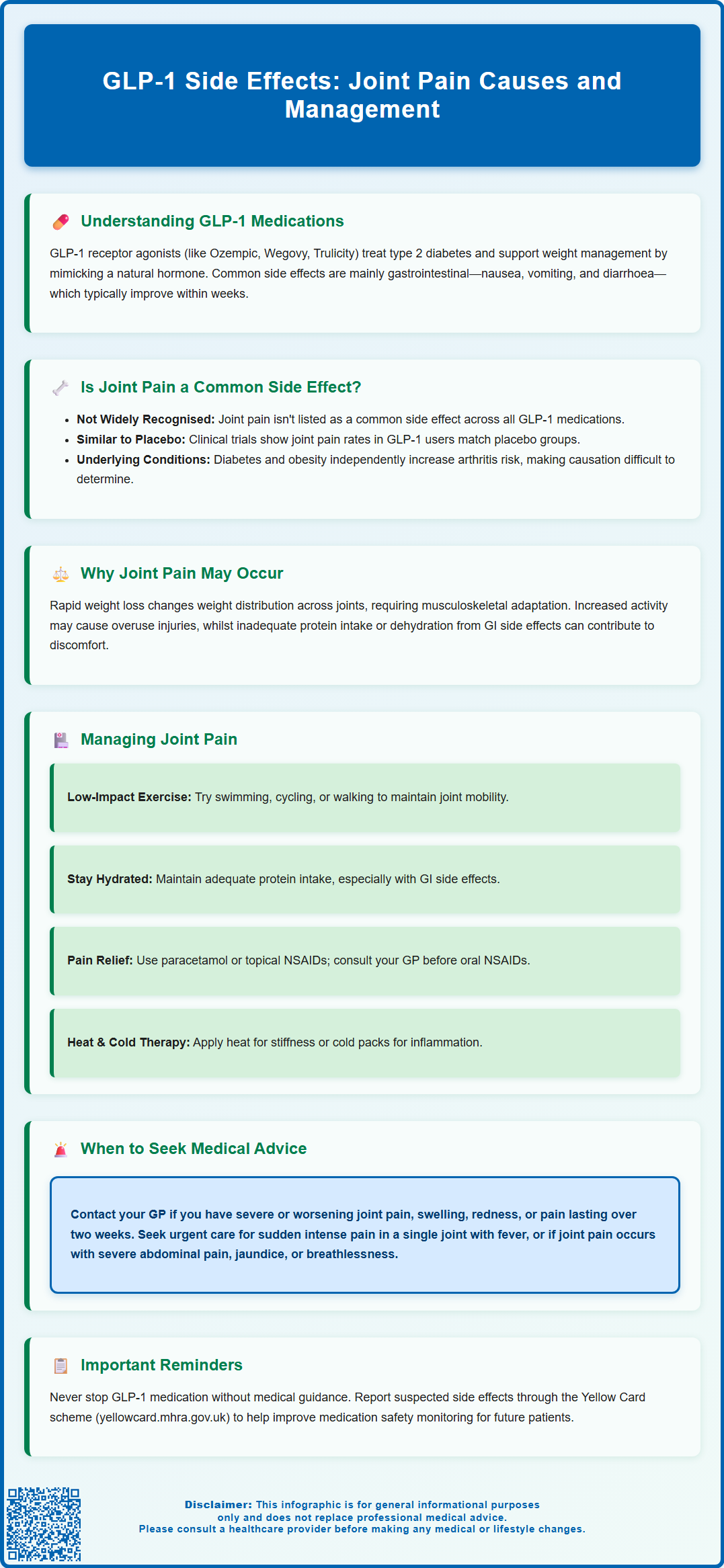
GLP-1 receptor agonists, including semaglutide (Ozempic, Wegovy), dulaglutide (Trulicity), and liraglutide (Victoza, Saxenda), are widely prescribed in the UK for type 2 diabetes and weight management. Whilst gastrointestinal side effects such as nausea and diarrhoea are well-recognised, some patients report joint pain during treatment. Joint pain is not a common class-wide side effect of GLP-1 medications, though musculoskeletal symptoms appear in certain product summaries. This article examines the relationship between GLP-1 agonists and joint pain, explores potential contributing factors such as rapid weight loss and increased activity, and provides guidance on managing symptoms and recognising when medical review is needed.
Summary: Joint pain is not a common class-wide side effect of GLP-1 receptor agonists, though musculoskeletal symptoms are listed in some product summaries with varying frequency.
- GLP-1 agonists primarily cause gastrointestinal side effects; arthralgia incidence in trials is generally similar to placebo
- Rapid weight loss from GLP-1 treatment may alter biomechanical loading on joints, causing temporary adjustment-related discomfort
- Patients prescribed GLP-1 medications often have type 2 diabetes or obesity, conditions independently associated with increased osteoarthritis rates
- Seek medical advice for severe, worsening, or persistent joint pain, or if accompanied by swelling, redness, warmth, or systemic symptoms
- Report suspected medication side effects through the MHRA Yellow Card scheme to support ongoing safety monitoring
Table of Contents
Understanding GLP-1 Medications and Their Common Side Effects
Glucagon-like peptide-1 (GLP-1) receptor agonists represent a class of medications prescribed in the UK for managing type 2 diabetes and, in specific formulations, for weight management. For type 2 diabetes, these include semaglutide (Ozempic), dulaglutide (Trulicity), liraglutide (Victoza), and exenatide (Byetta, Bydureon). For weight management, only semaglutide (Wegovy) and liraglutide (Saxenda) are specifically licensed in the UK. GLP-1 agonists work by mimicking a naturally occurring hormone that regulates blood glucose levels, enhances insulin secretion when blood sugar is elevated, suppresses glucagon release, and slows gastric emptying.
The mechanism of action makes GLP-1 medications highly effective for glycaemic control and weight reduction. However, as with all pharmaceutical interventions, they are associated with a range of side effects. The most commonly reported adverse effects are gastrointestinal in nature, affecting a significant proportion of patients, particularly during the initial weeks of treatment or following dose escalation.
Common gastrointestinal side effects include:
-
Nausea and vomiting
-
Diarrhoea or constipation
-
Abdominal pain and bloating
-
Reduced appetite
-
Indigestion
These effects typically diminish as the body adjusts to the medication, usually within several weeks. Other recognised side effects include injection site reactions, fatigue, dizziness, and headache. More serious but rare adverse events include pancreatitis, gallbladder disease, and thyroid C-cell tumours (patients should be advised to report symptoms such as neck mass, dysphagia or persistent hoarseness).
Important safety considerations include the risk of hypoglycaemia when combined with insulin or sulfonylureas, potential dehydration and acute kidney injury with severe gastrointestinal symptoms, and for semaglutide specifically, possible worsening of diabetic retinopathy in those with pre-existing disease. The MHRA, NICE and NHS provide comprehensive guidance on the safe prescribing and monitoring of GLP-1 agonists, emphasising the importance of patient education regarding expected side effects and warning signs that warrant medical attention.
Can GLP-1 Agonists Cause Joint Pain?
Joint pain (arthralgia) is not generally recognised as a common class-wide side effect of GLP-1 receptor agonists, though individual product profiles vary. The established adverse effect profile, based on clinical trial data submitted to regulatory authorities such as the MHRA and EMA, predominantly features gastrointestinal symptoms.
However, musculoskeletal symptoms including arthralgia are listed in some product SmPCs with varying frequencies. For example, back pain and musculoskeletal discomfort appear in certain GLP-1 agonist SmPCs as uncommon or common adverse reactions. The frequency and reporting of these symptoms differ between individual medications within the class, so it's important to consult the specific SmPC for the prescribed product.
Clinical trials for GLP-1 agonists have reported musculoskeletal side effects such as back pain and muscle pain in a small percentage of participants, but joint pain specifically has not emerged as a consistent or significant adverse event across the class. The incidence of arthralgia in many trial populations taking GLP-1 medications has generally been similar to placebo groups, though this varies by product.
Patients prescribed GLP-1 agonists often have type 2 diabetes or obesity, conditions independently associated with increased rates of osteoarthritis and other musculoskeletal disorders. This makes it challenging to determine whether joint pain is a medication side effect or related to underlying health conditions. Concomitant medications may also contribute to musculoskeletal symptoms. Healthcare professionals should maintain awareness of patient-reported symptoms whilst recognising the complex relationship between GLP-1 agonists, their therapeutic effects, and joint symptoms.
Why Joint Pain May Occur During GLP-1 Treatment
Whilst there is no established direct mechanism by which GLP-1 receptor agonists consistently cause joint pain, several indirect factors may explain why some patients experience musculoskeletal discomfort during treatment. Understanding these potential contributing factors helps contextualise patient experiences and guides appropriate management.
Rapid weight loss is one of the most significant indirect factors. GLP-1 medications, particularly at higher doses used for weight management, can lead to substantial weight reduction. This weight loss alters biomechanical loading patterns on joints, particularly weight-bearing joints such as the knees, hips, and ankles. As body composition changes, the musculoskeletal system must adapt to new movement patterns and weight distribution, which may temporarily cause discomfort or pain. Paradoxically, whilst long-term weight loss typically improves joint health and reduces osteoarthritis symptoms (as noted in NICE NG226), the transition period may be associated with adjustment-related discomfort.
Changes in physical activity levels often accompany GLP-1 treatment. Patients who lose weight may become more active or undertake new exercise regimens, potentially leading to overuse injuries or delayed-onset muscle soreness that may be perceived as joint pain. Conversely, some patients may experience fatigue as a side effect, leading to reduced activity and subsequent joint stiffness.
Nutritional factors may play a role. Significant appetite suppression and reduced food intake should be managed with a balanced diet containing adequate protein per NHS guidance. Dehydration, which can occur with gastrointestinal side effects such as vomiting or diarrhoea, may also contribute to joint discomfort.
Pre-existing musculoskeletal conditions are common in the patient population prescribed GLP-1 agonists. Individuals with type 2 diabetes have higher rates of osteoarthritis, and obesity itself is a major risk factor for joint disease. Weight loss can also occasionally trigger gout flares (as noted in NICE NG219), which may present as acute joint pain, particularly in a single joint.
Managing Joint Pain While Taking GLP-1 Medications
If you experience joint pain whilst taking a GLP-1 medication, several practical strategies may help manage symptoms whilst you continue your prescribed treatment. It is important to discuss any new or worsening symptoms with your healthcare provider to ensure appropriate assessment and management.
Self-care measures for mild joint discomfort include:
-
Gentle, regular exercise: Low-impact activities such as swimming, cycling, or walking can maintain joint mobility without excessive stress. Physiotherapy-guided exercises may strengthen supporting muscles and improve joint stability.
-
Adequate hydration and nutrition: Ensure sufficient fluid intake, particularly if experiencing gastrointestinal side effects. Maintain adequate protein intake to support muscle and connective tissue health.
-
Gradual activity progression: If increasing physical activity following weight loss, do so gradually to allow joints and muscles time to adapt to new demands.
-
Weight management monitoring: Work with your healthcare team to ensure weight loss occurs at a sustainable pace, typically 0.5–1 kg per week, which may reduce biomechanical stress on joints.
-
Pain relief options: Paracetamol may be used for mild pain relief, following package instructions. Topical NSAIDs (such as ibuprofen gel) are recommended by NICE as first-line for localised joint pain. Oral non-steroidal anti-inflammatory drugs (NSAIDs) such as ibuprofen may be considered for short-term use, but discuss with your GP or pharmacist first, particularly if you have diabetes-related kidney concerns, heart disease, or gastrointestinal risks.
Application of heat or cold therapy to affected joints may provide symptomatic relief. Heat can ease stiffness, whilst cold packs may reduce inflammation and swelling.
Medication review with your prescriber is essential if joint pain is significant or persistent. Your doctor may consider whether dose adjustment, temporary treatment interruption, or investigation for alternative causes is appropriate. Do not stop or alter your GLP-1 medication without medical guidance, as this may affect your diabetes control or weight management goals. Your healthcare team can help distinguish between medication-related effects and other causes of joint pain, ensuring you receive appropriate treatment whilst maintaining the benefits of GLP-1 therapy.
When to Seek Medical Advice About Joint Pain on GLP-1s
Whilst mild, transient joint discomfort may not require urgent medical attention, certain features of joint pain warrant prompt evaluation by your GP or healthcare provider. Recognising warning signs helps ensure timely diagnosis and management of potentially serious conditions.
Contact your GP or healthcare provider if you experience:
-
Severe or worsening joint pain that interferes with daily activities or does not improve with simple measures
-
Joint swelling, redness, or warmth, which may indicate inflammation or infection
-
Sudden onset of intense pain in a single joint, particularly if accompanied by fever (may require same-day assessment to exclude septic arthritis or gout)
-
Joint pain associated with systemic symptoms such as unexplained fever, weight loss (beyond expected treatment effects), rash, or general malaise
-
Persistent pain lasting more than two weeks despite self-care measures
-
Joint stiffness lasting more than 30 minutes after waking, which may suggest inflammatory arthritis
-
Reduced range of motion or inability to bear weight on affected joints
Seek urgent medical attention (contact 111 or attend A&E) if:
-
Joint pain is accompanied by severe abdominal pain, persistent vomiting, or signs of pancreatitis (if pancreatitis is suspected, stop your GLP-1 medication immediately; if confirmed, the medication should not be restarted)
-
You develop right-upper abdominal pain, jaundice (yellowing of skin/eyes), pale stools or dark urine (possible gallbladder disease)
-
You develop chest pain, severe breathlessness, or signs of allergic reaction
-
Joint pain follows trauma or injury with suspected fracture
Your healthcare provider may undertake investigations including blood tests (inflammatory markers, rheumatoid factor, uric acid), X-rays, or referral to rheumatology if inflammatory arthritis is suspected. They will also review your complete medication list, as drug interactions or other medications may contribute to musculoskeletal symptoms.
Maintaining open communication with your diabetes team or prescriber ensures that any side effects are properly documented and managed. If you suspect your medication is causing side effects, you can report them through the Yellow Card scheme (yellowcard.mhra.gov.uk), operated by the MHRA. This helps contribute to ongoing medication safety monitoring and benefits future patients.
Frequently Asked Questions
Do GLP-1 medications commonly cause joint pain?
Joint pain is not a common class-wide side effect of GLP-1 receptor agonists. Clinical trial data shows arthralgia incidence is generally similar to placebo, though some musculoskeletal symptoms appear in certain product summaries with varying frequency.
Why might I experience joint pain whilst taking a GLP-1 medication?
Joint pain during GLP-1 treatment may result from rapid weight loss altering biomechanical loading on joints, increased physical activity levels, or pre-existing musculoskeletal conditions such as osteoarthritis, which are common in people with type 2 diabetes or obesity.
When should I contact my GP about joint pain on GLP-1 treatment?
Contact your GP if you experience severe or worsening joint pain, joint swelling or redness, sudden intense pain in a single joint, persistent pain lasting more than two weeks, or joint stiffness lasting over 30 minutes after waking.
The health-related content published on this site is based on credible scientific sources and is periodically reviewed to ensure accuracy and relevance. Although we aim to reflect the most current medical knowledge, the material is meant for general education and awareness only.
The information on this site is not a substitute for professional medical advice. For any health concerns, please speak with a qualified medical professional. By using this information, you acknowledge responsibility for any decisions made and understand we are not liable for any consequences that may result.
Heading 1
Heading 2
Heading 3
Heading 4
Heading 5
Heading 6
Lorem ipsum dolor sit amet, consectetur adipiscing elit, sed do eiusmod tempor incididunt ut labore et dolore magna aliqua. Ut enim ad minim veniam, quis nostrud exercitation ullamco laboris nisi ut aliquip ex ea commodo consequat. Duis aute irure dolor in reprehenderit in voluptate velit esse cillum dolore eu fugiat nulla pariatur.
Block quote
Ordered list
- Item 1
- Item 2
- Item 3
Unordered list
- Item A
- Item B
- Item C
Bold text
Emphasis
Superscript
Subscript