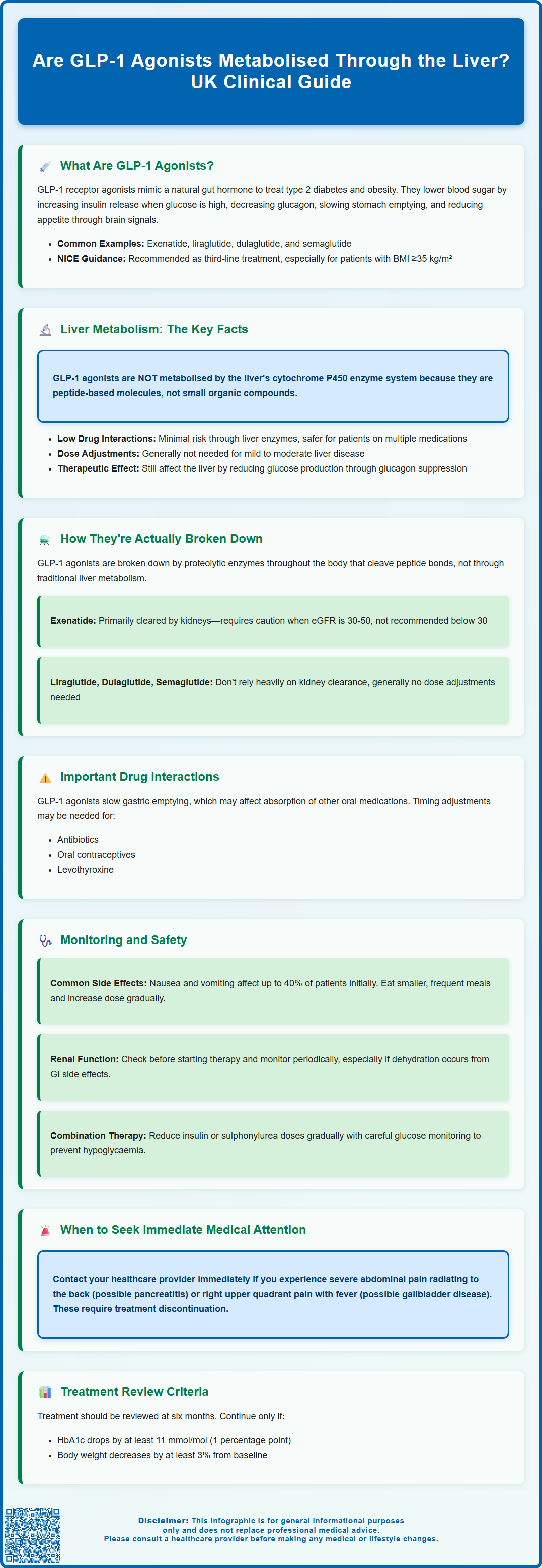
Are GLP-1 agonists metabolised through the liver? This is a common question amongst healthcare professionals and patients alike, particularly when considering prescribing for individuals with hepatic impairment or complex medication regimens. Unlike many oral medications, GLP-1 receptor agonists—including exenatide, liraglutide, dulaglutide, and semaglutide—are peptide-based drugs that bypass traditional hepatic cytochrome P450 metabolism. Instead, they undergo proteolytic degradation throughout the body. Understanding this unique metabolic pathway is essential for safe prescribing, minimising drug interactions, and optimising treatment in patients with type 2 diabetes and obesity. This article explores how GLP-1 agonists are broken down, their clinical implications, and key monitoring considerations aligned with UK guidance.
Summary: GLP-1 agonists are not primarily metabolised through the liver via cytochrome P450 enzymes; instead, they undergo proteolytic degradation throughout the body.
- GLP-1 agonists are peptide-based medications that bypass hepatic cytochrome P450 metabolism, reducing potential for drug-drug interactions.
- These agents are broken down by ubiquitous proteolytic enzymes throughout the body into smaller peptides and amino acids.
- Dose adjustments are generally not required in mild to moderate hepatic impairment, though caution is advised in severe liver disease.
- Exenatide is predominantly cleared renally and requires dose adjustment in renal impairment, whilst liraglutide, dulaglutide, and semaglutide do not.
- Common adverse effects include gastrointestinal symptoms; serious but rare complications include pancreatitis and gallbladder disease requiring clinical monitoring.
- NICE recommends reviewing GLP-1 therapy at six months and continuing only if beneficial metabolic response and weight loss are achieved.
Table of Contents
What Are GLP-1 Agonists and How Do They Work?
Glucagon-like peptide-1 (GLP-1) receptor agonists are a class of medications primarily used to manage type 2 diabetes mellitus and, more recently, obesity. These agents mimic the action of naturally occurring GLP-1, an incretin hormone released from the intestinal L-cells in response to food intake. The endogenous hormone plays a crucial role in glucose homeostasis, but it is rapidly degraded by the enzyme dipeptidyl peptidase-4 (DPP-4), limiting its therapeutic potential.
GLP-1 agonists have been structurally modified to resist enzymatic degradation, thereby extending their duration of action. Examples include exenatide, liraglutide, dulaglutide, semaglutide (injectable and oral formulations), and lixisenatide, each with varying half-lives and dosing schedules. These medications work through several complementary mechanisms:
-
Glucose-dependent insulin secretion: They enhance insulin release from pancreatic beta cells only when blood glucose levels are elevated, reducing the risk of hypoglycaemia.
-
Suppression of glucagon: They inhibit the release of glucagon from pancreatic alpha cells, thereby reducing hepatic glucose output.
-
Delayed gastric emptying: By slowing the rate at which food leaves the stomach, GLP-1 agonists help moderate postprandial glucose excursions.
-
Central appetite regulation: They act on receptors in the hypothalamus to promote satiety and reduce food intake, contributing to weight loss.
According to NICE guidance (NG28), GLP-1 agonists are typically recommended as part of triple therapy for type 2 diabetes when metformin and other oral agents have not achieved adequate glycaemic control. They are particularly considered for patients with a body mass index (BMI) ≥35 kg/m² (with adjustment for ethnicity) or those for whom weight loss would benefit obesity-related comorbidities. Some GLP-1 agonists (liraglutide, semaglutide, dulaglutide) have also demonstrated cardiovascular outcome benefits in clinical trials. Treatment should be reviewed at six months and continued only if there has been a beneficial metabolic response.
Are GLP-1 Agonists Metabolised Through the Liver?
A common question among both patients and healthcare professionals is whether GLP-1 receptor agonists undergo hepatic metabolism. The short answer is no—GLP-1 agonists are not primarily metabolised through the liver via the cytochrome P450 enzyme system, which distinguishes them from many other medications. This characteristic has important clinical implications, particularly for patients with hepatic impairment or those taking multiple medications.
GLP-1 agonists are peptide-based molecules rather than small organic compounds. As such, they are not substrates for the hepatic cytochrome P450 (CYP) enzymes that metabolise the majority of oral medications. This means there is generally low potential for drug-drug interactions mediated through hepatic enzyme induction or inhibition, which can be advantageous in polypharmacy scenarios common in patients with type 2 diabetes.
However, GLP-1 agonists can affect the absorption of other oral medications through their effect on gastric emptying. For example, exenatide and lixisenatide may require timing separation from certain oral medications (such as antibiotics or oral contraceptives). Oral semaglutide may affect levothyroxine absorption, and thyroid function should be monitored when these medications are co-administered.
The absence of hepatic metabolism also means that dose adjustments are generally not required in patients with liver disease. According to UK Summaries of Product Characteristics (SmPCs), most GLP-1 agonists do not require dose modification for mild to moderate hepatic impairment. However, clinical experience in severe hepatic impairment remains limited, and caution is advised in this population. It is always advisable to check the specific SmPC for each agent.
It is worth noting that while the liver is not the primary site of GLP-1 agonist metabolism, it remains a target organ for their therapeutic effects. These medications reduce hepatic glucose production through glucagon suppression. Understanding that GLP-1 agonists bypass hepatic metabolism helps clinicians make informed prescribing decisions, particularly in complex patient populations with comorbid liver conditions.
How GLP-1 Agonists Are Broken Down in the Body
Understanding the metabolic fate of GLP-1 agonists requires appreciation of proteolytic degradation pathways rather than traditional hepatic metabolism. These peptide-based medications are broken down through mechanisms similar to endogenous proteins, primarily involving proteolytic enzymes throughout the body.
The principal route of degradation occurs through ubiquitous proteolytic enzymes present throughout the body, not confined to any single organ. These enzymes cleave the peptide bonds within the GLP-1 agonist molecule, breaking it down into smaller peptide fragments and individual amino acids. This process occurs systemically in various tissues and does not rely on hepatic enzyme systems.
The metabolites are then eliminated from the body, with the specific clearance pathways varying between agents. Exenatide is the notable exception among GLP-1 agonists, as it is predominantly cleared by the kidneys. According to its SmPC, exenatide should be used with caution in moderate renal impairment (eGFR 30-50 mL/min/1.73m²) and is not recommended in severe renal impairment or end-stage renal disease (eGFR <30 mL/min/1.73m²).
In contrast, liraglutide, dulaglutide, and semaglutide undergo more extensive proteolytic degradation with minimal reliance on renal excretion of intact drug. According to their respective SmPCs, these agents generally do not require dose adjustment in renal impairment, though caution is advised in severe renal impairment due to limited clinical experience.
Good clinical practice includes assessment of renal function before initiating GLP-1 therapy and periodic monitoring, particularly if patients develop dehydration from gastrointestinal side effects, as this could potentially affect renal function.
The half-life of GLP-1 agonists varies considerably, from hours (exenatide immediate-release) to days (semaglutide), influencing dosing frequency. Longer-acting formulations have been engineered through structural modifications that slow proteolytic degradation, such as albumin binding or pegylation, extending their therapeutic duration without altering the fundamental non-hepatic clearance pathway.
Monitoring and Safety Considerations for GLP-1 Therapy
Whilst GLP-1 agonists have a favourable safety profile compared to some other glucose-lowering agents, appropriate monitoring and patient education remain essential components of safe prescribing. Healthcare professionals should be aware of both common adverse effects and rare but serious complications.
Common adverse effects are predominantly gastrointestinal and include:
-
Nausea and vomiting: Occurring in up to 40% of patients, particularly during treatment initiation. These symptoms typically improve over several weeks. Advising patients to eat smaller, more frequent meals and to titrate doses gradually can help mitigate these effects.
-
Diarrhoea or constipation: Altered bowel habits are frequently reported and usually transient.
-
Injection site reactions: Mild erythema, itching, or discomfort at subcutaneous injection sites.
Important safety considerations include:
-
Pancreatitis: Patients should be counselled to seek immediate medical attention if they develop severe, persistent abdominal pain radiating to the back, which could indicate pancreatitis. GLP-1 agonists should be discontinued if pancreatitis is suspected.
-
Gallbladder disease: GLP-1 agonists have been associated with an increased risk of gallstones and cholecystitis. Patients should be advised to seek medical attention for symptoms such as right upper quadrant pain, fever, or jaundice.
-
Diabetic retinopathy: Particularly with semaglutide, rapid improvement in glucose control has been associated with temporary worsening of diabetic retinopathy. Appropriate ophthalmological monitoring should be considered, especially in patients with pre-existing retinopathy.
-
Risk of diabetic ketoacidosis (DKA): The MHRA has highlighted that rapid reduction or discontinuation of insulin when initiating GLP-1 therapy may increase the risk of DKA. Insulin doses should be reduced gradually with appropriate blood glucose monitoring.
-
Thyroid considerations: UK SmPCs include warnings about thyroid C-cell tumours based on rodent studies, though human relevance remains uncertain. Routine monitoring of thyroid function or calcitonin is not recommended in UK practice.
Patient safety advice should emphasise:
-
When to contact healthcare services: Persistent vomiting leading to dehydration, severe abdominal pain, or symptoms of hypoglycaemia (when used with insulin or sulphonylureas).
-
Hypoglycaemia risk: When GLP-1 agonists are used as monotherapy, hypoglycaemia risk is low due to their glucose-dependent mechanism. However, when combined with insulin or sulphonylureas, dose reduction of these agents may be necessary.
According to NICE guidance, GLP-1 therapy should be reviewed at six months, and continuation is only recommended if there has been a beneficial metabolic response (HbA1c reduction ≥11 mmol/mol or ≥1 percentage point) and weight loss of at least 3% of initial body weight. Regular follow-up ensures both efficacy and safety are maintained throughout treatment.
Patients should be encouraged to report any suspected adverse reactions to the MHRA Yellow Card scheme (yellowcard.mhra.gov.uk).
Frequently Asked Questions
Do GLP-1 agonists require dose adjustment in liver disease?
Most GLP-1 agonists do not require dose modification for mild to moderate hepatic impairment as they are not metabolised through the liver. However, caution is advised in severe hepatic impairment due to limited clinical experience, and the specific Summary of Product Characteristics should always be consulted.
Which GLP-1 agonist requires dose adjustment in renal impairment?
Exenatide is predominantly cleared by the kidneys and should be used with caution in moderate renal impairment (eGFR 30-50 mL/min/1.73m²) and is not recommended in severe renal impairment or end-stage renal disease (eGFR <30 mL/min/1.73m²). Other GLP-1 agonists such as liraglutide, dulaglutide, and semaglutide generally do not require renal dose adjustment.
What are the most common side effects of GLP-1 agonists?
The most common adverse effects are gastrointestinal, including nausea, vomiting, diarrhoea, and constipation, occurring in up to 40% of patients particularly during treatment initiation. These symptoms typically improve over several weeks with gradual dose titration and dietary modifications.
The health-related content published on this site is based on credible scientific sources and is periodically reviewed to ensure accuracy and relevance. Although we aim to reflect the most current medical knowledge, the material is meant for general education and awareness only.
The information on this site is not a substitute for professional medical advice. For any health concerns, please speak with a qualified medical professional. By using this information, you acknowledge responsibility for any decisions made and understand we are not liable for any consequences that may result.
Heading 1
Heading 2
Heading 3
Heading 4
Heading 5
Heading 6
Lorem ipsum dolor sit amet, consectetur adipiscing elit, sed do eiusmod tempor incididunt ut labore et dolore magna aliqua. Ut enim ad minim veniam, quis nostrud exercitation ullamco laboris nisi ut aliquip ex ea commodo consequat. Duis aute irure dolor in reprehenderit in voluptate velit esse cillum dolore eu fugiat nulla pariatur.
Block quote
Ordered list
- Item 1
- Item 2
- Item 3
Unordered list
- Item A
- Item B
- Item C
Bold text
Emphasis
Superscript
Subscript