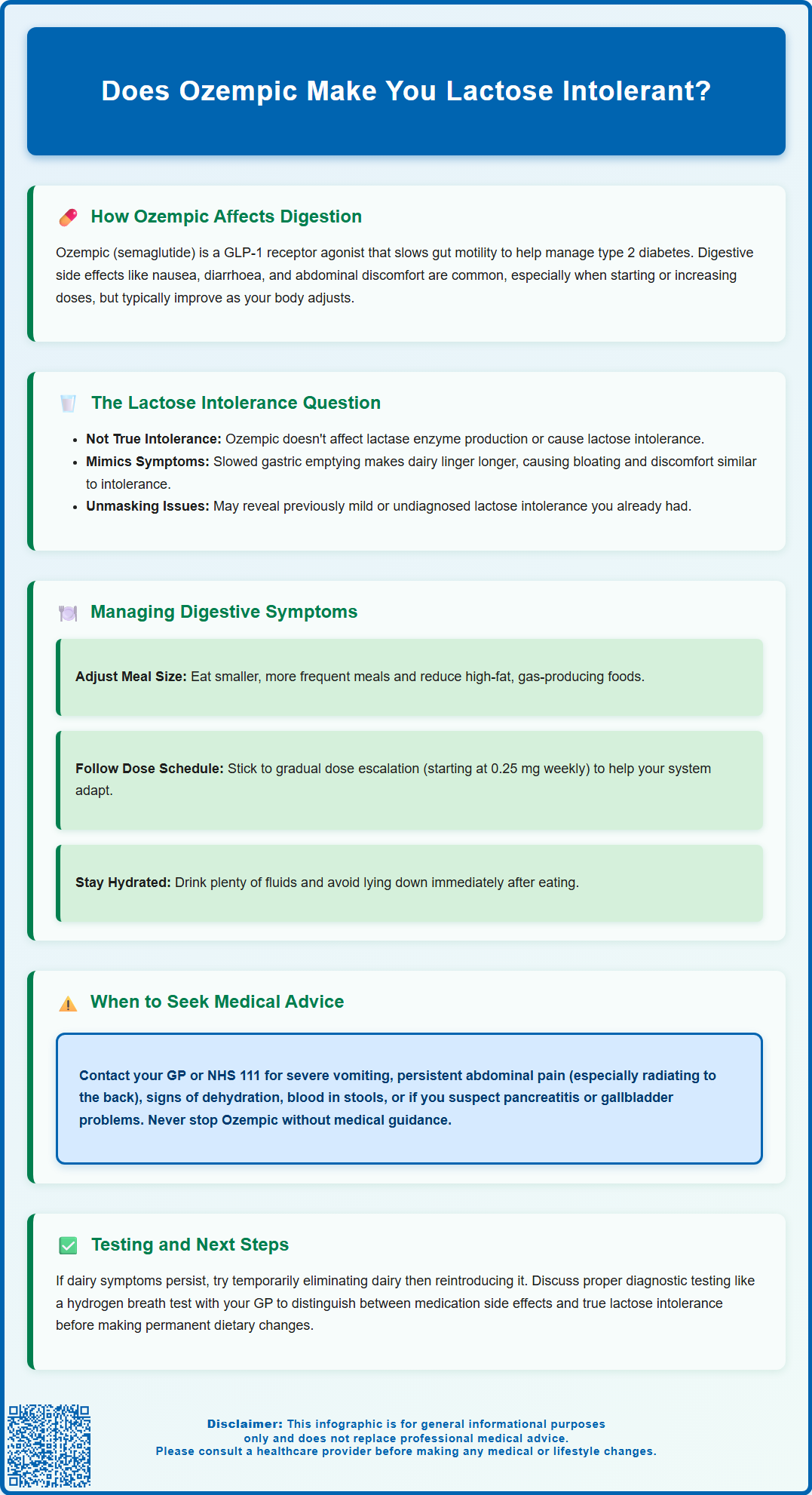
Does Ozempic make you lactose intolerant? This is a common concern among patients experiencing digestive symptoms whilst taking semaglutide. Ozempic (semaglutide) is a GLP-1 receptor agonist licensed in the UK for type 2 diabetes management. Whilst gastrointestinal side effects such as nausea, bloating, and diarrhoea are well-documented, there is no established link between Ozempic and the development of true lactose intolerance. However, the medication's effect on gastric emptying can produce symptoms that closely mimic lactose intolerance, leading to confusion. Understanding the distinction between medication-related digestive changes and genuine enzyme deficiency is essential for appropriate management and symptom relief.
Summary: Ozempic does not cause lactose intolerance, but its effect on gastric emptying can produce symptoms that mimic this condition.
- Ozempic (semaglutide) is a GLP-1 receptor agonist licensed in the UK for type 2 diabetes treatment, not for causing lactase enzyme deficiency.
- Gastrointestinal side effects including nausea, bloating, and diarrhoea are common, affecting more than 1 in 10 patients, particularly during dose initiation.
- Slowed gastric emptying caused by semaglutide can make dairy products remain in the digestive system longer, exacerbating bloating and discomfort.
- True lactose intolerance results from lactase enzyme deficiency and is not listed as an adverse reaction in the MHRA-approved product information.
- Management includes dietary modifications, gradual dose escalation, and monitoring for serious complications such as pancreatitis or gallbladder disease.
- Seek medical advice for severe abdominal pain, persistent vomiting, blood in stools, or symptoms suggesting pancreatitis or dehydration.
Table of Contents
Understanding Ozempic and Digestive Side Effects
Ozempic (semaglutide) is a glucagon-like peptide-1 (GLP-1) receptor agonist licensed in the UK for the treatment of type 2 diabetes mellitus. It works by mimicking the action of naturally occurring GLP-1, a hormone that stimulates insulin secretion in response to food intake, suppresses glucagon release, and affects gut motility. This mechanism helps improve glycaemic control and often leads to weight reduction as a secondary benefit, though weight management itself is not a licensed indication for Ozempic in the UK (a different semaglutide product, Wegovy, is specifically licensed for weight management).
Digestive side effects are among the most commonly reported adverse reactions associated with Ozempic therapy. According to the MHRA-approved Summary of Product Characteristics (SmPC), gastrointestinal disturbances affect a significant proportion of patients, particularly during dose initiation and escalation. The most frequently documented symptoms include:
-
Nausea (very common: may affect more than 1 in 10 people)
-
Diarrhoea (common: may affect up to 1 in 10 people)
-
Vomiting (common: may affect up to 1 in 10 people)
-
Abdominal pain and discomfort
-
Constipation
-
Dyspepsia (indigestion)
These effects are attributed to multiple factors including slowed gastric emptying, which delays the movement of food from the stomach into the small intestine, and central effects on appetite regulation. This physiological change can lead to feelings of fullness, bloating, and altered bowel habits. Most gastrointestinal symptoms are mild to moderate in severity and tend to diminish over time as the body adapts to the medication. However, the persistence or worsening of digestive complaints warrants clinical review to exclude other underlying conditions, including gallbladder disease, and to optimise management strategies.
Does Ozempic Cause Lactose Intolerance?
There is no established link between Ozempic (semaglutide) and the development of lactose intolerance. Lactose intolerance is not listed as an adverse reaction in the Ozempic SmPC and has not been demonstrated in clinical trials. Lactose intolerance is a specific condition caused by deficiency of lactase, the enzyme responsible for breaking down lactose (milk sugar) in the small intestine. This deficiency can be primary (genetic), secondary (resulting from intestinal damage), or developmental. Ozempic does not affect lactase production or the structural integrity of the intestinal brush border where this enzyme is located.
However, patients taking Ozempic may experience symptoms that mimic lactose intolerance, which can lead to confusion. The slowed gastric emptying caused by semaglutide means that dairy products, like other foods, remain in the digestive system for longer periods. This prolonged transit time can exacerbate feelings of bloating, abdominal discomfort, and nausea—symptoms that overlap considerably with those of lactose intolerance. Additionally, if a patient has pre-existing lactose intolerance that was previously mild or undiagnosed, the gastrointestinal effects of Ozempic may unmask or amplify these symptoms.
It is also worth noting that some individuals may develop temporary changes in digestive tolerance to certain foods whilst taking GLP-1 receptor agonists, not due to enzyme deficiency but rather due to altered gastric motility and heightened sensitivity to dietary components, though evidence for this is limited and largely observational. This phenomenon is distinct from true lactose intolerance. If you suspect lactose intolerance whilst on Ozempic, it may be helpful to try a short period of lactose restriction followed by reintroduction to assess your response. If symptoms persist, discuss with your healthcare provider about appropriate diagnostic approaches, which may include a hydrogen breath test to help diagnose lactose malabsorption.
Managing Digestive Symptoms While Taking Ozempic
Effective management of digestive symptoms whilst taking Ozempic involves a combination of dietary modifications, lifestyle adjustments, and appropriate medication use. The NICE guidance on type 2 diabetes management (NG28) emphasises the importance of patient education and individualised care when initiating GLP-1 receptor agonists.
Dietary strategies can significantly reduce gastrointestinal discomfort:
-
Eat smaller, more frequent meals rather than large portions, as this accommodates the slowed gastric emptying
-
Reduce intake of high-fat foods, which are digested more slowly and may worsen nausea and bloating
-
Limit foods that commonly cause gas, such as beans, cruciferous vegetables, and carbonated beverages
-
Stay well hydrated, particularly if experiencing diarrhoea
-
Consider temporarily reducing dairy intake if symptoms worsen after consuming milk products, then gradually reintroduce to assess tolerance
-
Avoid lying down immediately after eating to prevent reflux and discomfort
Regarding medication management, it is crucial to follow the prescribed dose escalation schedule. According to the SmPC, Ozempic is typically initiated at 0.25 mg once weekly for four weeks, then increased to 0.5 mg weekly. Further increases to 1 mg or 2 mg should only occur after at least four weeks at each dose level. This gradual titration allows the digestive system to adapt and minimises adverse effects.
Symptomatic relief may be achieved through:
-
Antiemetics for persistent nausea – speak to your GP or pharmacist for appropriate options as these require prescription or pharmacy advice
-
Antacids for dyspepsia
-
Loperamide for diarrhoea if appropriate, but avoid if you have blood in your stool, high fever, or severe abdominal pain
-
For constipation, increase fluid intake, gradually add fibre as tolerated, and consider a pharmacist-recommended osmotic laxative such as macrogol if needed
-
Probiotics, though evidence for their efficacy in this context remains limited
If you are also taking insulin or sulfonylureas, monitor your blood glucose closely and speak with your healthcare team about possible dose adjustments if your food intake decreases significantly, to reduce the risk of hypoglycaemia.
Patients should maintain regular contact with their diabetes care team, particularly during the first few months of treatment, to ensure symptoms are monitored and managed appropriately. Note that Ozempic is not recommended for patients with severe gastrointestinal disease, including severe gastroparesis.
When to Seek Medical Advice About Digestive Changes
While mild gastrointestinal symptoms are expected with Ozempic, certain warning signs require prompt medical assessment. Patients should contact their GP or diabetes specialist nurse if they experience:
-
Severe or persistent vomiting that prevents adequate fluid or food intake, as this increases the risk of dehydration and hypoglycaemia
-
Severe abdominal pain, particularly if constant or radiating to the back, which could indicate pancreatitis—a rare but serious adverse effect of GLP-1 receptor agonists
-
Sudden pain in the right upper abdomen, fever or jaundice, which may indicate gallbladder problems (cholelithiasis or cholecystitis)
-
Blood in stools or black, tarry stools
-
Unexplained weight loss beyond what is expected from the medication's therapeutic effect
-
Signs of dehydration, including reduced urine output, dizziness, or confusion
-
Persistent diarrhoea lasting more than a few days
-
Symptoms that significantly impair quality of life or prevent adherence to the medication regimen
Pancreatitis is a particular concern with semaglutide, though it remains uncommon. Characteristic symptoms include severe, persistent abdominal pain (often radiating to the back), nausea, and vomiting. If pancreatitis is suspected, Ozempic should be discontinued immediately and not restarted if pancreatitis is confirmed, as stated in the SmPC.
If you believe you may have developed genuine lactose intolerance rather than medication-related symptoms, discuss this with your GP. A trial of lactose reduction followed by reintroduction can be a practical first step. If needed, a hydrogen breath test can help diagnose lactose malabsorption.
If digestive symptoms do not improve with standard management strategies or worsen over time, further investigation may be warranted to exclude other gastrointestinal conditions such as gastroparesis, inflammatory bowel disease, or coeliac disease.
For urgent symptoms such as severe abdominal pain with vomiting, inability to keep fluids down, or passing little or no urine, contact NHS 111 for advice or attend A&E if symptoms are severe. You can report any suspected side effects to the MHRA through the Yellow Card Scheme.
Your healthcare team can help determine whether symptoms are an expected side effect of Ozempic requiring supportive management, or whether they indicate a more serious condition requiring investigation or treatment modification. Never discontinue Ozempic without medical guidance, as abrupt cessation may affect your diabetes control.
Frequently Asked Questions
Can Ozempic cause permanent lactose intolerance?
No, Ozempic does not cause permanent lactose intolerance. The medication does not affect lactase enzyme production or damage the intestinal lining where lactose is digested. Digestive symptoms related to dairy typically resolve when the body adapts to the medication or if Ozempic is discontinued.
Why do I feel worse after eating dairy whilst taking Ozempic?
Ozempic slows gastric emptying, causing dairy products to remain in your digestive system longer. This prolonged transit time can lead to bloating, nausea, and discomfort that mimics lactose intolerance, even if you do not have true enzyme deficiency.
Should I avoid dairy completely whilst taking Ozempic?
Complete avoidance is not necessary unless you have confirmed lactose intolerance. Consider temporarily reducing dairy intake if symptoms worsen, then gradually reintroduce to assess tolerance. Smaller portions and low-fat dairy options may be better tolerated due to slower digestion of high-fat foods.
The health-related content published on this site is based on credible scientific sources and is periodically reviewed to ensure accuracy and relevance. Although we aim to reflect the most current medical knowledge, the material is meant for general education and awareness only.
The information on this site is not a substitute for professional medical advice. For any health concerns, please speak with a qualified medical professional. By using this information, you acknowledge responsibility for any decisions made and understand we are not liable for any consequences that may result.
Heading 1
Heading 2
Heading 3
Heading 4
Heading 5
Heading 6
Lorem ipsum dolor sit amet, consectetur adipiscing elit, sed do eiusmod tempor incididunt ut labore et dolore magna aliqua. Ut enim ad minim veniam, quis nostrud exercitation ullamco laboris nisi ut aliquip ex ea commodo consequat. Duis aute irure dolor in reprehenderit in voluptate velit esse cillum dolore eu fugiat nulla pariatur.
Block quote
Ordered list
- Item 1
- Item 2
- Item 3
Unordered list
- Item A
- Item B
- Item C
Bold text
Emphasis
Superscript
Subscript