Wegovy®
A weekly GLP-1 treatment proven to reduce hunger and support meaningful, long-term fat loss.
- ~16.9% average body weight loss
- Boosts metabolic & cardiovascular health
- Proven, long-established safety profile
- Weekly injection, easy to use
Many people wonder whether Ozempic (semaglutide) speeds up metabolism as part of its effects on weight and blood sugar control. Ozempic is a glucagon-like peptide-1 (GLP-1) receptor agonist licensed in the UK for treating type 2 diabetes mellitus in adults. Whilst it can lead to weight loss and improved metabolic health markers, the mechanism is not through increasing metabolic rate. Instead, Ozempic works primarily by reducing appetite, slowing gastric emptying, and enhancing insulin secretion in a glucose-dependent manner. Understanding how this medication truly functions helps set realistic expectations for patients and healthcare professionals alike.
Summary: Ozempic does not directly speed up metabolism or increase basal metabolic rate; it facilitates weight loss primarily through appetite suppression and reduced caloric intake.
Ozempic (semaglutide) is a prescription medicine licensed in the UK for the treatment of type 2 diabetes mellitus in adults. It belongs to a class of drugs called glucagon-like peptide-1 (GLP-1) receptor agonists. Ozempic is administered as a once-weekly subcutaneous injection and is available in pre-filled pens at doses of 0.25 mg, 0.5 mg, 1 mg, and 2 mg.
The primary mechanism of action involves mimicking the naturally occurring hormone GLP-1, which is released by the intestine in response to food intake. By binding to GLP-1 receptors in the pancreas, Ozempic stimulates insulin secretion in a glucose-dependent manner—meaning it only works when blood glucose levels are elevated. This reduces the risk of hypoglycaemia compared to some other diabetes medications. Additionally, semaglutide suppresses glucagon release, a hormone that raises blood sugar, thereby helping to maintain more stable glucose levels throughout the day.
Beyond its effects on insulin and glucagon, Ozempic also acts on receptors in the brain, particularly in areas that regulate appetite and satiety. This leads to reduced hunger and increased feelings of fullness, which can result in decreased caloric intake. Furthermore, semaglutide slows gastric emptying—the rate at which food leaves the stomach—contributing to prolonged satiety after meals.
Ozempic is typically prescribed alongside lifestyle modifications, including diet and exercise, and may be used in combination with other glucose-lowering medications such as metformin. The Medicines and Healthcare products Regulatory Agency (MHRA) has approved Ozempic specifically for glycaemic control in type 2 diabetes, not for weight loss. It is not indicated for type 1 diabetes or for the treatment of diabetic ketoacidosis. NICE guidance supports its use in certain patient groups where other treatments have proven insufficient.
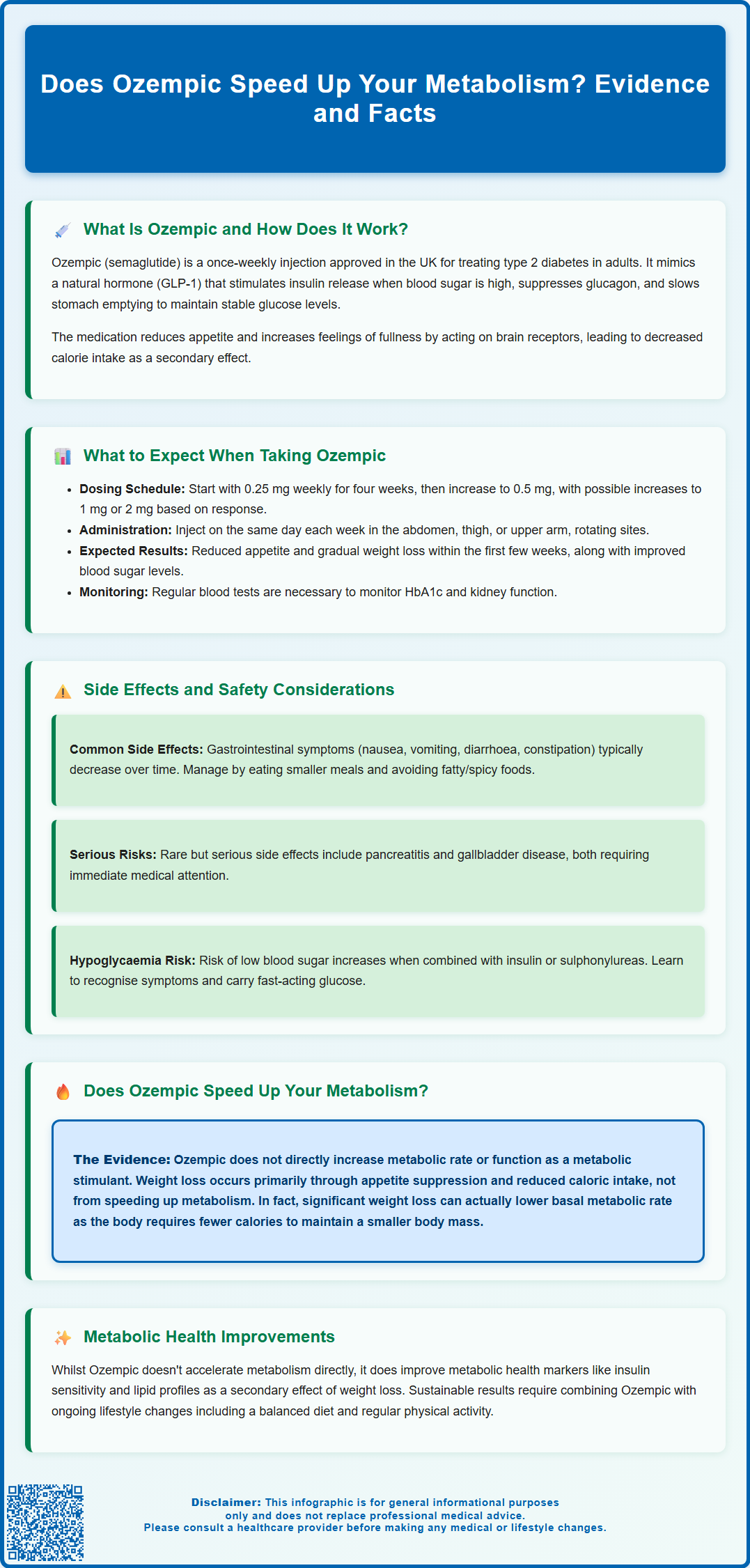
When initiating Ozempic therapy, patients typically begin with a starting dose of 0.25 mg once weekly for the first four weeks. This lower dose is not intended to provide full glycaemic control but rather to allow the body to adjust to the medication and minimise gastrointestinal side effects. After four weeks, the dose is usually increased to 0.5 mg weekly. Depending on individual response and tolerability, your healthcare provider may further increase the dose to 1 mg or 2 mg weekly after at least 4 weeks at each dose level to optimise blood glucose control.
Patients often notice a reduction in appetite within the first few weeks of treatment, which may lead to decreased food intake and gradual weight loss. Clinical trials have demonstrated that many individuals with type 2 diabetes experience significant improvements in HbA1c (a measure of average blood glucose over three months) alongside modest to substantial weight reduction. However, individual responses vary, and not everyone will experience the same degree of benefit.
It is important to administer Ozempic on the same day each week, though the time of day can be flexible. If needed, the weekly injection day can be changed provided at least 3 days (72 hours) have elapsed since the last dose. The injection can be given in the abdomen, thigh, or upper arm, and injection sites should be rotated to minimise injection-site reactions. If a dose is missed, it should be taken as soon as possible, provided the next scheduled dose is more than 5 days away; otherwise, skip the missed dose and take the next dose on the usual day.
Regular monitoring is essential while taking Ozempic. Your GP or diabetes specialist will typically arrange blood tests to assess HbA1c levels, kidney function, and other relevant parameters. When Ozempic is added to treatment with insulin or sulphonylureas, doses of these medications may need to be reduced to lower the risk of hypoglycaemia. Patients should stay well-hydrated, especially if experiencing vomiting or diarrhoea, as dehydration can lead to acute kidney injury. Seek medical advice promptly for persistent gastrointestinal symptoms. Ozempic is not recommended during pregnancy or breastfeeding, and women of childbearing potential should use effective contraception. If pregnancy is planned, Ozempic should be discontinued at least 2 months beforehand.
Like all medications, Ozempic can cause side effects, although not everyone will experience them. The most commonly reported adverse effects are gastrointestinal in nature and include nausea, vomiting, diarrhoea, constipation, and abdominal pain. These symptoms are usually mild to moderate and tend to diminish over time as the body adjusts to the medication. Starting at a lower dose and gradually titrating upwards helps to minimise these effects.
Nausea is particularly common during the initial weeks of treatment and after dose increases. Patients are advised to eat smaller, more frequent meals, avoid high-fat or spicy foods, and stay well hydrated. If nausea becomes severe or persistent, it is important to consult your GP, as dose adjustment or additional supportive measures may be required. Persistent vomiting or diarrhoea can lead to dehydration and acute kidney injury, so seek medical attention if you cannot maintain adequate fluid intake.
More serious, though rare, side effects include pancreatitis (inflammation of the pancreas). Symptoms such as severe, persistent abdominal pain that may radiate to the back, often accompanied by nausea and vomiting, warrant immediate medical attention. Ozempic should be discontinued if pancreatitis is suspected. There have also been reports of gallbladder disease, including cholelithiasis (gallstones) and cholecystitis, particularly in patients experiencing rapid weight loss.
Animal studies have shown an increased incidence of thyroid C-cell tumours with GLP-1 receptor agonists, although the relevance to humans is unknown. Patients should seek medical advice if they experience symptoms such as a lump in the neck, persistent hoarseness, or difficulty swallowing. Ozempic is not recommended in patients with severe gastrointestinal disease, including severe gastroparesis.
Hypoglycaemia risk is generally low with Ozempic monotherapy but increases when used in combination with insulin or sulphonylureas. Patients should be educated on recognising symptoms of low blood sugar—such as sweating, tremor, confusion, and palpitations—and the importance of carrying fast-acting glucose. Additionally, there have been reports of diabetic retinopathy complications, particularly in patients with pre-existing retinopathy who experience rapid improvements in glycaemic control. Regular eye examinations are recommended for all patients with diabetes, with enhanced monitoring for those with pre-existing retinopathy.
If you experience any side effects, talk to your doctor, pharmacist or nurse. This includes any possible side effects not listed in the package leaflet. You can also report side effects directly via the Yellow Card Scheme at yellowcard.mhra.gov.uk or via the Yellow Card app.
A common question among patients and the public is whether Ozempic directly speeds up metabolism. The short answer is that there is no official evidence that Ozempic increases metabolic rate in the way that some might expect. Metabolism refers to the complex biochemical processes by which the body converts food into energy, and basal metabolic rate (BMR) is the number of calories the body burns at rest to maintain vital functions.
Ozempic does not function as a traditional metabolic stimulant. It does not increase thermogenesis (heat production) or significantly elevate resting energy expenditure in humans. Instead, its primary effects on weight and energy balance are mediated through appetite suppression and reduced caloric intake. By acting on GLP-1 receptors in the brain, semaglutide decreases hunger and enhances satiety, leading individuals to consume fewer calories. This caloric deficit, rather than an increase in metabolic rate, is the main driver of weight loss observed in clinical trials.
That said, weight loss itself can have secondary effects on metabolism. As individuals lose weight, particularly adipose (fat) tissue, there may be improvements in insulin sensitivity and metabolic health markers, such as reduced inflammation and improved lipid profiles. However, it is also well established that significant weight loss can lead to a reduction in BMR, as the body requires fewer calories to maintain a lower body mass. This phenomenon, sometimes referred to as metabolic adaptation, means that the body becomes more efficient and burns fewer calories at rest.
In summary, while Ozempic facilitates weight loss and improves metabolic parameters associated with type 2 diabetes, it does not directly "speed up" metabolism. Its benefits are primarily achieved through reduced appetite, slower gastric emptying, and improved glycaemic control. Patients considering Ozempic should have realistic expectations and understand that sustainable weight management requires ongoing lifestyle modifications, including a balanced diet and regular physical activity, in conjunction with medication. Always consult your GP or diabetes specialist to discuss whether Ozempic is appropriate for your individual circumstances.
Ozempic causes weight loss primarily by reducing appetite and increasing feelings of fullness through its action on GLP-1 receptors in the brain, leading to decreased caloric intake rather than increased energy expenditure.
No, Ozempic is licensed by the MHRA specifically for glycaemic control in type 2 diabetes mellitus in adults, not for weight loss, although weight reduction is a common secondary effect.
The most common side effects are gastrointestinal, including nausea, vomiting, diarrhoea, constipation, and abdominal pain, which typically diminish over time as the body adjusts to the medication.
The health-related content published on this site is based on credible scientific sources and is periodically reviewed to ensure accuracy and relevance. Although we aim to reflect the most current medical knowledge, the material is meant for general education and awareness only.
The information on this site is not a substitute for professional medical advice. For any health concerns, please speak with a qualified medical professional. By using this information, you acknowledge responsibility for any decisions made and understand we are not liable for any consequences that may result.
Lorem ipsum dolor sit amet, consectetur adipiscing elit, sed do eiusmod tempor incididunt ut labore et dolore magna aliqua. Ut enim ad minim veniam, quis nostrud exercitation ullamco laboris nisi ut aliquip ex ea commodo consequat. Duis aute irure dolor in reprehenderit in voluptate velit esse cillum dolore eu fugiat nulla pariatur.
Block quote
Ordered list
Unordered list
Bold text
Emphasis
Superscript
Subscript