Does Ozempic reduce hunger? Yes, Ozempic (semaglutide) does reduce hunger in many patients through its action as a GLP-1 receptor agonist. Licensed in the UK for type 2 diabetes mellitus, this once-weekly injectable medication works by mimicking natural gut hormones that regulate appetite. It slows gastric emptying and acts on brain centres controlling hunger, leading to reduced caloric intake and enhanced satiety. Whilst appetite suppression is a recognised effect, Ozempic is prescribed primarily for blood glucose control rather than weight management alone. Understanding how this medication influences hunger can help patients and clinicians optimise treatment outcomes safely.
Summary: Ozempic (semaglutide) does reduce hunger by activating GLP-1 receptors that slow gastric emptying and suppress appetite centres in the brain.
- Ozempic is a GLP-1 receptor agonist licensed in the UK for type 2 diabetes mellitus, not primarily for weight loss.
- It reduces hunger through delayed gastric emptying and central action on brain appetite centres including the hypothalamus.
- Clinical trials show significant appetite suppression with reduced caloric intake, though individual responses vary considerably.
- Common side effects include nausea, vomiting, and gastrointestinal discomfort, typically improving after initial weeks.
- Patients should maintain balanced nutrition despite reduced appetite and report severe abdominal pain or persistent vomiting urgently.
- NICE guidance supports GLP-1 use for glycaemic control in diabetes; higher-dose semaglutide (Wegovy) is licensed separately for weight management.
Table of Contents
How Ozempic Works to Control Appetite
Ozempic (semaglutide) is a glucagon-like peptide-1 (GLP-1) receptor agonist licensed in the UK for the treatment of type 2 diabetes mellitus. Its appetite-suppressing effects have garnered significant attention, though it is important to understand that weight loss is a secondary outcome rather than the primary indication for this medication.
The mechanism by which Ozempic influences hunger is multifaceted. GLP-1 is a naturally occurring incretin hormone released by the intestine in response to food intake. Semaglutide mimics this hormone by binding to GLP-1 receptors located throughout the body, including key areas of the brain involved in appetite regulation—particularly the hypothalamus and brainstem. By activating these receptors, Ozempic initially slows gastric emptying, meaning food remains in the stomach for longer periods. This delayed gastric emptying creates a sensation of fullness (satiety), though this specific effect may attenuate over time while central appetite effects persist.
Additionally, semaglutide acts centrally on appetite centres in the brain to reduce hunger signals and food cravings. This dual action—both peripheral (at the stomach level) and central (in the brain)—contributes to reduced caloric intake in many patients. Clinical studies have demonstrated that, on average, patients taking semaglutide consume fewer calories, which supports gradual, sustained weight loss over time.
It is worth noting that while Ozempic is prescribed primarily for glycaemic control in type 2 diabetes, the Medicines and Healthcare products Regulatory Agency (MHRA) has approved a higher-dose formulation of semaglutide (marketed as Wegovy) specifically for weight management. Wegovy is prescribed within specialist weight management services according to NICE criteria for adults with obesity or overweight with weight-related comorbidities. Both formulations share the same active ingredient and appetite-regulating mechanism.
What to Expect: Appetite Changes on Ozempic
Patients initiating Ozempic typically notice changes in appetite within the first few weeks of treatment, although individual responses vary considerably. The medication is administered once weekly via subcutaneous injection, and dosing follows a gradual titration schedule to minimise gastrointestinal side effects. Most patients begin with 0.25 mg weekly for four weeks as an initiation dose (not intended for glycaemic control), increasing to 0.5 mg, and potentially up to 1 mg or 2 mg depending on glycaemic targets and tolerability.
Early appetite suppression is commonly reported during the initial titration phase. Many patients describe feeling satisfied with smaller portion sizes, experiencing reduced cravings for high-calorie or sweet foods, and noticing less frequent hunger between meals. Some individuals report a subtle but persistent sense of fullness, even several hours after eating. These changes often become more pronounced as the dose increases, though the effect tends to plateau once a maintenance dose is established.
It is important to recognise that appetite reduction is not universal. Some patients may experience minimal changes in hunger, and response can be influenced by factors such as baseline eating patterns, metabolic health, concurrent medications, and psychological relationship with food. The appetite-suppressing effects generally persist during treatment, even as some gastric emptying effects may diminish.
Patients should be counselled that appetite changes do not equate to malnutrition. While reduced hunger is expected, it remains essential to consume balanced, nutrient-dense meals to meet daily nutritional requirements. Healthcare professionals should monitor weight trends, dietary intake, and any signs of inadequate nutrition, particularly in older adults or those with pre-existing nutritional vulnerabilities.
Patients taking Ozempic alongside insulin or sulfonylureas should be aware of an increased risk of hypoglycaemia and may require dose adjustments of these medications. Those with pre-existing diabetic retinopathy should report any visual changes promptly, as rapid improvements in blood glucose can occasionally worsen retinopathy.
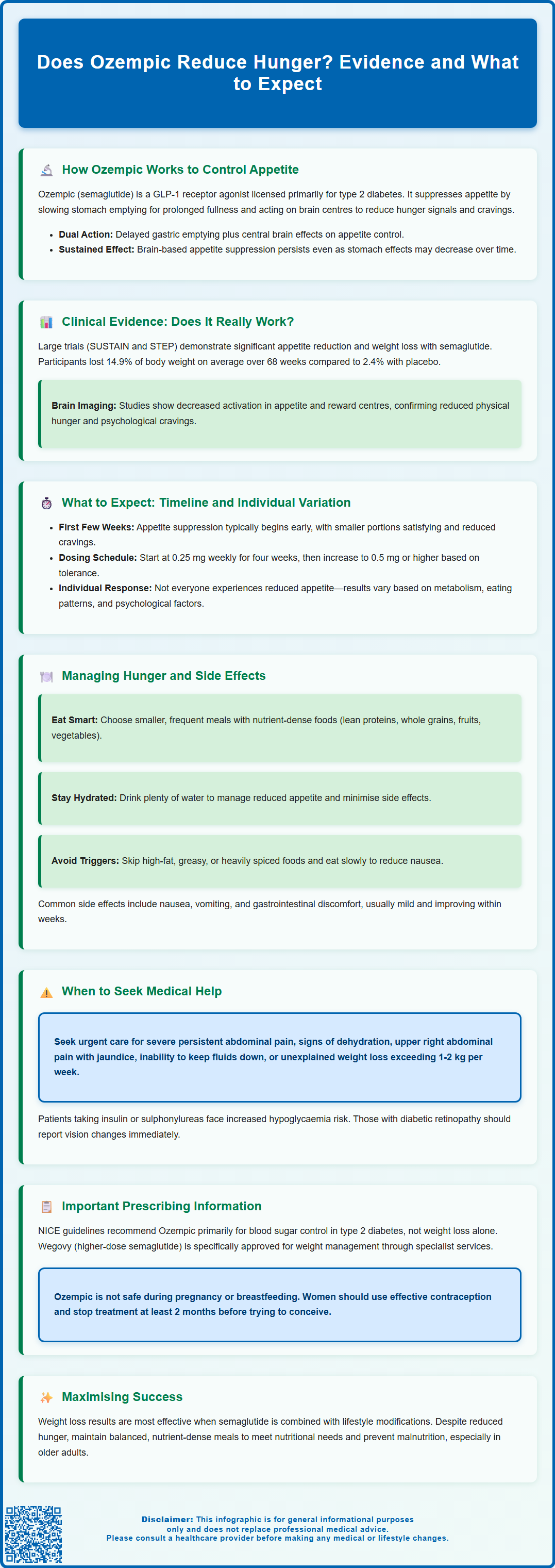
Managing Hunger and Side Effects While Taking Ozempic
While reduced appetite is a desired effect for many patients, it can occasionally lead to challenges, particularly when accompanied by gastrointestinal side effects. The most commonly reported adverse effects of Ozempic include nausea, vomiting, diarrhoea, constipation, and abdominal discomfort. These symptoms are usually mild to moderate and tend to improve after the first few weeks as the body adjusts to the medication.
To optimise tolerability and manage appetite changes effectively, patients are advised to adopt several practical strategies:
-
Eat smaller, more frequent meals rather than large portions, which can exacerbate nausea and feelings of excessive fullness.
-
Choose nutrient-dense foods such as lean proteins, whole grains, fruits, vegetables, and healthy fats to ensure adequate nutrition despite reduced caloric intake.
-
Stay well hydrated, as dehydration can worsen gastrointestinal symptoms, contribute to fatigue, and potentially affect kidney function.
-
Avoid high-fat, greasy, or heavily spiced foods, which may slow gastric emptying further and increase nausea.
-
Take time to eat slowly and chew thoroughly, allowing the body to register satiety signals appropriately.
If nausea becomes troublesome, patients should contact their GP or diabetes specialist nurse. Anti-emetic medications may be considered in some cases, though lifestyle modifications are typically the first-line approach. Persistent or severe gastrointestinal symptoms warrant medical review, as dose adjustment or temporary treatment interruption may be necessary.
When to seek urgent medical advice: Patients should call NHS 111 or contact their healthcare provider immediately if they experience severe, persistent abdominal pain (which may indicate pancreatitis), signs of dehydration (dizziness, reduced urine output, dry mouth), symptoms of gallbladder disease (severe pain in the upper right abdomen, jaundice), or an inability to tolerate oral fluids. Call 999 or attend A&E for severe symptoms such as persistent vomiting with abdominal pain or severe dehydration. Additionally, any unexplained weight loss exceeding 1–2 kg per week should be discussed with a clinician to rule out inadequate nutrition or other underlying concerns.
Ozempic is not recommended during pregnancy or breastfeeding. Women of childbearing potential should use effective contraception and discontinue treatment at least 2 months before a planned pregnancy.
Patients are encouraged to report any suspected side effects to the MHRA Yellow Card scheme.
Does Ozempic Reduce Hunger? Clinical Evidence
The clinical evidence supporting Ozempic's appetite-reducing effects is robust and derives from multiple large-scale randomised controlled trials. The SUSTAIN clinical trial programme, which evaluated semaglutide in patients with type 2 diabetes, consistently demonstrated significant reductions in body weight alongside improvements in glycaemic control. These weight reductions were attributed primarily to decreased caloric intake resulting from appetite suppression and enhanced satiety.
In the SUSTAIN 6 trial (published in the New England Journal of Medicine), patients receiving semaglutide 1 mg weekly experienced a mean weight loss of approximately 4.3 kg over 104 weeks compared to 0.7 kg with placebo. Subsequent studies, including the STEP trials examining higher-dose semaglutide for weight management, showed even more pronounced effects. In STEP 1, participants lost an average of 14.9% of their baseline body weight over 68 weeks with semaglutide 2.4 mg compared to 2.4% with placebo. Patient-reported outcomes from these trials confirmed reductions in hunger scores and food cravings in many participants.
Mechanistic studies using functional MRI have provided further insight, demonstrating that semaglutide reduces neural activation in brain regions associated with appetite and reward processing when participants are exposed to food cues. This suggests that the medication not only affects physical hunger but also diminishes the psychological drive to eat, though these mechanistic findings represent supportive rather than primary evidence.
NICE guidance (NG28 for type 2 diabetes) acknowledges the weight loss benefits of GLP-1 receptor agonists in the context of diabetes management, while separate technology appraisals address semaglutide for weight management. NICE emphasises that GLP-1 receptor agonists should be prescribed primarily for glycaemic control in diabetes rather than weight loss alone, unless using the licensed weight management formulation (Wegovy) within specialist services.
The evidence indicates that Ozempic does reduce hunger in many patients, and this effect translates into clinically meaningful weight loss when combined with appropriate lifestyle modifications. However, individual responses vary, and ongoing monitoring by healthcare professionals is essential to ensure safe and effective use.
Frequently Asked Questions
How quickly does Ozempic reduce hunger?
Most patients notice appetite changes within the first few weeks of starting Ozempic, with effects becoming more pronounced as the dose increases during the gradual titration schedule. Individual responses vary, and some patients may experience minimal changes in hunger.
Is Ozempic licensed for weight loss in the UK?
Ozempic is licensed for type 2 diabetes mellitus, not primarily for weight loss. A higher-dose formulation called Wegovy (also semaglutide) is separately licensed for weight management and prescribed within specialist services according to NICE criteria.
What should I do if I experience severe nausea on Ozempic?
Contact your GP or diabetes specialist nurse if nausea becomes troublesome. Eating smaller, frequent meals and avoiding high-fat foods can help, but persistent or severe symptoms may require dose adjustment or medical review.
The health-related content published on this site is based on credible scientific sources and is periodically reviewed to ensure accuracy and relevance. Although we aim to reflect the most current medical knowledge, the material is meant for general education and awareness only.
The information on this site is not a substitute for professional medical advice. For any health concerns, please speak with a qualified medical professional. By using this information, you acknowledge responsibility for any decisions made and understand we are not liable for any consequences that may result.
Heading 1
Heading 2
Heading 3
Heading 4
Heading 5
Heading 6
Lorem ipsum dolor sit amet, consectetur adipiscing elit, sed do eiusmod tempor incididunt ut labore et dolore magna aliqua. Ut enim ad minim veniam, quis nostrud exercitation ullamco laboris nisi ut aliquip ex ea commodo consequat. Duis aute irure dolor in reprehenderit in voluptate velit esse cillum dolore eu fugiat nulla pariatur.
Block quote
Ordered list
- Item 1
- Item 2
- Item 3
Unordered list
- Item A
- Item B
- Item C
Bold text
Emphasis
Superscript
Subscript












