Ozempic (semaglutide) is a GLP-1 receptor agonist licensed in the UK for type 2 diabetes management. Whilst the MHRA-approved product information does not list heavy menstrual bleeding as a recognised adverse effect, some women report changes in menstrual patterns during treatment. There is no established direct pharmacological link between semaglutide and increased menstrual flow. However, significant weight loss and metabolic changes may theoretically influence the hypothalamic-pituitary-ovarian axis. If you experience heavy periods whilst taking Ozempic, it is essential to consult your GP to exclude other important causes and determine appropriate management.
Summary: Ozempic (semaglutide) is not recognised as a direct cause of heavy menstrual bleeding, though metabolic changes from treatment may theoretically influence menstrual patterns.
- Semaglutide is a GLP-1 receptor agonist licensed for type 2 diabetes, working primarily on metabolic pathways rather than reproductive hormones.
- The MHRA-approved product information does not list heavy menstrual bleeding as a recognised adverse effect of Ozempic.
- Significant weight loss during treatment may temporarily affect the hypothalamic-pituitary-ovarian axis and menstrual patterns.
- Heavy bleeding warrants GP assessment to exclude other causes including pregnancy, fibroids, hormonal imbalances, and endometrial pathology.
- Management options include levonorgestrel IUS, tranexamic acid, NSAIDs, and hormonal contraception, as recommended by NICE guidelines.
- Do not stop Ozempic without consulting your prescriber, particularly if you have type 2 diabetes requiring glycaemic control.
Table of Contents
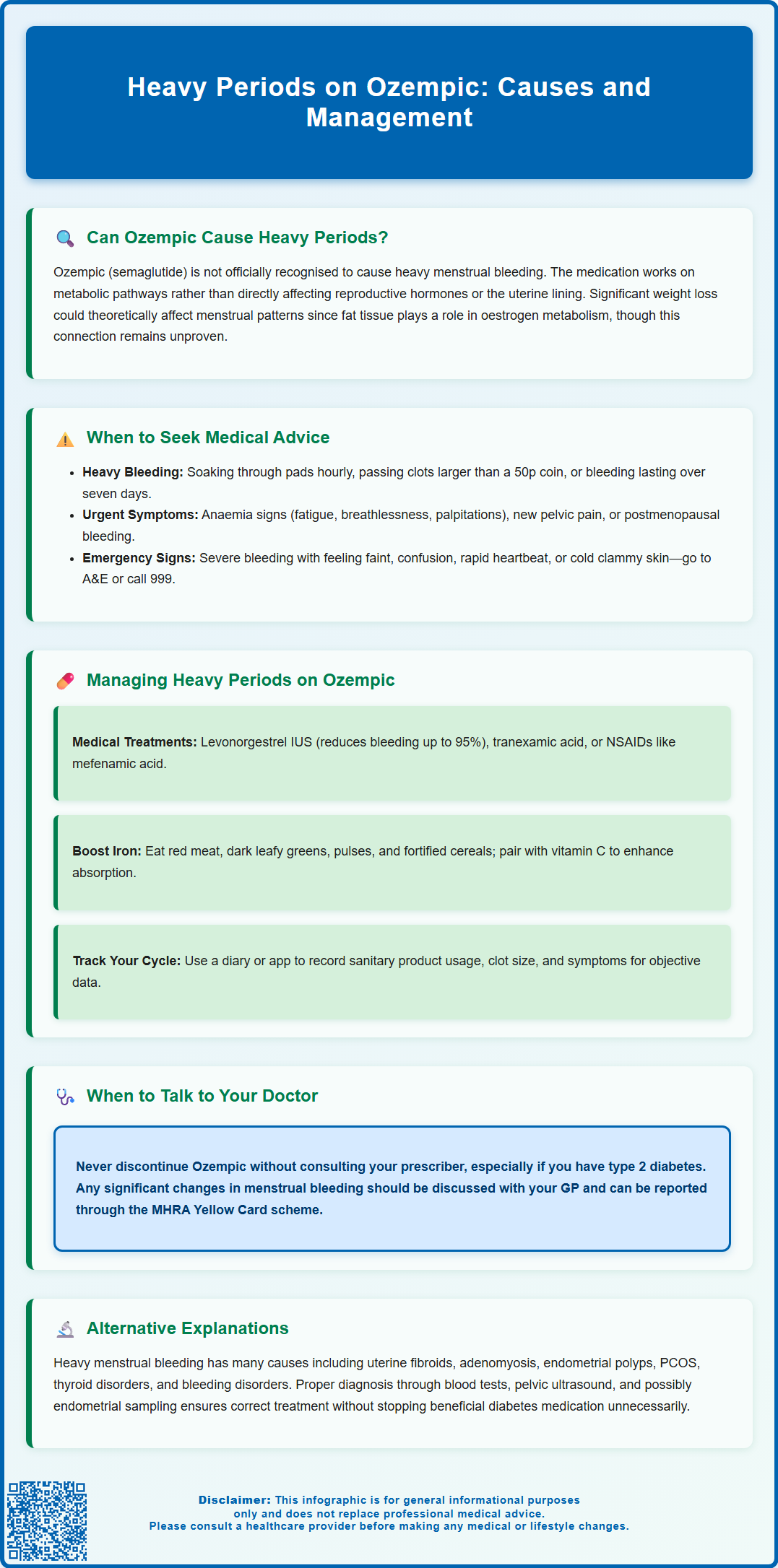
Can Ozempic Cause Heavy Periods?
Ozempic (semaglutide) is a glucagon-like peptide-1 (GLP-1) receptor agonist licensed in the UK for the treatment of type 2 diabetes mellitus. It works by enhancing insulin secretion, suppressing glucagon release, and slowing gastric emptying, which collectively improves glycaemic control and often leads to weight loss. The Medicines and Healthcare products Regulatory Agency (MHRA) approved product information does not list heavy menstrual bleeding (menorrhagia) as a recognised adverse effect of Ozempic.
There is currently no established direct pharmacological link between semaglutide and increased menstrual flow. The drug primarily acts on metabolic pathways rather than directly influencing reproductive hormones or endometrial tissue. However, significant metabolic changes that occur during treatment—particularly substantial weight loss—could theoretically affect menstrual patterns. Adipose tissue plays a role in oestrogen metabolism, and changes in body composition might temporarily influence the hypothalamic-pituitary-ovarian axis, though this remains speculative.
It is essential to recognise that correlation does not imply causation. Women experiencing heavy periods whilst taking Ozempic should consider other potential causes, including pregnancy or early pregnancy complications. The timing of symptom onset in relation to medication initiation should be carefully considered, but other causes must be systematically excluded. If you notice a significant change in your menstrual bleeding pattern after starting Ozempic, this warrants discussion with your GP or prescribing clinician to determine whether further investigation is needed.
If you suspect your medication may be contributing to menstrual changes, you can report this through the MHRA Yellow Card scheme, which helps monitor medication safety.
When to Seek Medical Advice About Heavy Bleeding
Prompt medical assessment is essential if you experience heavy menstrual bleeding, regardless of whether you are taking Ozempic. The National Institute for Health and Care Excellence (NICE) defines heavy menstrual bleeding as excessive menstrual blood loss that interferes with a woman's physical, social, emotional, or material quality of life. Practical indicators include soaking through sanitary protection hourly, passing clots larger than a 50p coin, or bleeding that lasts longer than seven days.
You should contact your GP urgently if you experience:
-
Bleeding so heavy that you soak through your usual sanitary protection every hour for several consecutive hours
-
Passing large blood clots repeatedly
-
Bleeding between periods or after intercourse
-
Symptoms of anaemia, including persistent fatigue, breathlessness, palpitations, or dizziness
-
Pelvic pain or pressure that is new or worsening
-
Any postmenopausal bleeding (bleeding occurring 12 months or more after your last period)
Seek immediate medical attention (attend A&E or call 999) if you experience severe bleeding accompanied by signs of haemodynamic compromise, such as feeling faint, confusion, rapid heartbeat, or cold and clammy skin. These may indicate significant blood loss requiring urgent intervention.
Your GP will take a thorough history, including details about your menstrual cycle, contraception, medications (including Ozempic), and any associated symptoms. They may perform a physical examination and arrange blood tests to check for anaemia. If you are of reproductive age, a pregnancy test will be performed. Additional tests such as thyroid function may be arranged if clinically indicated. Depending on clinical findings, referral to gynaecology services for further investigation, such as pelvic ultrasound or endometrial assessment, may be appropriate according to NICE guidelines.
Managing Heavy Periods While Taking Ozempic
Management of heavy menstrual bleeding should be individualised and address both the underlying cause and symptomatic relief. If you are experiencing heavy periods whilst taking Ozempic, your healthcare team will need to determine whether the medication should be continued, adjusted, or temporarily stopped whilst investigations proceed. This decision depends on the severity of bleeding, the importance of glycaemic control, and whether alternative explanations have been identified. It's important not to stop Ozempic abruptly without consulting your prescriber, particularly if you have type 2 diabetes.
Medical management options for heavy menstrual bleeding, as recommended by NICE, include:
-
Levonorgestrel intrauterine system (LNG-IUS): Often first-line treatment, reducing menstrual blood loss by up to 95% within 12 months
-
Tranexamic acid: An antifibrinolytic agent taken during menstruation to reduce blood loss by 40-50% (caution if you have a history of blood clots)
-
Non-steroidal anti-inflammatory drugs (NSAIDs): Such as mefenamic acid, which can reduce flow by 20-30% and help with associated pain (use with caution if you have gastrointestinal, renal or cardiovascular conditions)
-
Combined hormonal contraception: Can regulate cycles and reduce bleeding in suitable candidates
-
Oral progestogens: Taken cyclically or continuously, depending on individual circumstances
If you currently use a copper intrauterine device (IUD), this can contribute to heavier periods, and switching to a levonorgestrel IUS might be beneficial.
Lifestyle measures may also provide support during this period. Ensuring adequate iron intake through diet or supplementation can help prevent or treat anaemia. Foods rich in iron include red meat, dark green leafy vegetables, pulses, and fortified cereals. Vitamin C enhances iron absorption, so consuming citrus fruits or taking supplements alongside iron-rich meals is beneficial.
Monitoring your symptoms using a menstrual diary or smartphone application can provide valuable information for your healthcare team. Record the number of sanitary products used, clot size, cycle length, and any associated symptoms. This objective data helps guide management decisions and assess treatment response. Continue attending your scheduled diabetes reviews to ensure your glycaemic control remains optimal whilst addressing menstrual concerns.
Alternative Explanations for Changes in Menstrual Flow
Numerous gynaecological and systemic conditions can cause heavy menstrual bleeding, and these must be systematically considered before attributing symptoms to Ozempic. The most common structural causes include uterine fibroids (leiomyomas), adenomyosis, endometrial polyps, and endometrial hyperplasia. Pregnancy complications, including miscarriage or ectopic pregnancy, should be excluded early in the assessment of any change in bleeding pattern.
Hormonal imbalances frequently underlie menstrual irregularities. Polycystic ovary syndrome (PCOS), thyroid disorders (both hypothyroidism and hyperthyroidism), and hyperprolactinaemia can all disrupt normal menstrual patterns. Weight loss itself—whether achieved through medication, diet, or exercise—can temporarily affect menstrual cycles as the body adjusts to metabolic changes and altered hormone levels.
Coagulation disorders should be considered, particularly if heavy periods have been present since menarche or if there is a personal or family history of bleeding problems. Von Willebrand disease is the most prevalent inherited bleeding disorder, though clinically significant cases are less common than the often-quoted 1% prevalence. Medications affecting clotting, such as anticoagulants (including warfarin and direct oral anticoagulants), may also contribute to increased menstrual blood loss.
Contraceptive devices, particularly copper intrauterine devices (IUDs), are known to increase menstrual bleeding and should be considered as potential contributors.
Endometrial pathology, including hyperplasia and malignancy, must be excluded, particularly in women with risk factors such as obesity, diabetes, or unopposed oestrogen exposure. NICE recommends urgent referral (within two weeks) for suspected endometrial cancer in women aged 55 and over with postmenopausal bleeding. For premenopausal women with persistent intermenstrual bleeding, direct access ultrasound and risk-based assessment for further investigation is typically recommended rather than automatic urgent referral.
Comprehensive investigation by your GP or gynaecologist will help identify the underlying cause of heavy bleeding. This typically includes blood tests (full blood count, pregnancy test, and other tests if clinically indicated), pelvic ultrasound, and potentially endometrial sampling depending on age and risk factors. Establishing the correct diagnosis ensures appropriate, targeted treatment rather than unnecessarily discontinuing diabetes medication that may be providing important metabolic benefits.
Frequently Asked Questions
Does Ozempic directly cause heavy menstrual bleeding?
No, there is no established direct pharmacological link between Ozempic (semaglutide) and heavy menstrual bleeding. The MHRA-approved product information does not list menorrhagia as a recognised adverse effect, though metabolic changes from weight loss may theoretically influence menstrual patterns.
When should I see my GP about heavy bleeding whilst taking Ozempic?
Contact your GP urgently if you soak through sanitary protection hourly for several hours, pass large clots repeatedly, experience bleeding between periods, or develop symptoms of anaemia such as fatigue, breathlessness, or dizziness. Seek immediate medical attention if you experience severe bleeding with faintness, confusion, or rapid heartbeat.
What other conditions can cause heavy periods during Ozempic treatment?
Common causes include uterine fibroids, adenomyosis, endometrial polyps, hormonal imbalances (PCOS, thyroid disorders), pregnancy complications, coagulation disorders, and copper IUDs. Your GP will perform comprehensive investigations including blood tests and pelvic ultrasound to identify the underlying cause.
The health-related content published on this site is based on credible scientific sources and is periodically reviewed to ensure accuracy and relevance. Although we aim to reflect the most current medical knowledge, the material is meant for general education and awareness only.
The information on this site is not a substitute for professional medical advice. For any health concerns, please speak with a qualified medical professional. By using this information, you acknowledge responsibility for any decisions made and understand we are not liable for any consequences that may result.
Heading 1
Heading 2
Heading 3
Heading 4
Heading 5
Heading 6
Lorem ipsum dolor sit amet, consectetur adipiscing elit, sed do eiusmod tempor incididunt ut labore et dolore magna aliqua. Ut enim ad minim veniam, quis nostrud exercitation ullamco laboris nisi ut aliquip ex ea commodo consequat. Duis aute irure dolor in reprehenderit in voluptate velit esse cillum dolore eu fugiat nulla pariatur.
Block quote
Ordered list
- Item 1
- Item 2
- Item 3
Unordered list
- Item A
- Item B
- Item C
Bold text
Emphasis
Superscript
Subscript