GLP-1 receptor agonists for menopause weight loss represent an emerging treatment option for women experiencing weight changes during the menopausal transition. These medications, originally developed for type 2 diabetes, work by mimicking natural gut hormones to reduce appetite and promote weight reduction. Whilst not specifically licensed for menopausal weight gain, GLP-1 treatments may be prescribed for women meeting obesity treatment criteria during this life stage. Understanding eligibility, safety considerations, and NHS access pathways is essential for menopausal women considering this therapeutic approach alongside lifestyle modifications recommended by NICE and the NHS.
Summary: GLP-1 receptor agonists are not specifically licensed for menopausal weight gain but may be prescribed for women meeting obesity treatment criteria (BMI ≥35 kg/m² with comorbidities) during the menopausal transition.
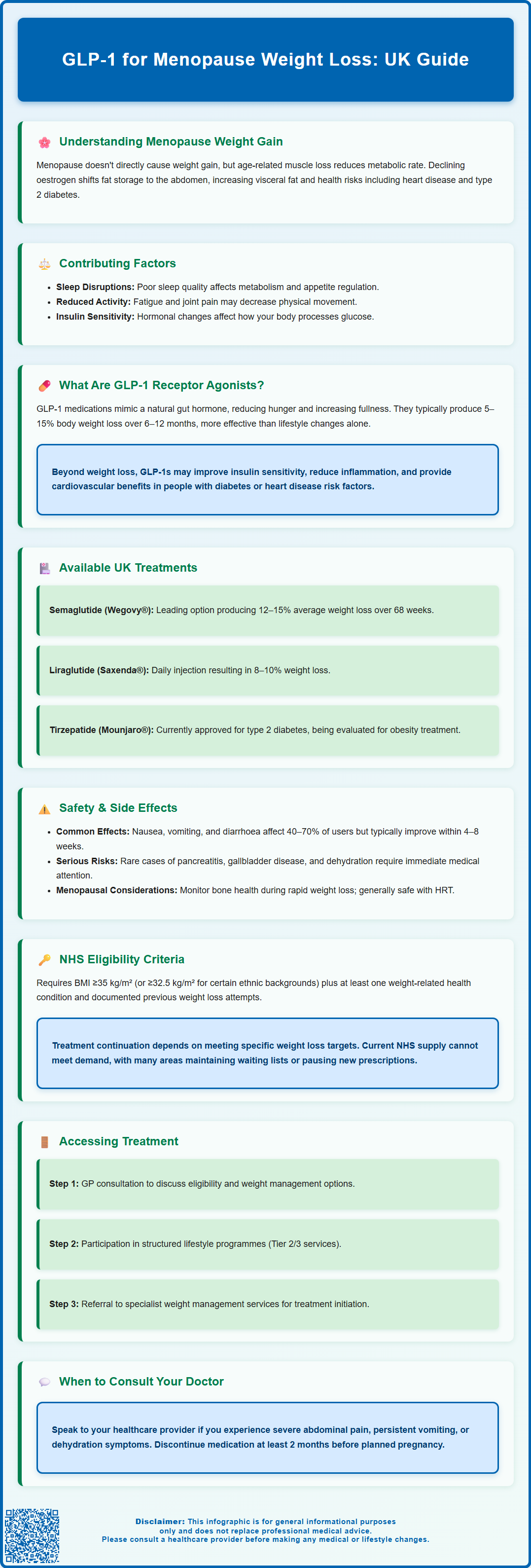
- GLP-1 receptor agonists mimic natural gut hormones to reduce appetite, slow gastric emptying, and promote gradual weight reduction over 6–12 months.
- Semaglutide (Wegovy®) and liraglutide (Saxenda®) are licensed for weight management in the UK, requiring specialist initiation within Tier 3 services.
- Common side effects include nausea, vomiting, and gastrointestinal discomfort, typically diminishing over 4–8 weeks with dose titration.
- NHS access requires BMI ≥35 kg/m² (or ≥32.5 kg/m² for specific ethnic groups) with weight-related comorbidities and previous lifestyle modification attempts.
- Treatment continuation depends on achieving specified weight loss targets; weight regain commonly occurs after discontinuation, suggesting long-term management may be necessary.
- Rare but serious risks include pancreatitis, gallbladder disease, and dehydration; suspected adverse reactions should be reported via the MHRA Yellow Card Scheme.
Table of Contents
Understanding Weight Gain During Menopause
Weight gain during the menopausal transition is common, affecting many women in the UK, typically occurring between ages 45 and 55. This phenomenon results from a complex interplay of ageing, lifestyle factors, and hormonal changes rather than a single cause.
Ageing and lifestyle factors are significant contributors to midlife weight changes. The natural decline in muscle mass (sarcopenia) that occurs with ageing leads to reduced metabolic rate, meaning fewer calories are burned at rest. This metabolic slowing means women may gain weight despite maintaining previous dietary habits.
Hormonal changes during menopause primarily affect fat distribution rather than directly causing weight gain. As oestrogen levels decline, the body undergoes significant metabolic shifts. Oestrogen plays a role in regulating body composition and fat distribution. The reduction in oestrogen typically causes a redistribution of adipose tissue from peripheral sites (hips and thighs) to central abdominal areas, increasing visceral fat accumulation. This shift in fat distribution carries particular health implications, as visceral adiposity is associated with increased cardiovascular risk, type 2 diabetes, and metabolic syndrome.
Additional contributing factors include:
-
Sleep disturbances and night sweats disrupting metabolic regulation
-
Reduced physical activity due to fatigue or joint discomfort
-
Psychological factors including stress, mood changes, and emotional eating
-
Changes in insulin sensitivity
Weight changes during the menopausal transition vary considerably between individuals. Understanding these mechanisms helps contextualise why traditional weight management approaches may prove challenging during this life stage. The NHS and NICE recommend lifestyle modifications including regular physical activity and dietary changes as first-line approaches to managing weight during menopause, with pharmacological interventions such as GLP-1 receptor agonists considered only in specific circumstances.
What Are GLP-1 Receptor Agonists?
GLP-1 (glucagon-like peptide-1) receptor agonists are a class of medications that mimic the action of naturally occurring GLP-1, an incretin hormone produced in the intestinal L-cells following food intake. These agents were initially developed for type 2 diabetes management but have demonstrated significant efficacy in weight reduction, leading to their expanded use in obesity treatment.
Mechanism of action: GLP-1 receptor agonists work through multiple physiological pathways. They bind to GLP-1 receptors located throughout the body, including the pancreas, brain, gastrointestinal tract, and cardiovascular system. In the pancreas, they enhance glucose-dependent insulin secretion whilst suppressing inappropriate glucagon release, thereby improving glycaemic control without causing hypoglycaemia. Crucially for weight management, these medications act on appetite-regulating centres in the hypothalamus, reducing hunger signals and increasing satiety. They also slow gastric emptying, prolonging the sensation of fullness after meals and reducing overall caloric intake.
The weight loss achieved with GLP-1 receptor agonists typically ranges from 5–15% of initial body weight, depending on the specific agent and dosage used. This reduction occurs gradually over 6–12 months and appears to be sustained with continued treatment. Clinical trials have demonstrated that weight loss with these medications exceeds that achieved through lifestyle modification alone. However, it's important to note that weight regain commonly occurs after discontinuation, suggesting that long-term management may be necessary for sustained benefits.
Beyond weight reduction, GLP-1 receptor agonists may offer additional metabolic benefits. In people with type 2 diabetes or specific cardiovascular risk factors, these can include improvements in insulin sensitivity, reduction in inflammatory markers, favourable effects on lipid profiles (particularly triglycerides), and potential cardiovascular benefits. Some evidence suggests potential effects on non-alcoholic fatty liver disease, though these benefits vary by specific medication and patient population.
It is important to note that whilst GLP-1 receptor agonists are not specifically licensed for "menopausal weight gain" as a distinct indication, they may be prescribed for women meeting criteria for obesity treatment or type 2 diabetes management during the menopausal transition.
Available GLP-1 Treatments in the UK
Several GLP-1 receptor agonists are currently licensed and available in the UK, each with distinct characteristics regarding administration, efficacy, and approved indications. The Medicines and Healthcare products Regulatory Agency (MHRA) regulates these medications, and NICE provides guidance on their use within the NHS.
Semaglutide represents the most widely discussed GLP-1 receptor agonist for weight management. It is available in two formulations: a once-weekly subcutaneous injection (Wegovy® for obesity, Ozempic® for type 2 diabetes) and a daily oral tablet (Rybelsus® for type 2 diabetes). Wegovy® received NICE approval in 2023 for weight management in adults with a BMI ≥35 kg/m² (or ≥32.5 kg/m² for people from South Asian, Chinese, other Asian, Middle Eastern, Black African, or African-Caribbean backgrounds) with at least one weight-related comorbidity. Treatment must be initiated and supervised within specialist weight management services (Tier 3) and is typically time-limited. Clinical trials have demonstrated average weight loss of 12–15% over 68 weeks with semaglutide 2.4 mg weekly.
Liraglutide (Saxenda® for obesity, Victoza® for diabetes) is administered as a once-daily subcutaneous injection. NICE TA664 recommends liraglutide 3.0 mg for weight management under similar specialist service criteria to semaglutide, though it typically produces slightly less weight reduction (approximately 8–10% of initial body weight).
Other GLP-1 receptor agonists licensed in the UK include dulaglutide (Trulicity®), exenatide (Byetta®, Bydureon®), and lixisenatide (Lyxumia®). These are primarily indicated for type 2 diabetes management rather than obesity treatment, though they may contribute to modest weight loss.
Tirzepatide (Mounjaro®), a dual GLP-1/GIP receptor agonist, received UK approval for type 2 diabetes and is under evaluation for obesity treatment. Early evidence suggests substantial weight loss potential in clinical trials.
Prescribing considerations: These medications require specialist initiation or shared care arrangements in many NHS settings. Treatment continuation depends on achieving specified weight loss targets as defined in the product-specific NICE guidance and SmPCs. It's important to note that Ozempic® is not licensed for weight management and should not be used off-label for this purpose given current UK supply constraints. Private prescription is also available, though costs are substantial, making this prohibitive for many patients.
Safety Considerations and Side Effects
Whilst GLP-1 receptor agonists demonstrate good overall tolerability, patients and prescribers must understand potential adverse effects and safety considerations, particularly for menopausal women who may have age-related comorbidities.
Gastrointestinal side effects represent the most common adverse reactions, affecting 40–70% of users to varying degrees. These include:
-
Nausea (often most pronounced during dose escalation)
-
Vomiting and diarrhoea
-
Constipation
-
Abdominal discomfort and bloating
-
Reduced appetite (therapeutic effect but may be excessive)
These symptoms typically diminish over 4–8 weeks as tolerance develops. Gradual dose titration, eating smaller meals, and avoiding high-fat foods can mitigate gastrointestinal effects. However, approximately 5–10% of patients discontinue treatment due to persistent gastrointestinal intolerance.
Serious but rare adverse effects require awareness:
-
Pancreatitis: Acute pancreatitis is a rare but serious potential risk. Patients should seek immediate medical attention for severe, persistent abdominal pain radiating to the back.
-
Gallbladder disease: Rapid weight loss increases cholelithiasis risk. Symptoms include right upper quadrant pain, particularly after fatty meals.
-
Hypoglycaemia: Risk is low with GLP-1 monotherapy but increases when combined with insulin or sulphonylureas.
-
Thyroid concerns: Animal studies identified thyroid C-cell tumours with some GLP-1 receptor agonists. While a causal relationship in humans has not been established, clinical vigilance is advised.
-
Diabetic retinopathy: In people with diabetes, rapid improvement in blood glucose can temporarily worsen retinopathy; appropriate monitoring is recommended.
-
Dehydration/acute kidney injury: Persistent vomiting or diarrhoea may lead to dehydration and kidney problems.
Specific considerations for menopausal women:
-
Interaction with hormone replacement therapy (HRT) appears minimal, though absorption of oral medications may be affected by delayed gastric emptying
-
Tirzepatide may reduce oral contraceptive effectiveness; additional contraceptive methods may be needed during initiation and dose escalation
-
Bone health monitoring may be advisable, as rapid weight loss can affect bone density
-
Cardiovascular benefits may be particularly relevant given increased cardiovascular risk post-menopause
When to contact your healthcare provider:
-
Severe or persistent abdominal pain
-
Persistent vomiting preventing fluid intake
-
Signs of dehydration
-
Symptoms of gallbladder disease
-
Any concerns about medication tolerability
Pregnancy must be avoided during treatment, and specific medications (e.g., semaglutide) require discontinuation at least 2 months before planned conception. Regular monitoring of weight, tolerability, and metabolic parameters is essential throughout treatment.
Suspected adverse reactions should be reported via the MHRA Yellow Card Scheme (yellowcard.mhra.gov.uk).
Accessing GLP-1 Treatment Through the NHS
Accessing GLP-1 receptor agonists for weight management through the NHS involves specific eligibility criteria and pathways, reflecting NICE guidance and local commissioning decisions. Understanding these requirements helps set realistic expectations for menopausal women considering this treatment option.
Eligibility criteria for NHS-funded GLP-1 treatment for weight management include:
-
For semaglutide (Wegovy®): BMI ≥35 kg/m² (or ≥32.5 kg/m² for people from South Asian, Chinese, other Asian, Middle Eastern, Black African, or African-Caribbean backgrounds) with at least one weight-related comorbidity
-
For liraglutide (Saxenda®): Similar BMI criteria as defined in NICE TA664
-
Evidence of previous weight management attempts through lifestyle modification
-
Treatment must be initiated within specialist weight management services (Tier 3)
-
Time-limited use as specified in the relevant NICE guidance
- The referral pathway typically involves:
- Initial GP consultation: Discuss weight concerns, document BMI and comorbidities, and review previous weight management efforts
- Tier 2/3 weight management services: Many areas require participation in structured lifestyle programmes before pharmacological intervention
- Specialist assessment: Referral to specialist weight management services for treatment initiation
- Ongoing monitoring: Regular review to assess response, tolerability, and continuation criteria
Treatment continuation requires achieving the weight loss thresholds specified in the product-specific NICE guidance and SmPCs. Failure to meet these thresholds typically results in treatment discontinuation, as cost-effectiveness is not demonstrated with lesser responses.
Current NHS challenges: Demand for GLP-1 receptor agonists substantially exceeds supply, with many NHS areas implementing waiting lists or restrictive prescribing policies. Some Integrated Care Boards have paused new initiations pending supply stabilisation. Patients should check with their healthcare provider about local availability.
Alternative access routes:
-
Private prescription: Available through private GPs, specialist weight management clinics, or online prescribing services, though costs are substantial
-
Clinical trials: Some research studies recruit menopausal women, offering supervised access to these medications
-
Diabetes indication: Women with type 2 diabetes may access GLP-1 receptor agonists through diabetes services according to NICE NG28 guidance
Patients should discuss their individual circumstances with their GP to determine eligibility and local access pathways. Realistic expectations regarding waiting times and the need for comprehensive lifestyle modification alongside pharmacotherapy are essential for successful outcomes.
Frequently Asked Questions
Can I get GLP-1 treatment on the NHS for menopause weight gain?
GLP-1 treatment is available on the NHS if you meet specific criteria: BMI ≥35 kg/m² (or ≥32.5 kg/m² for certain ethnic groups) with at least one weight-related comorbidity, previous lifestyle modification attempts, and referral to specialist weight management services (Tier 3). Treatment is not specifically licensed for menopausal weight gain but may be prescribed if you meet obesity treatment criteria during the menopausal transition.
How much weight can I expect to lose with GLP-1 medications during menopause?
Weight reduction with GLP-1 receptor agonists typically occurs gradually over 6–12 months and varies by specific medication. Semaglutide demonstrates substantial efficacy in clinical trials, whilst liraglutide produces moderate reductions. Individual responses vary considerably, and weight regain commonly occurs after discontinuation, suggesting long-term management may be necessary for sustained benefits.
Are GLP-1 medications safe to use alongside hormone replacement therapy (HRT)?
Interaction between GLP-1 receptor agonists and HRT appears minimal, though delayed gastric emptying caused by GLP-1 medications may affect absorption of oral medications. Women should discuss their complete medication regimen with their healthcare provider to ensure appropriate monitoring and management during treatment.
The health-related content published on this site is based on credible scientific sources and is periodically reviewed to ensure accuracy and relevance. Although we aim to reflect the most current medical knowledge, the material is meant for general education and awareness only.
The information on this site is not a substitute for professional medical advice. For any health concerns, please speak with a qualified medical professional. By using this information, you acknowledge responsibility for any decisions made and understand we are not liable for any consequences that may result.
Heading 1
Heading 2
Heading 3
Heading 4
Heading 5
Heading 6
Lorem ipsum dolor sit amet, consectetur adipiscing elit, sed do eiusmod tempor incididunt ut labore et dolore magna aliqua. Ut enim ad minim veniam, quis nostrud exercitation ullamco laboris nisi ut aliquip ex ea commodo consequat. Duis aute irure dolor in reprehenderit in voluptate velit esse cillum dolore eu fugiat nulla pariatur.
Block quote
Ordered list
- Item 1
- Item 2
- Item 3
Unordered list
- Item A
- Item B
- Item C
Bold text
Emphasis
Superscript
Subscript












