Ozempic (semaglutide) is a glucagon-like peptide-1 (GLP-1) receptor agonist licensed in the UK for type 2 diabetes mellitus and weight management. Many patients wonder whether Ozempic shows up in blood work or affects their laboratory results. Whilst Ozempic itself does not appear as a measurable substance in standard blood tests, it significantly influences metabolic parameters such as HbA1c, kidney function markers, and lipid profiles. Understanding what blood tests reveal during Ozempic treatment helps patients and clinicians monitor therapeutic effects, detect potential side effects, and ensure safe, effective diabetes management.
Summary: Ozempic (semaglutide) does not appear as a measurable substance in standard blood tests, but it significantly influences metabolic markers such as HbA1c, kidney function, and lipid profiles.
- Semaglutide is a GLP-1 receptor agonist licensed in the UK for type 2 diabetes mellitus and weight management
- Standard blood panels do not detect semaglutide levels as these are not routinely measured in UK clinical practice
- Ozempic typically reduces HbA1c by 1.0–1.5% and improves metabolic parameters including lipid profiles and liver enzymes
- Regular monitoring includes HbA1c every 3–6 months, annual renal and liver function tests, and assessment for gastrointestinal side effects
- Patients must inform all healthcare providers about Ozempic use, particularly before surgical procedures due to delayed gastric emptying
Table of Contents
Understanding Ozempic and Routine Blood Tests
Ozempic (semaglutide) is a glucagon-like peptide-1 (GLP-1) receptor agonist licensed in the UK for the treatment of type 2 diabetes mellitus and, at higher doses under the brand name Wegovy, for weight management in specific patient groups. Many patients prescribed this medication wonder whether it will be detected during routine blood tests or affect their laboratory results.
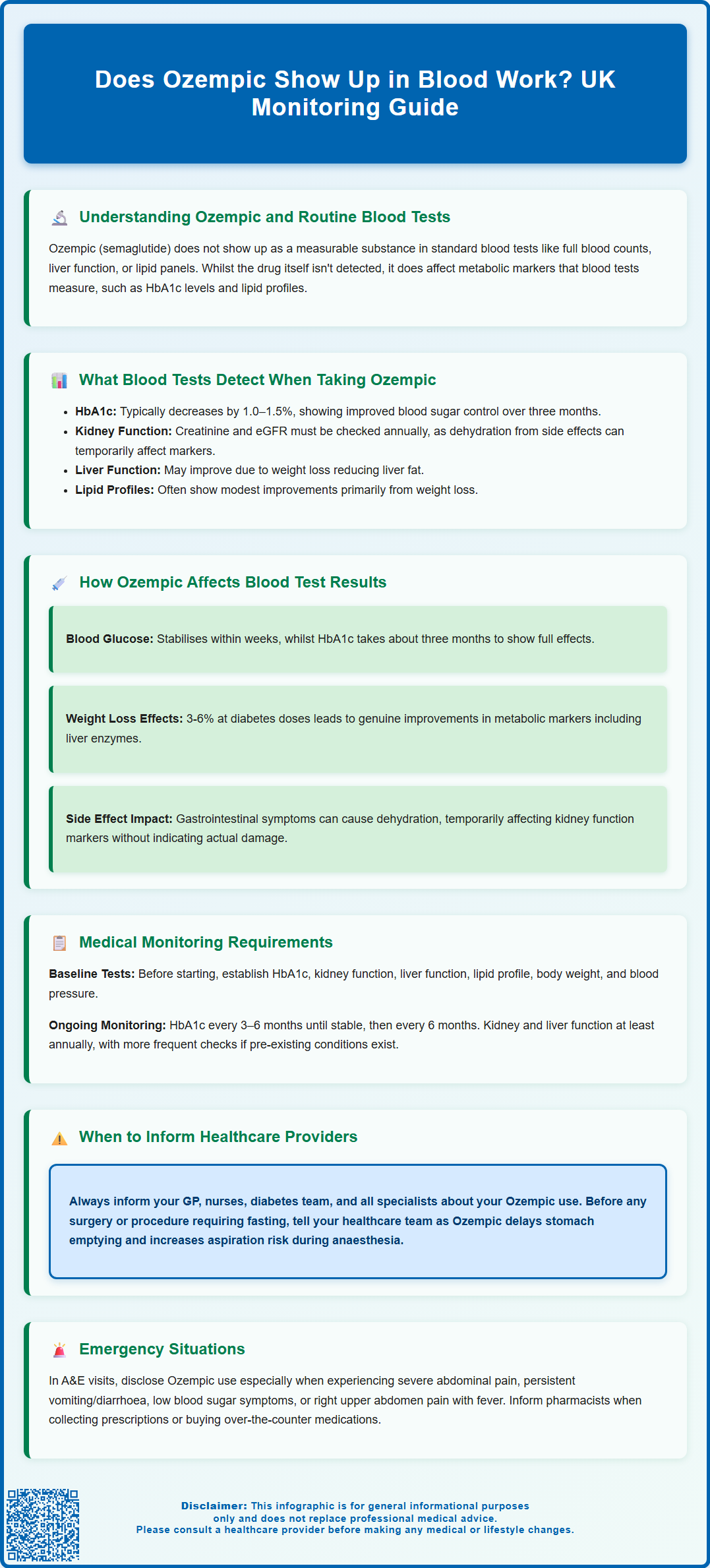
Ozempic itself does not typically appear as a measurable substance in standard blood work. Routine blood tests ordered by GPs or hospital clinicians—such as full blood counts, liver function tests, kidney function panels, or lipid profiles—are not designed to detect semaglutide or other GLP-1 receptor agonists. Semaglutide levels are not routinely measured in clinical practice in the UK. These medications work by mimicking the action of naturally occurring GLP-1 hormones, which regulate blood glucose levels and appetite, but the drug molecule itself is not measured.
However, whilst Ozempic won't show up as a distinct marker on standard blood panels, the medication does influence various metabolic parameters that blood tests measure . For instance, patients taking Ozempic for type 2 diabetes will typically see improvements in their HbA1c (glycated haemoglobin) levels, which reflect average blood glucose control over the preceding two to three months. Additionally, some patients may experience changes in lipid profiles, liver enzymes, or kidney function markers as their metabolic health improves or if side effects such as dehydration from gastrointestinal symptoms develop.
Understanding the distinction between direct detection of a medication and its effects on measurable health markers is important for patients undergoing regular monitoring. This knowledge helps set realistic expectations about what blood tests reveal and why ongoing monitoring remains essential during Ozempic treatment.
What Blood Tests Detect When Taking Ozempic
When patients take Ozempic, their blood tests primarily reveal the medication's therapeutic effects and any potential metabolic changes, rather than the presence of semaglutide itself. The most commonly monitored parameters include glycaemic control markers, kidney function, and liver enzymes.
HbA1c (glycated haemoglobin) is the cornerstone blood test for patients with type 2 diabetes taking Ozempic. This test measures the percentage of haemoglobin with glucose attached and provides an average picture of blood glucose levels over approximately three months. Patients typically see HbA1c reductions of 1.0–1.5% (11–16 mmol/mol) with Ozempic therapy, which represents clinically significant improvement in diabetes control. NICE guidelines (NG28) recommend monitoring HbA1c every three to six months until stable, then six-monthly in patients with type 2 diabetes.
Renal function tests, including serum creatinine and estimated glomerular filtration rate (eGFR), are routinely monitored at least annually, or more frequently in patients with pre-existing chronic kidney disease. Clinical trials in people with type 2 diabetes and CKD have shown potential kidney benefits with semaglutide, though this is not a licensed renal indication in the UK. Dehydration from gastrointestinal side effects such as nausea, vomiting, or diarrhoea can temporarily affect kidney function markers.
Liver function tests (LFTs) may show modest improvements in some patients as weight loss can reduce hepatic fat. However, it's important to note that gallbladder problems (cholelithiasis or cholecystitis) can occur with GLP-1 receptor agonists and may cause LFT abnormalities. Patients should seek medical attention for right upper quadrant pain and fever. Lipid profiles often show modest improvements with Ozempic treatment, primarily related to weight loss rather than direct drug effects. These changes reflect the medication's beneficial effects rather than direct detection of the drug itself.
How Ozempic Affects Blood Test Results
Ozempic influences blood test results through its pharmacological mechanism of action rather than through direct interference with laboratory assays. Understanding these effects helps patients and clinicians interpret blood work accurately during treatment.
The medication works by binding to GLP-1 receptors in pancreatic beta cells, enhancing glucose-dependent insulin secretion whilst suppressing inappropriate glucagon release. This mechanism leads to improved fasting and postprandial glucose levels, which become evident in both point-of-care glucose measurements and HbA1c testing. Patients may notice their blood glucose readings stabilise within weeks of starting treatment, though the full effect on HbA1c takes approximately three months to manifest fully.
Weight loss associated with Ozempic can produce secondary effects on various blood markers. At diabetes treatment doses (0.5-1mg weekly), patients typically lose around 3-6% of body weight. Higher doses used for weight management (Wegovy 2.4mg) can produce greater weight loss of up to 15%. As patients lose weight, metabolic parameters often improve. This may include improvements in liver enzymes (particularly in patients with fatty liver disease) and favourable changes in lipid profiles. These changes represent genuine health improvements rather than artificial alterations of test results.
In rare cases, gastrointestinal side effects from Ozempic—including nausea, vomiting, and diarrhoea—can lead to dehydration, which may temporarily affect kidney function markers and electrolyte levels. Elevated creatinine or reduced eGFR in the context of dehydration does not necessarily indicate kidney damage but rather volume depletion requiring clinical assessment and management.
Thyroid function tests remain unaffected by Ozempic in most patients. The UK SmPC notes that rodent studies showed C-cell tumours, but the human relevance is uncertain. Clinical monitoring is advised, but routine calcitonin testing is not required. Patients with concerns about personal or family history of medullary thyroid carcinoma or Multiple Endocrine Neoplasia syndrome type 2 should discuss this with their specialist.
Medical Monitoring Requirements for Ozempic Users
Patients prescribed Ozempic require structured monitoring protocols to ensure treatment safety and effectiveness, in accordance with NICE guidance and MHRA recommendations for GLP-1 receptor agonist therapy.
Baseline assessments before initiating Ozempic should include HbA1c, renal function (serum creatinine and eGFR), liver function tests, and lipid profile. Body weight and blood pressure should also be documented. These baseline values provide essential comparators for monitoring treatment response and detecting any adverse changes during therapy.
Ongoing monitoring schedules typically include:
-
HbA1c testing every 3–6 months until stable, then 6-monthly to assess glycaemic control and determine whether treatment targets are being achieved. NICE NG28 recommends individualised HbA1c targets: 48 mmol/mol (6.5%) for patients not on medications causing hypoglycaemia; 53 mmol/mol (7.0%) for those on agents with hypoglycaemia risk; with higher targets appropriate for some patients based on individual circumstances.
-
Renal function monitoring at least annually, or more frequently in patients with pre-existing kidney disease or those experiencing significant gastrointestinal side effects. Any acute deterioration in kidney function warrants prompt clinical review.
-
Liver function tests annually, or more frequently if baseline abnormalities exist or if patients develop symptoms suggesting hepatobiliary disease.
-
Weight and blood pressure measurements at each clinical review to document treatment response and cardiovascular benefits.
Additional monitoring considerations include assessing for symptoms of pancreatitis (severe, persistent abdominal pain), gallbladder disease (right upper quadrant pain, fever), or diabetic retinopathy changes. Patients should be educated about these potential adverse effects and advised to seek medical attention promptly if concerning symptoms develop. Those with pre-existing diabetic retinopathy should continue with the NHS Diabetic Eye Screening Programme and may require more frequent ophthalmological review, as rapid improvements in glycaemic control can occasionally worsen retinopathy temporarily.
Patients taking Ozempic alongside other glucose-lowering medications, particularly insulin or sulphonylureas, may require more frequent blood glucose monitoring to adjust doses and prevent hypoglycaemia as their diabetes control improves.
Any suspected adverse reactions should be reported via the MHRA Yellow Card scheme (yellowcard.mhra.gov.uk).
When to Inform Healthcare Providers About Ozempic Use
Transparent communication about Ozempic use is essential across all healthcare interactions to ensure safe, coordinated care and accurate interpretation of clinical findings and test results.
Patients should always inform their GP, practice nurse, and diabetes specialist team about their Ozempic prescription, including the dose and duration of treatment. This information should be clearly documented in medical records to ensure all healthcare professionals involved in the patient's care are aware. When attending appointments with other specialists—such as cardiologists, nephrologists, or surgeons—patients must disclose their Ozempic use, as it may influence treatment decisions and perioperative management.
Before any surgical procedures or investigations requiring fasting, patients must inform their healthcare team about Ozempic. The medication delays gastric emptying, which can increase the risk of aspiration during anaesthesia. Patients should follow local hospital perioperative guidance and their anaesthetist's advice regarding Ozempic management before procedures. Many patients can continue GLP-1 receptor agonists; decisions are based on individual aspiration risk assessment, with modifications to fasting and airway management plans as needed. If clinicians advise withholding Ozempic, ensure there's a plan for glycaemic management and resumption post-procedure.
When seeking emergency care or attending A&E, patients should inform healthcare providers about their Ozempic use, particularly if presenting with:
-
Severe abdominal pain (potential pancreatitis)
-
Persistent vomiting or diarrhoea (dehydration risk)
-
Symptoms of hypoglycaemia (if taking other diabetes medications)
-
Right upper quadrant pain or fever (potential gallbladder disease)
Pharmacists should be informed when collecting prescriptions or purchasing over-the-counter medications, as some drugs may interact with Ozempic or affect diabetes control. For instance, corticosteroids can raise blood glucose levels, potentially requiring dose adjustments.
When undergoing blood tests at private clinics or occupational health services, patients should mention their Ozempic use to provide context for interpreting results, particularly glucose and HbA1c levels. Whilst the medication itself won't be detected, its effects on metabolic markers are significant and should be considered when evaluating overall health status. This transparency ensures accurate clinical decision-making and optimal patient safety throughout the treatment journey.
Frequently Asked Questions
Can blood tests detect Ozempic in your system?
No, standard blood tests do not detect Ozempic (semaglutide) itself, as semaglutide levels are not routinely measured in UK clinical practice. However, blood tests will show the medication's effects on metabolic markers such as HbA1c, kidney function, and lipid profiles.
What blood tests are monitored whilst taking Ozempic?
Patients taking Ozempic require regular monitoring of HbA1c (every 3–6 months), renal function tests including creatinine and eGFR (at least annually), liver function tests (annually), and lipid profiles. These tests assess treatment effectiveness and detect potential side effects.
Should I tell my doctor I'm taking Ozempic before blood tests?
Yes, you should always inform healthcare providers about Ozempic use before blood tests and medical procedures. This ensures accurate interpretation of results, particularly glucose and HbA1c levels, and allows for appropriate clinical decision-making and perioperative management.
The health-related content published on this site is based on credible scientific sources and is periodically reviewed to ensure accuracy and relevance. Although we aim to reflect the most current medical knowledge, the material is meant for general education and awareness only.
The information on this site is not a substitute for professional medical advice. For any health concerns, please speak with a qualified medical professional. By using this information, you acknowledge responsibility for any decisions made and understand we are not liable for any consequences that may result.
Heading 1
Heading 2
Heading 3
Heading 4
Heading 5
Heading 6
Lorem ipsum dolor sit amet, consectetur adipiscing elit, sed do eiusmod tempor incididunt ut labore et dolore magna aliqua. Ut enim ad minim veniam, quis nostrud exercitation ullamco laboris nisi ut aliquip ex ea commodo consequat. Duis aute irure dolor in reprehenderit in voluptate velit esse cillum dolore eu fugiat nulla pariatur.
Block quote
Ordered list
- Item 1
- Item 2
- Item 3
Unordered list
- Item A
- Item B
- Item C
Bold text
Emphasis
Superscript
Subscript