GLP-1 receptor agonists for non-alcoholic fatty liver disease (NAFLD) represent an emerging area of clinical interest in the UK. Whilst these medications are not currently licensed specifically for liver disease, growing evidence suggests they may reduce hepatic fat and improve metabolic parameters in patients with NAFLD. This article examines how GLP-1 therapies work, the clinical evidence supporting their use, current prescribing criteria within NHS pathways, and essential monitoring considerations for patients with concurrent metabolic and liver conditions. Understanding the role of GLP-1 agonists in NAFLD management is increasingly relevant given the condition's high prevalence and limited pharmacological treatment options.
Summary: GLP-1 receptor agonists are not licensed for NAFLD treatment in the UK but may reduce liver fat and improve metabolic parameters when prescribed for type 2 diabetes or weight management in eligible patients with concurrent liver disease.
- GLP-1 agonists work primarily through weight loss, improved insulin sensitivity, and reduced hepatic lipogenesis rather than direct liver receptor activation.
- Clinical trials demonstrate significant reductions in hepatic steatosis with semaglutide and liraglutide, though fibrosis improvement remains modest.
- UK prescribing is restricted to licensed indications: type 2 diabetes management or weight management in patients meeting specific BMI and comorbidity criteria.
- Monitoring requires baseline and ongoing liver function tests, FIB-4 scoring for fibrosis risk, and vigilance for pancreatitis and gallbladder disease.
- Referral to specialist hepatology services is recommended for patients with elevated ELF scores (≥10.51) or evidence of advanced fibrosis.
Table of Contents
What Is Non-Alcoholic Fatty Liver Disease (NAFLD)?
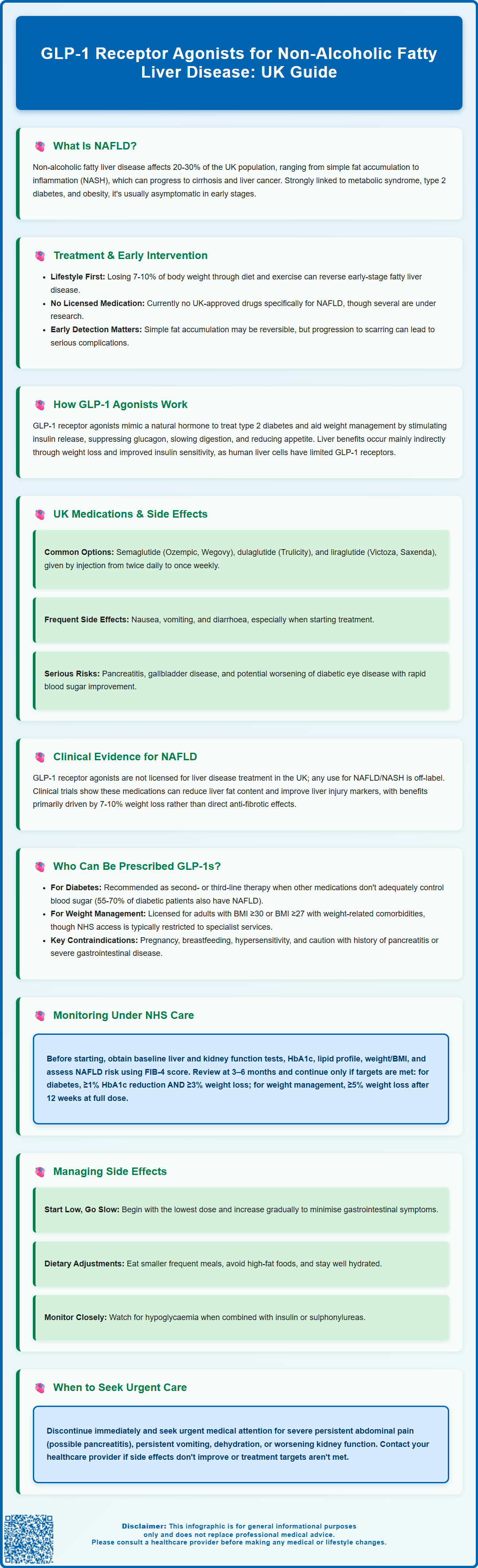
Non-alcoholic fatty liver disease (NAFLD) is a common condition characterised by excessive fat accumulation in the liver of individuals who consume little to no alcohol (typically defined as less than 14 units per week in the UK). It represents a spectrum of liver pathology, ranging from simple steatosis (fat accumulation without inflammation) to non-alcoholic steatohepatitis (NASH), which involves inflammation and hepatocyte damage. NASH can progress to fibrosis, cirrhosis, and in some cases, particularly those with advanced fibrosis or cirrhosis, to hepatocellular carcinoma.
NAFLD affects approximately 20–30% of the UK population and is strongly associated with metabolic syndrome, type 2 diabetes, obesity, and insulin resistance. The condition is often asymptomatic in its early stages, typically discovered incidentally through abnormal liver function tests or imaging studies. Risk factors include central obesity, dyslipidaemia, hypertension, and sedentary lifestyle.
The pathophysiology of NAFLD involves complex interactions between insulin resistance, lipotoxicity, oxidative stress, and inflammatory pathways. Excess hepatic fat accumulation triggers a cascade of metabolic disturbances that can impair liver function over time. Early identification and intervention are crucial, as simple steatosis may be reversible with lifestyle modifications.
It is worth noting that the terminology is evolving, with metabolic dysfunction-associated steatotic liver disease (MASLD) increasingly being used alongside NAFLD in clinical practice.
Currently, NICE guidance (NG49) emphasises lifestyle intervention as the cornerstone of NAFLD management, including weight loss of 7–10% of body weight, increased physical activity, and dietary modification. However, achieving and maintaining such weight loss proves challenging for many patients, prompting interest in pharmacological interventions that address both metabolic dysfunction and liver pathology. There is no licensed pharmacological treatment specifically for NAFLD in the UK at present, though several therapeutic approaches are under investigation.
How GLP-1 Receptor Agonists Work in the Body
Glucagon-like peptide-1 (GLP-1) receptor agonists are a class of medications that mimic the action of the naturally occurring incretin hormone GLP-1. These agents bind to and activate GLP-1 receptors, which are expressed in multiple tissues including the pancreas, gastrointestinal tract, and brain. The primary therapeutic indication for GLP-1 agonists in the UK is type 2 diabetes management, with some formulations also licensed for weight management.
The mechanism of action involves several complementary pathways. In the pancreas, GLP-1 receptor activation stimulates glucose-dependent insulin secretion from beta cells whilst suppressing inappropriate glucagon release from alpha cells. This dual action improves glycaemic control without significantly increasing hypoglycaemia risk. In the gastrointestinal system, these medications slow gastric emptying and reduce appetite through central nervous system pathways, contributing to weight loss.
Hepatic effects of GLP-1 receptor agonists are increasingly recognised as clinically significant. These medications appear to reduce hepatic steatosis primarily through indirect mechanisms: improved insulin sensitivity reduces hepatic glucose production and lipogenesis; weight loss decreases overall fat deposition. While direct hepatic effects have been proposed, human hepatocyte GLP-1 receptor expression is limited, and most hepatic benefits correlate with weight loss and improved metabolic parameters rather than direct receptor-mediated effects.
Commonly prescribed GLP-1 receptor agonists in the UK include semaglutide (Ozempic, Wegovy, Rybelsus [oral formulation for diabetes only]), dulaglutide (Trulicity), liraglutide (Victoza, Saxenda), and exenatide (Byetta, Bydureon). Most are administered via subcutaneous injection, with dosing frequencies ranging from twice daily to once weekly depending on the specific formulation.
The medications are generally well-tolerated, though gastrointestinal side effects such as nausea, vomiting, and diarrhoea are common, particularly during dose titration. Important safety considerations include risk of pancreatitis (treatment should be discontinued if suspected), gallbladder disease, and potential worsening of diabetic retinopathy in patients with pre-existing retinopathy who experience rapid improvement in glucose control (particularly with semaglutide).
Clinical Evidence: GLP-1 Treatment for NAFLD in the UK
Emerging clinical evidence suggests GLP-1 receptor agonists may offer therapeutic benefits for patients with NAFLD and NASH, though it is important to note that these medications are not currently licensed specifically for liver disease treatment in the UK. Any use for NAFLD/NASH would be considered off-label. The evidence base derives primarily from clinical trials examining metabolic outcomes in patients with type 2 diabetes or obesity, many of whom had concurrent NAFLD.
Several randomised controlled trials have demonstrated that GLP-1 agonists can reduce liver fat content and improve biochemical markers of liver injury. Studies using magnetic resonance imaging (MRI) and proton density fat fraction (MRI-PDFF) measurements have shown significant reductions in hepatic steatosis with semaglutide and liraglutide treatment. The phase 2 semaglutide NASH trial (published in NEJM, 2021) demonstrated NASH resolution in a significant proportion of patients, though fibrosis improvement was modest. The LEAN trial showed liraglutide's potential benefits in NASH patients.
The weight loss achieved with GLP-1 therapy appears central to hepatic benefits, as weight reduction of 7–10% consistently improves NAFLD across multiple intervention studies. Most hepatic improvements correlate with the degree of weight loss, with limited evidence for weight-independent antifibrotic effects. Preliminary data suggest potential anti-inflammatory effects, but these findings require further validation.
Current UK guidance does not specifically recommend GLP-1 agonists for NAFLD treatment outside their licensed indications. NICE guidelines for NAFLD management (NG49) focus on lifestyle modification and treatment of associated metabolic conditions. However, when patients with NAFLD also have type 2 diabetes or meet criteria for weight management therapy, GLP-1 agonists prescribed for these licensed indications may confer additional hepatic benefits. Clinicians should follow MHRA-approved prescribing indications and discuss potential benefits and limitations with patients. Ongoing clinical trials, including studies specifically examining NASH outcomes, may inform future prescribing guidance.
Who Can Be Prescribed GLP-1 Agonists for Liver Health?
In the UK, GLP-1 receptor agonists cannot currently be prescribed solely for NAFLD or NASH treatment, as they lack specific licensing for liver disease indications. However, many patients with NAFLD have comorbid conditions for which these medications are appropriately indicated, potentially providing dual metabolic and hepatic benefits.
For type 2 diabetes management, NICE guidance (NG28) recommends GLP-1 agonists as second- or third-line therapy when metformin and other oral agents provide inadequate glycaemic control, or as an alternative to insulin in appropriate patients. Given the high prevalence of NAFLD among people with type 2 diabetes (estimated at 55–70%), many patients receiving GLP-1 therapy for diabetes will have concurrent liver disease.
For weight management, certain GLP-1 formulations (liraglutide 3.0mg [Saxenda] and semaglutide 2.4mg [Wegovy]) are licensed for chronic weight management in adults with:
-
BMI ≥30 kg/m², or
-
BMI ≥27 kg/m² with at least one weight-related comorbidity (such as type 2 diabetes, hypertension, or dyslipidaemia)
However, NHS access to these medications for weight management is typically restricted to specialist tier 3 or tier 4 weight management services, with specific eligibility criteria defined by NICE technology appraisals (TA494 for liraglutide, TA664 for semaglutide) and local commissioning arrangements. Patients must typically demonstrate commitment to lifestyle modification and meet specific clinical criteria.
Contraindications according to UK SmPCs include hypersensitivity to the active substance or any excipients. Cautions and precautions include:
-
History of pancreatitis (discontinue if pancreatitis is suspected)
-
Type 1 diabetes or diabetic ketoacidosis (not indicated)
-
Severe gastrointestinal disease including gastroparesis
-
Gallbladder disease (increased risk with GLP-1 therapy)
-
Diabetic retinopathy (monitor for worsening with rapid glycaemic improvement, particularly with semaglutide)
Regarding renal impairment, most GLP-1 agonists (semaglutide, liraglutide, dulaglutide) require no dose adjustment. Exenatide is not recommended in severe renal impairment (eGFR <30 mL/min/1.73 m²) and should be used with caution at eGFR 30–50 mL/min/1.73 m².
Pregnancy and breastfeeding are contraindications. Prescribing decisions should involve shared decision-making, considering individual patient circumstances, comorbidities, and treatment goals. Referral to specialist hepatology services may be appropriate for patients with advanced liver disease or diagnostic uncertainty.
Monitoring and Managing Treatment Under NHS Care
Patients receiving GLP-1 receptor agonists require structured monitoring to ensure treatment safety, efficacy, and appropriate continuation. Monitoring protocols should address both the primary indication (diabetes or weight management) and potential hepatic effects, particularly in patients with known or suspected NAFLD.
Baseline assessment before initiating GLP-1 therapy should include:
-
Liver function tests (ALT, AST, GGT, ALP, bilirubin) to establish baseline hepatic status
-
Renal function (eGFR, creatinine)
-
HbA1c and fasting glucose for diabetes management
-
Lipid profile to assess cardiovascular risk
-
Body weight and BMI to track treatment response
-
Blood pressure measurement
-
NAFLD risk stratification using age-adjusted FIB-4 score in primary care; if indeterminate/high, consider FibroScan or Enhanced Liver Fibrosis (ELF) test
Ongoing monitoring typically involves:
- Review at 3–6 months to assess treatment response, tolerability, and continuation criteria
- For diabetes, NICE NG28 specifies continuation if there is ≥11 mmol/mol (1%) reduction in HbA1c AND ≥3% weight loss at 6 months
-
For weight management, product-specific criteria apply: for liraglutide (Saxenda), discontinue if <5% weight loss after 12 weeks at 3mg daily; for semaglutide (Wegovy), evaluate response once maintenance dose is reached
-
Six-monthly reviews thereafter, including liver function tests, renal function, and metabolic parameters
-
Annual comprehensive review including cardiovascular risk assessment
-
NAFLD monitoring may include repeat FIB-4 or ELF testing; referral to hepatology is recommended if ELF score ≥10.51 or other evidence of advanced fibrosis
Managing adverse effects is crucial for treatment adherence. Gastrointestinal symptoms (nausea, vomiting, diarrhoea) are most common, typically improving with gradual dose titration. Patients should be advised to:
-
Start with the lowest dose and increase slowly
-
Eat smaller, more frequent meals
-
Avoid high-fat foods
-
Stay well-hydrated
Safety monitoring should include vigilance for:
-
Pancreatitis symptoms (severe persistent abdominal pain) — discontinue immediately if suspected
-
Gallbladder disease — increased risk with rapid weight loss
-
Hypoglycaemia — particularly when combined with insulin or sulphonylureas
-
Renal function deterioration — especially with dehydration from gastrointestinal effects
-
Diabetic retinopathy — monitor in patients with pre-existing retinopathy, particularly with semaglutide
Suspected adverse reactions should be reported via the MHRA Yellow Card scheme.
When to seek urgent medical advice: Patients should contact their GP or seek emergency care if they experience severe abdominal pain, persistent vomiting, signs of dehydration, or symptoms of pancreatitis. For NAFLD-specific monitoring, patients with established liver disease may require additional specialist hepatology input, including non-invasive fibrosis assessment and consideration for liver imaging. Treatment decisions should be regularly reviewed to ensure ongoing clinical benefit and appropriate resource utilisation within NHS care pathways.
Frequently Asked Questions
Can GLP-1 agonists be prescribed specifically for NAFLD in the UK?
No, GLP-1 receptor agonists are not currently licensed for NAFLD treatment in the UK. They may only be prescribed for approved indications such as type 2 diabetes or weight management, though patients with NAFLD meeting these criteria may experience additional hepatic benefits.
How do GLP-1 medications improve liver fat in NAFLD patients?
GLP-1 agonists reduce hepatic steatosis primarily through weight loss, improved insulin sensitivity, and decreased hepatic glucose production and lipogenesis. Most hepatic benefits correlate with the degree of weight loss achieved rather than direct liver receptor effects.
What monitoring is required for NAFLD patients on GLP-1 therapy?
Monitoring includes baseline and six-monthly liver function tests, NAFLD fibrosis risk stratification using FIB-4 score, and assessment for complications such as pancreatitis and gallbladder disease. Patients with elevated fibrosis scores should be referred to specialist hepatology services.
The health-related content published on this site is based on credible scientific sources and is periodically reviewed to ensure accuracy and relevance. Although we aim to reflect the most current medical knowledge, the material is meant for general education and awareness only.
The information on this site is not a substitute for professional medical advice. For any health concerns, please speak with a qualified medical professional. By using this information, you acknowledge responsibility for any decisions made and understand we are not liable for any consequences that may result.
Heading 1
Heading 2
Heading 3
Heading 4
Heading 5
Heading 6
Lorem ipsum dolor sit amet, consectetur adipiscing elit, sed do eiusmod tempor incididunt ut labore et dolore magna aliqua. Ut enim ad minim veniam, quis nostrud exercitation ullamco laboris nisi ut aliquip ex ea commodo consequat. Duis aute irure dolor in reprehenderit in voluptate velit esse cillum dolore eu fugiat nulla pariatur.
Block quote
Ordered list
- Item 1
- Item 2
- Item 3
Unordered list
- Item A
- Item B
- Item C
Bold text
Emphasis
Superscript
Subscript