Ozempic (semaglutide) does not lower blood sugar immediately after injection. Unlike rapid-acting insulin, which works within minutes, Ozempic is a once-weekly GLP-1 receptor agonist that requires time to reach therapeutic levels in the body. Initial glucose-lowering effects typically begin within the first week, but significant improvements in blood sugar control generally take 8–12 weeks to develop. Understanding this timeline helps patients set realistic expectations and supports adherence to treatment. This article explains how Ozempic works, when to expect results, and how to manage blood glucose safely during the initiation period.
Summary: Ozempic does not lower blood sugar immediately; initial effects typically begin within the first week, with significant improvements in HbA1c generally observed after 8–12 weeks of treatment.
- Ozempic (semaglutide) is a GLP-1 receptor agonist that stimulates glucose-dependent insulin secretion and suppresses glucagon release.
- Steady-state plasma concentrations are achieved after approximately 4–5 weeks of once-weekly dosing.
- Treatment begins with a 0.25 mg starter dose for four weeks to improve gastrointestinal tolerability before escalating to maintenance doses.
- Common side effects include nausea, vomiting, and diarrhoea, which are typically mild to moderate and improve after 4–8 weeks.
- Dose adjustments of sulfonylureas or insulin may be required to prevent hypoglycaemia as Ozempic becomes effective.
- Ozempic is licensed in the UK for type 2 diabetes only and should be used alongside diet and exercise modifications.
Table of Contents
How Ozempic Works to Lower Blood Sugar
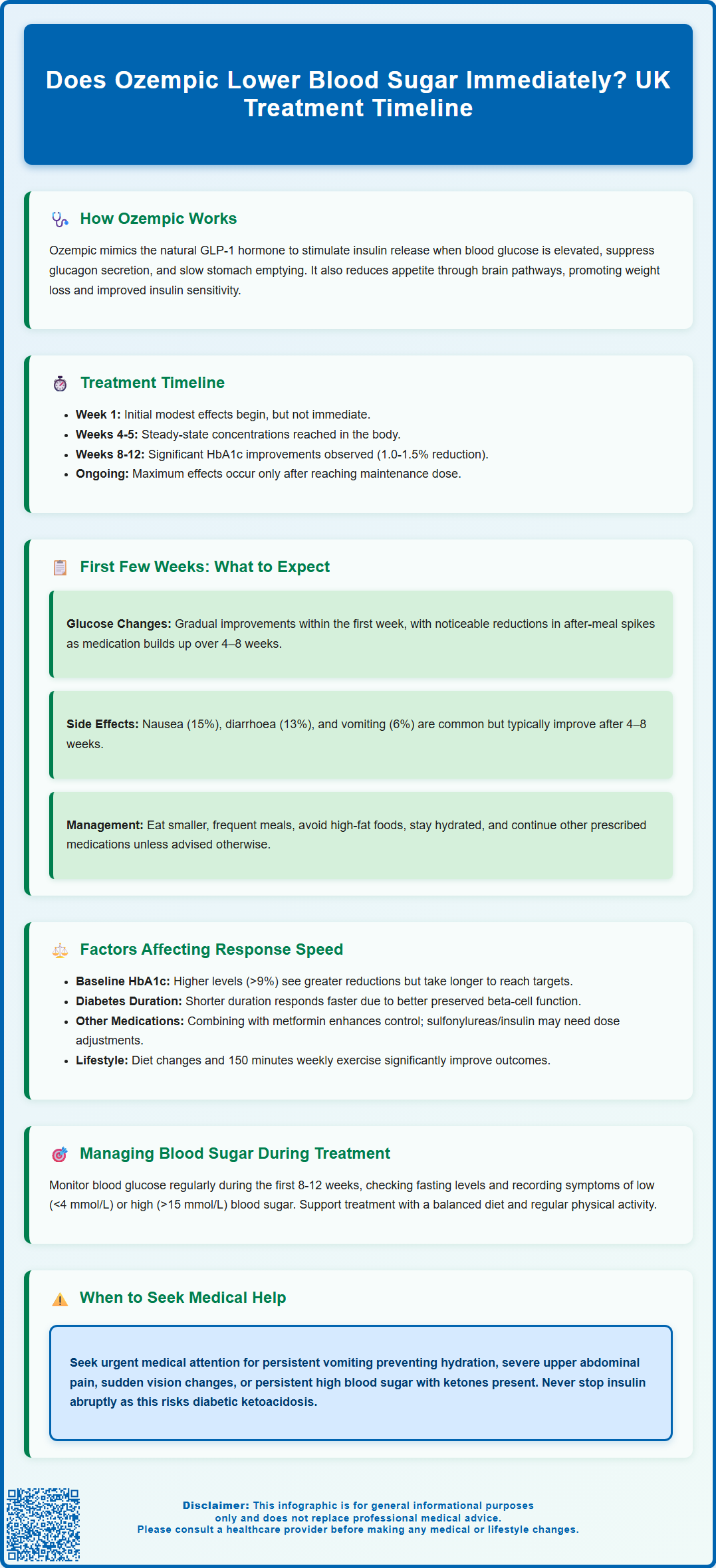
Ozempic (semaglutide) is a glucagon-like peptide-1 receptor agonist (GLP-1 RA) licensed in the UK for the treatment of type 2 diabetes mellitus. It works through several complementary mechanisms to improve glycaemic control, though it does not produce an immediate reduction in blood glucose levels in the way that rapid-acting insulin does.
The primary mechanism involves mimicking the action of endogenous GLP-1, a naturally occurring incretin hormone released from the gut in response to food intake. Semaglutide binds to GLP-1 receptors on pancreatic beta cells, stimulating glucose-dependent insulin secretion. Crucially, this effect is glucose-dependent, meaning insulin release only occurs when blood glucose levels are elevated, which significantly reduces the risk of hypoglycaemia compared to sulfonylureas or insulin therapy, though this risk remains if Ozempic is combined with these medications.
Additionally, Ozempic suppresses glucagon secretion from pancreatic alpha cells when glucose levels are elevated. Glucagon normally stimulates hepatic glucose production, so its suppression helps reduce excessive glucose output from the liver. The medication also slows gastric emptying, which moderates the rate at which glucose enters the bloodstream after meals, contributing to improved postprandial glucose control. This effect may be most prominent early in treatment and can diminish over time with long-acting GLP-1 RAs.
Beyond these direct glycaemic effects, semaglutide promotes satiety and reduces appetite through central nervous system pathways, often leading to weight loss. This secondary benefit can improve insulin sensitivity over time, further enhancing blood glucose control. The MHRA-approved indication specifies use alongside diet and exercise for type 2 diabetes only (not type 1 diabetes or diabetic ketoacidosis), and the medication is administered once weekly via subcutaneous injection, providing sustained therapeutic levels throughout the dosing interval. Ozempic is available in 0.25 mg, 0.5 mg, 1 mg, and 2 mg maintenance doses.
Timeline: When Does Ozempic Start Reducing Blood Glucose Levels?
Ozempic does not lower blood sugar immediately upon administration. Unlike rapid-acting insulin analogues that begin working within 15 minutes, semaglutide requires time to reach therapeutic concentrations and exert its full pharmacological effects.
Following the first injection, initial effects on blood glucose typically begin within the first week, though modest initially. According to the European Medicines Agency's assessment report, semaglutide reaches maximum plasma concentration (tmax) within 1-3 days after dosing. Clinical pharmacology studies demonstrate that steady-state plasma concentrations of semaglutide are achieved after approximately 4–5 weeks of once-weekly dosing. This means the medication gradually accumulates in the body, with progressively greater glucose-lowering effects over the first month of treatment.
Significant improvements in HbA1c (glycated haemoglobin, reflecting average blood glucose over 2–3 months) are generally observed after 8–12 weeks of treatment. The SUSTAIN clinical trial programme, which informed NICE guidance (NG28), demonstrated mean HbA1c reductions of 1.0–1.5% (11–16 mmol/mol) at 30 weeks, depending on the dose used.
The dose escalation schedule also influences the timeline. Treatment typically commences with 0.25 mg weekly for four weeks (a non-therapeutic starter dose designed to improve gastrointestinal tolerability), followed by an increase to 0.5 mg weekly. If additional glycaemic control is required after at least four weeks, the dose may be increased to 1 mg weekly. For patients who require further glycaemic control after at least 4 weeks on the 1 mg dose, the dose can be increased to the maximum 2 mg weekly. Maximum glucose-lowering effects correspond with reaching the maintenance dose and achieving steady-state concentrations.
Patients should be counselled that Ozempic is not a rescue medication for acute hyperglycaemia and that patience is required to observe its full therapeutic benefit.
What to Expect in the First Few Weeks of Treatment
During the initial 4–8 weeks of Ozempic therapy, patients typically experience gradual improvements in blood glucose control alongside potential gastrointestinal side effects. Understanding what to expect during this period helps set realistic expectations and supports treatment adherence.
Blood glucose changes in the first few weeks are usually modest. Fasting glucose levels may begin to decline within the first week, but postprandial (after-meal) glucose improvements become more apparent as the medication reaches higher concentrations. Patients using continuous glucose monitoring or regular capillary blood glucose testing may notice less pronounced glucose spikes after meals and a gradual lowering of overall glucose trends. However, dramatic reductions should not be expected immediately.
Gastrointestinal adverse effects are the most commonly reported side effects during initiation. According to the SmPC, nausea occurs in approximately 15% of patients, with vomiting (6%), diarrhoea (13%), constipation, and abdominal discomfort also reported. These effects are typically mild to moderate and transient, often improving after 4–8 weeks as the body adapts. The low starter dose (0.25 mg) is specifically designed to minimise these effects. Patients should be advised to eat smaller, more frequent meals, avoid high-fat foods, and stay well-hydrated. If persistent vomiting or diarrhoea occurs, patients should seek medical advice due to the risk of dehydration and acute kidney injury.
Weight loss may begin during the first month, though this varies considerably between individuals. Weight reduction is gradual and continues over months of treatment, with individual responses varying significantly.
Patients should be advised to continue their existing diabetes medications as prescribed unless specifically instructed otherwise by their healthcare provider. Regular blood glucose monitoring remains important, particularly if taking medications that carry hypoglycaemia risk (such as sulfonylureas or insulin), as dose adjustments may be required as Ozempic begins to work.
Patients should also be aware of the rare but serious risk of gallbladder disease (seek medical attention for severe upper abdominal pain) and that rapid improvement in glucose control has been associated with temporary worsening of diabetic retinopathy in some patients.
Factors That Influence How Quickly Ozempic Works
Several patient-specific and clinical factors influence the rate and extent of glucose-lowering response to Ozempic, contributing to the considerable inter-individual variation observed in clinical practice.
Baseline HbA1c and diabetes duration significantly affect response. Patients with higher baseline HbA1c levels (e.g., >75 mmol/mol or 9%) typically experience greater absolute reductions, though their glucose levels may take longer to reach target ranges. Conversely, those with shorter diabetes duration and better preserved beta-cell function often respond more rapidly, as their pancreatic cells retain greater capacity to respond to GLP-1 receptor stimulation.
Body weight and insulin resistance also play important roles. Patients with higher body mass index (BMI) may experience more pronounced weight loss, which subsequently improves insulin sensitivity and enhances glucose control over time. However, greater insulin resistance may initially blunt the glucose-lowering response until weight loss and lifestyle modifications take effect.
Concomitant medications can influence outcomes. Patients taking metformin alongside Ozempic often achieve better glycaemic control than those on Ozempic monotherapy. Conversely, medications that impair glucose metabolism (such as corticosteroids) may attenuate the response. Dose adjustments of sulfonylureas or insulin are frequently required to prevent hypoglycaemia as Ozempic becomes effective.
Adherence to lifestyle modifications substantially impacts treatment success. NICE guidance (NG28) emphasises that GLP-1 receptor agonists should be prescribed alongside dietary modification and increased physical activity. Patients who engage with structured education programmes and make sustained lifestyle changes typically achieve better and faster glucose improvements.
Gastrointestinal tolerability affects adherence and therefore effectiveness. Patients who experience severe nausea may struggle with the dose escalation schedule, potentially delaying achievement of therapeutic doses.
According to the SmPC, no dose adjustment is required for patients with renal or hepatic impairment, though clinical experience in severe impairment is limited and tolerability should be monitored.
Managing Blood Sugar While Starting Ozempic
Effective blood glucose management during Ozempic initiation requires a structured approach combining monitoring, medication adjustment, lifestyle optimisation, and patient education to ensure safety and maximise therapeutic benefit.
Regular glucose monitoring is essential, particularly in the first 8–12 weeks. Patients should be advised to:
-
Check fasting glucose regularly, especially if taking insulin or sulfonylureas
-
Monitor pre- and post-meal glucose periodically to assess postprandial control
-
Record symptoms of hypoglycaemia (blood glucose <4 mmol/L) or persistent hyperglycaemia (>15 mmol/L)
-
Report concerning patterns to their diabetes care team promptly
Medication adjustments are frequently necessary. NICE guidance (NG28) recommends:
-
Consider reducing sulfonylurea or insulin doses when starting Ozempic to mitigate hypoglycaemia risk, with adjustments guided by blood glucose monitoring
-
Maintaining metformin at existing doses unless contraindicated
-
Reviewing all medications that affect glucose metabolism
-
Never stopping insulin abruptly, as this could lead to diabetic ketoacidosis (DKA)
Lifestyle optimisation enhances Ozempic's effectiveness. Patients should be encouraged to:
-
Follow a balanced, portion-controlled diet emphasising whole grains, vegetables, lean proteins, and healthy fats
-
Engage in regular physical activity (at least 150 minutes of moderate-intensity exercise weekly, as per NICE guidance)
-
Stay well-hydrated to minimise gastrointestinal side effects
-
Avoid excessive alcohol consumption, which can impair glucose regulation
Patient safety advice includes recognising when to seek medical attention:
-
Contact your GP or diabetes nurse if experiencing persistent nausea/vomiting preventing adequate nutrition or hydration
-
Contact NHS 111 or seek urgent medical advice for severe abdominal pain (potential pancreatitis or gallbladder disease, though rare)
-
Report visual changes or symptoms of diabetic retinopathy progression
-
Seek emergency care (A&E) for persistent vomiting with reduced urine output, or for persistent hyperglycaemia with ketones
-
Attend scheduled follow-up appointments for HbA1c monitoring (typically at 3–6 months)
Patients should be reassured that gradual glucose improvement is expected and appropriate, and that working collaboratively with their healthcare team optimises outcomes whilst minimising risks.
Scientific References
- Ozempic 0.5 mg solution for injection in pre-filled pen - Summary of Product Characteristics (SmPC).
- Ozempic (semaglutide) - European Public Assessment Report.
- Type 2 diabetes in adults: management (NG28).
- Semaglutide, reduction in glycated haemoglobin and the risk of diabetic retinopathy complications.
- Treatment for type 2 diabetes.
Frequently Asked Questions
How long does it take for Ozempic to start working?
Initial blood glucose-lowering effects typically begin within the first week of treatment, though modest initially. Significant improvements in HbA1c are generally observed after 8–12 weeks, with maximum effects achieved once steady-state concentrations are reached at 4–5 weeks.
Can I use Ozempic to treat high blood sugar emergencies?
No, Ozempic is not a rescue medication for acute hyperglycaemia. It works gradually over weeks to months and should not be used to treat sudden high blood sugar episodes, which may require rapid-acting insulin or urgent medical attention.
What side effects should I expect when starting Ozempic?
The most common side effects are gastrointestinal, including nausea (approximately 15% of patients), vomiting, diarrhoea, and constipation. These effects are typically mild to moderate, transient, and often improve after 4–8 weeks as your body adapts to the medication.
The health-related content published on this site is based on credible scientific sources and is periodically reviewed to ensure accuracy and relevance. Although we aim to reflect the most current medical knowledge, the material is meant for general education and awareness only.
The information on this site is not a substitute for professional medical advice. For any health concerns, please speak with a qualified medical professional. By using this information, you acknowledge responsibility for any decisions made and understand we are not liable for any consequences that may result.
Heading 1
Heading 2
Heading 3
Heading 4
Heading 5
Heading 6
Lorem ipsum dolor sit amet, consectetur adipiscing elit, sed do eiusmod tempor incididunt ut labore et dolore magna aliqua. Ut enim ad minim veniam, quis nostrud exercitation ullamco laboris nisi ut aliquip ex ea commodo consequat. Duis aute irure dolor in reprehenderit in voluptate velit esse cillum dolore eu fugiat nulla pariatur.
Block quote
Ordered list
- Item 1
- Item 2
- Item 3
Unordered list
- Item A
- Item B
- Item C
Bold text
Emphasis
Superscript
Subscript