: Both can aggravate reflux and potentially trigger hiccups.
-
Chew food thoroughly and eat slowly: Rapid eating increases air swallowing (aerophagia), contributing to gastric distension.
-
Remain upright after eating: Avoid lying down for at least two to three hours post-meal to facilitate gastric emptying and reduce reflux risk.
Medication administration timing may also play a role. Ozempic is typically administered once weekly, and some patients find that scheduling injections at a time when they can monitor symptoms more closely (such as weekends) allows for better symptom management, though this is optional. Ensure you follow the dose escalation schedule recommended by your prescriber and detailed in the Ozempic SmPC—gradual titration allows the gastrointestinal system to adapt and may reduce the severity of side effects, including hiccups.
Hydration is essential but should be managed carefully. Sip water throughout the day rather than consuming large volumes at once, which can contribute to gastric distension. Avoid drinking large amounts immediately before or during meals.
If you experience recurrent hiccups despite these measures, discuss with your healthcare provider whether a temporary dose reduction or slower titration schedule might be appropriate. NICE guidance (NG28) for type 2 diabetes emphasises individualised treatment approaches, and adjustments can often be made without compromising glycaemic control.
Alternative Treatments If Hiccups Persist
When conservative measures fail to resolve hiccups, or if episodes become persistent (>48 hours) or intractable (>1 month), medical evaluation and pharmacological intervention may be necessary.
Clinical assessment should include a thorough history and examination to exclude other causes of persistent hiccups, such as gastro-oesophageal reflux disease (GORD), gastric distension, central nervous system pathology, metabolic disturbances, or medication interactions. Your GP may arrange investigations based on clinical findings, potentially including:
-
Blood tests: To assess electrolytes, renal function, and glucose control
-
Chest X-ray: If diaphragmatic irritation or thoracic pathology is suspected
-
Upper gastrointestinal endoscopy: If reflux or structural abnormalities are suspected
-
Further imaging: Such as CT scans, if clinically indicated
Pharmacological options for persistent hiccups are generally prescribed off-label (not licensed specifically for hiccups) and should be initiated and monitored by a clinician:
-
Metoclopramide: A prokinetic agent that enhances gastric emptying. It may be particularly useful in Ozempic-related hiccups given the underlying delayed gastric emptying. The MHRA restricts use to short courses (≤5 days) due to risk of extrapyramidal side effects and QT prolongation.
-
Baclofen: A GABA-B receptor agonist that suppresses the hiccup reflex centrally. Starting dose is typically 5 mg three times daily, titrated according to response. Sedation, dizziness and falls are potential side effects, particularly in older adults.
-
Gabapentin: May be considered in refractory cases, particularly where neuropathic mechanisms are suspected. Requires careful dose adjustment in renal impairment.
-
Chlorpromazine: Sometimes used in specialist settings with appropriate monitoring for sedation and cardiovascular effects.
-
Proton pump inhibitors (PPIs): If GORD is contributing, a PPI such as omeprazole 20 mg once daily may provide benefit.
Medication review is essential. Your diabetes team should assess whether continuing Ozempic is appropriate or whether switching to an alternative glucose-lowering agent might be considered. Other GLP-1 receptor agonists (such as dulaglutide or liraglutide) have different pharmacokinetic profiles and may be better tolerated. Alternatively, agents from different classes—such as SGLT-2 inhibitors or DPP-4 inhibitors—could be discussed if glycaemic targets allow.
Referral pathways: Persistent hiccups unresponsive to initial management may warrant referral to gastroenterology, neurology, respiratory medicine or ENT depending on suspected underlying causes. Highly specialised interventions such as phrenic nerve blocks are rarely required and only available in certain specialist centres.
Never discontinue Ozempic without consulting your prescriber, as abrupt cessation may affect diabetes control. A collaborative, stepwise approach ensures both symptom relief and continuation of effective metabolic therapy where possible.
Frequently Asked Questions
Why does Ozempic cause hiccups?
Ozempic slows gastric emptying, which may lead to gastric distension and diaphragmatic irritation, potentially triggering hiccups through vagal nerve stimulation. However, hiccups are not listed as an official adverse reaction in UK product information.
When should I see a doctor about Ozempic hiccups?
Seek medical advice if hiccups persist beyond 48 hours, interfere significantly with daily activities, or are accompanied by severe abdominal pain, chest pain, vomiting, difficulty breathing, or neurological symptoms. Contact your GP, NHS 111, or call 999 in emergencies.
Can I prevent hiccups whilst taking Ozempic?
Preventative measures include eating smaller frequent meals, avoiding carbonated beverages and high-fat foods, remaining upright after eating for 2–3 hours, and following the prescribed dose escalation schedule to allow your gastrointestinal system to adapt gradually.
The health-related content published on this site is based on credible scientific sources and is periodically reviewed to ensure accuracy and relevance. Although we aim to reflect the most current medical knowledge, the material is meant for general education and awareness only.
The information on this site is not a substitute for professional medical advice. For any health concerns, please speak with a qualified medical professional. By using this information, you acknowledge responsibility for any decisions made and understand we are not liable for any consequences that may result.
Heading 1
Heading 2
Heading 3
Heading 4
Heading 5
Heading 6
Lorem ipsum dolor sit amet, consectetur adipiscing elit, sed do eiusmod tempor incididunt ut labore et dolore magna aliqua. Ut enim ad minim veniam, quis nostrud exercitation ullamco laboris nisi ut aliquip ex ea commodo consequat. Duis aute irure dolor in reprehenderit in voluptate velit esse cillum dolore eu fugiat nulla pariatur.
Block quote
Ordered list
- Item 1
- Item 2
- Item 3
Unordered list
- Item A
- Item B
- Item C
Bold text
Emphasis
Superscript
Subscript










