Wegovy (semaglutide 2.4 mg) is a GLP-1 receptor agonist licensed in the UK for weight management in adults with obesity or overweight with weight-related comorbidities. Whilst the medication effectively reduces appetite and promotes weight loss, maintaining adequate protein intake during treatment is essential to preserve lean muscle mass and support metabolic health. Without sufficient dietary protein, a significant proportion of weight loss can come from lean tissue rather than fat, potentially compromising physical function and metabolic rate. This article examines evidence-based protein recommendations for individuals taking Wegovy, practical strategies to meet nutritional requirements despite reduced appetite, and the importance of clinical monitoring throughout treatment.
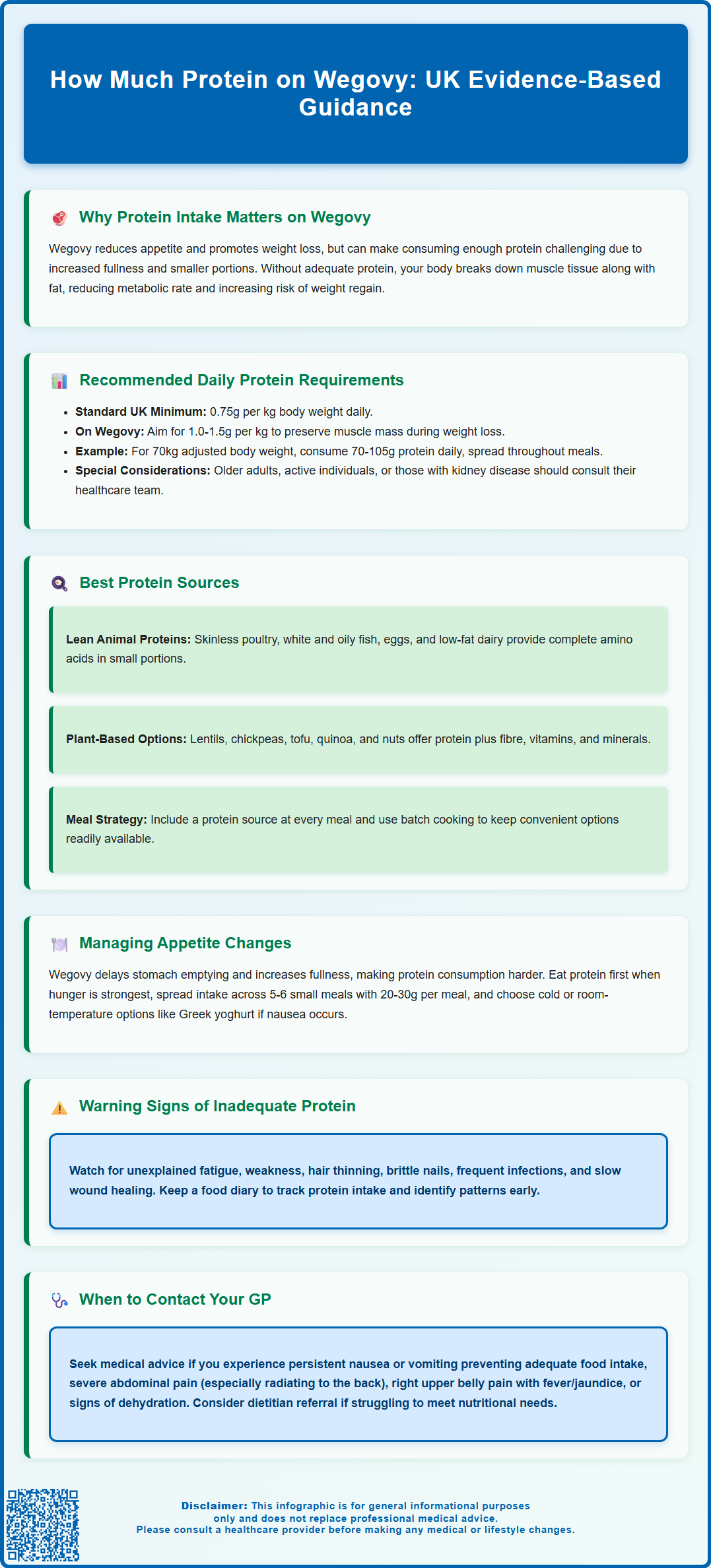
Summary: Adults taking Wegovy typically require 1.0 to 1.5 grams of protein per kilogram of adjusted body weight daily to preserve lean muscle mass during weight loss.
- Wegovy (semaglutide 2.4 mg) is a GLP-1 receptor agonist that reduces appetite by slowing gastric emptying and enhancing satiety signals
- Higher protein intake during weight loss helps preserve lean body mass, maintain metabolic rate, and improve body composition outcomes
- Protein requirements may be adjusted based on age, activity level, rate of weight loss, and presence of comorbidities such as kidney disease
- Lean animal proteins, plant-based sources, and low-fat dairy provide complete amino acids in smaller portions suited to reduced appetite
- Patients should attend regular GP follow-up appointments to monitor nutritional status, manage adverse effects, and assess treatment response
- Referral to a registered dietitian is recommended for those struggling to meet nutritional requirements or experiencing rapid weight loss
Table of Contents
Why Protein Intake Matters When Taking Wegovy
Wegovy (semaglutide 2.4 mg) is a glucagon-like peptide-1 (GLP-1) receptor agonist licensed in the UK for weight management in adults with obesity or overweight with weight-related comorbidities. Whilst the medication effectively reduces appetite and promotes weight loss, maintaining adequate protein intake during treatment is essential to preserve lean muscle mass and support overall metabolic health.
When individuals lose weight, the body naturally breaks down both fat and muscle tissue for energy. Without sufficient dietary protein, a significant proportion of weight loss can come from lean tissue, potentially compromising physical function, reducing metabolic rate, and increasing the risk of weight regain after treatment cessation. Protein plays a crucial role in muscle protein synthesis, immune function, wound healing, and the production of enzymes and hormones.
The mechanism of Wegovy involves slowing gastric emptying (particularly during early treatment), enhancing satiety signals in the brain, and reducing overall food intake. Whilst this promotes a caloric deficit necessary for weight loss, it also creates a risk of inadequate nutrient consumption, particularly protein. Patients may feel full more quickly and for longer periods, making it challenging to meet their nutritional requirements through smaller meal portions.
Clinical evidence suggests that higher protein intake during weight loss interventions helps preserve lean body mass, maintains resting metabolic rate, and improves body composition outcomes. For individuals taking Wegovy, prioritising protein-rich foods becomes an important part of nutritional strategy to optimise treatment benefits whilst minimising potential adverse effects on muscle health and overall wellbeing.
Recommended Daily Protein Requirements on Wegovy
The standard dietary reference value for protein in the UK is 0.75 grams per kilogram of body weight per day for adults, as established by the Scientific Advisory Committee on Nutrition (SACN). This represents the minimum intake to prevent deficiency in healthy adults. However, during active weight loss with Wegovy, protein requirements may need to be higher to support muscle preservation and metabolic function.
Current expert consensus suggests that individuals undergoing weight management may benefit from 1.0 to 1.5 grams of protein per kilogram of body weight daily, with adjustments based on individual factors. For people with obesity, calculations are sometimes based on adjusted body weight rather than actual weight, as this provides a more appropriate target that supports lean tissue maintenance without excessive intake.
For practical application, a person with an adjusted body weight of 70 kg might aim for approximately 70 to 105 grams of protein daily, distributed across meals and snacks. This represents an increase from baseline requirements and may seem challenging given the appetite-suppressing effects of semaglutide.
Individual factors that may influence protein requirements include age (older adults often benefit from higher intakes), activity level, presence of comorbidities, and rate of weight loss. Patients with pre-existing muscle loss (sarcopenia) may require protein at the higher end of the recommended range. Those with kidney disease should discuss protein intake with their healthcare team, as requirements may need modification.
It's important to note that specific protein targets for GLP-1 receptor agonist therapy are still evolving in clinical guidance. Patients should discuss their individual protein requirements with their GP or a registered dietitian who can provide personalised advice. Regular monitoring ensures that dietary adjustments align with both weight loss goals and overall health status.
Best Protein Sources for Wegovy Patients
Selecting high-quality, nutrient-dense protein sources is essential for individuals taking Wegovy, as reduced appetite and smaller meal portions necessitate maximising nutritional value with every bite. Lean protein sources should form the foundation of dietary planning, providing essential amino acids without excessive saturated fat or calories that might hinder weight loss progress.
Animal-based proteins offer complete amino acid profiles and high bioavailability. Recommended options include skinless poultry (chicken, turkey), white fish (cod, haddock, plaice), oily fish (salmon, mackerel, sardines—which also provide omega-3 fatty acids), eggs, low-fat dairy products (Greek yoghurt, cottage cheese, skimmed milk), and lean cuts of red meat consumed in moderation. These foods are particularly valuable as they provide concentrated protein in relatively small serving sizes, which suits the reduced appetite experienced on Wegovy.
Plant-based proteins are equally important and offer additional benefits including fibre, vitamins, minerals, and phytonutrients. Excellent sources include pulses (lentils, chickpeas, black beans, kidney beans), soya products (tofu, tempeh, edamame), quinoa, nuts and seeds (almonds, chia seeds, hemp seeds), and plant-based protein alternatives. A varied plant-based diet throughout the day generally provides all essential amino acids, with soya being a complete protein source.
Protein supplementation may be considered when dietary intake proves insufficient despite best efforts. Whey protein, casein, or plant-based protein powders can be incorporated into smoothies, porridge, or yoghurt. However, whole food sources should remain the priority, as they provide additional nutrients and promote satiety more effectively than isolated supplements.
Patients should aim to include a protein source at each meal and consider protein-rich snacks between meals, in line with the NHS Eatwell Guide recommendations. Practical strategies include meal planning, batch cooking protein-rich foods, and keeping convenient options readily available to overcome appetite fluctuations and ensure consistent intake throughout treatment.
Managing Appetite Changes and Protein Consumption
The appetite-suppressing effects of Wegovy, whilst therapeutically beneficial for weight loss, can create significant challenges in meeting daily protein requirements. Semaglutide's mechanism of action—delaying gastric emptying and enhancing satiety—means patients often experience early fullness, reduced hunger, and sometimes food aversions or nausea, particularly during dose escalation phases.
Practical strategies to optimise protein intake despite reduced appetite include prioritising protein-rich foods at the beginning of meals when hunger is greatest, consuming smaller, more frequent meals throughout the day (five to six occasions rather than three large meals), and choosing protein sources that are well-tolerated and appealing. Many patients find that cold or room-temperature proteins (such as Greek yoghurt, cottage cheese, or chicken salad) are better tolerated than hot, heavy meals when experiencing nausea.
Timing of protein consumption matters significantly. Distributing protein intake evenly across the day (approximately 20-30 grams per meal) optimises muscle protein synthesis more effectively than consuming the majority at one sitting. This approach also helps manage the sensation of fullness that can occur when attempting to consume large portions.
Common adverse effects of Wegovy include nausea (reported in up to 44% of patients), vomiting, diarrhoea, constipation, and abdominal discomfort. These gastrointestinal symptoms can further complicate nutritional intake. Patients experiencing persistent nausea should consider bland, easily digestible protein sources, avoid high-fat preparations that delay gastric emptying further, and ensure adequate hydration.
If symptoms are severe or persistent, patients should consult their prescribing clinician rather than discontinuing treatment independently. Seek urgent medical advice for severe, persistent abdominal pain (especially if radiating to the back), right upper quadrant pain with fever or jaundice, or signs of dehydration. Suspected side effects can be reported via the MHRA Yellow Card Scheme (yellowcard.mhra.gov.uk).
Keeping a food diary can help identify patterns, monitor protein intake, and recognise early signs of nutritional inadequacy. This record proves valuable during consultations with healthcare professionals and enables timely intervention if dietary intake becomes insufficient.
Monitoring Nutritional Health During Wegovy Treatment
Regular monitoring of nutritional status throughout Wegovy treatment is essential to ensure that weight loss occurs in a healthy, sustainable manner whilst preserving lean body mass and preventing micronutrient deficiencies. NICE guidance on obesity management emphasises the importance of ongoing clinical review during pharmacological weight loss interventions.
Clinical monitoring should include regular weight measurements, body composition assessment where available (to distinguish fat loss from muscle loss), and evaluation of dietary intake patterns. Patients should attend scheduled follow-up appointments with their GP or specialist weight management service as per their local pathway and clinical need. These consultations provide opportunities to assess treatment response, manage adverse effects, and address nutritional concerns.
Signs of inadequate protein intake may include unexplained fatigue, weakness, difficulty recovering from exercise, hair thinning or loss, brittle nails, frequent infections, and slow wound healing. Functional assessment (such as grip strength, ability to perform daily activities) and detailed dietary history are often more useful indicators of nutritional status than blood tests alone. Patients experiencing concerning symptoms should contact their GP promptly for assessment.
Blood tests may be indicated to evaluate overall nutritional status, including full blood count, iron studies, vitamin B12, folate, and vitamin D. It's worth noting that serum albumin is not a reliable marker of protein status in outpatient settings, as it's affected by many factors including inflammation and hydration.
Referral to a registered dietitian should be considered for patients struggling to meet nutritional requirements, those with complex dietary needs, individuals with pre-existing nutritional deficiencies, or anyone losing weight at a rate causing clinical concern (typically >1% of body weight per week over several weeks). Dietitians can provide personalised meal planning, practical strategies to optimise protein intake, and ongoing nutritional counselling tailored to individual circumstances.
Patients should be advised to contact their GP if they experience persistent nausea or vomiting preventing adequate food intake, signs of dehydration, severe abdominal pain, or any concerning symptoms. Early intervention can prevent complications and ensure that Wegovy treatment remains both safe and effective. Maintaining open communication with healthcare providers throughout the treatment journey optimises outcomes and supports long-term weight management success.
Frequently Asked Questions
Why is protein intake important when taking Wegovy?
Adequate protein intake during Wegovy treatment helps preserve lean muscle mass during weight loss, maintains metabolic rate, and supports overall health. Without sufficient protein, a significant proportion of weight loss may come from muscle tissue rather than fat, potentially compromising physical function and increasing the risk of weight regain.
What are the best protein sources for people on Wegovy?
High-quality protein sources include lean poultry, white and oily fish, eggs, low-fat dairy (Greek yoghurt, cottage cheese), pulses (lentils, chickpeas), soya products (tofu, tempeh), and nuts and seeds. These provide essential amino acids in smaller portions suited to the reduced appetite experienced on semaglutide.
When should I contact my GP about protein intake on Wegovy?
Contact your GP if you experience persistent nausea or vomiting preventing adequate food intake, unexplained fatigue or weakness, rapid weight loss (typically more than 1% of body weight per week over several weeks), or signs of nutritional deficiency such as hair loss or frequent infections. Early intervention can prevent complications and optimise treatment outcomes.
The health-related content published on this site is based on credible scientific sources and is periodically reviewed to ensure accuracy and relevance. Although we aim to reflect the most current medical knowledge, the material is meant for general education and awareness only.
The information on this site is not a substitute for professional medical advice. For any health concerns, please speak with a qualified medical professional. By using this information, you acknowledge responsibility for any decisions made and understand we are not liable for any consequences that may result.
Heading 1
Heading 2
Heading 3
Heading 4
Heading 5
Heading 6
Lorem ipsum dolor sit amet, consectetur adipiscing elit, sed do eiusmod tempor incididunt ut labore et dolore magna aliqua. Ut enim ad minim veniam, quis nostrud exercitation ullamco laboris nisi ut aliquip ex ea commodo consequat. Duis aute irure dolor in reprehenderit in voluptate velit esse cillum dolore eu fugiat nulla pariatur.
Block quote
Ordered list
- Item 1
- Item 2
- Item 3
Unordered list
- Item A
- Item B
- Item C
Bold text
Emphasis
Superscript
Subscript