Saxenda (liraglutide 3.0 mg) is a GLP-1 receptor agonist licensed in the UK for weight management in adults with obesity or overweight with comorbidities. For individuals living with autoimmune diseases such as rheumatoid arthritis, inflammatory bowel disease, or thyroid disorders, questions often arise about whether Saxenda is safe and appropriate. Whilst liraglutide primarily targets metabolic pathways rather than immune function, limited evidence exists specifically for autoimmune populations. This article examines the safety considerations, monitoring requirements, and alternative weight management options for people with autoimmune conditions considering Saxenda, emphasising the importance of individualised medical supervision and shared decision-making with relevant specialists.
Summary: Saxenda may be used in patients with autoimmune disease, but requires individualised assessment and close medical supervision due to limited specific evidence and potential complications.
- Saxenda is a GLP-1 receptor agonist that regulates appetite and glucose metabolism rather than directly affecting immune function.
- Gastrointestinal side effects may complicate monitoring in inflammatory bowel disease, and thyroid surveillance is important in autoimmune thyroid conditions.
- Baseline investigations should include renal function, thyroid function, glucose control, and lipid profile before initiating treatment.
- Treatment requires regular monitoring of weight loss progress, adverse effects, blood glucose, and autoimmune disease activity with specialist input.
- Alternative options include lifestyle modification, orlistat, other GLP-1 agonists, or bariatric surgery depending on individual circumstances and contraindications.
Table of Contents
What Is Saxenda and How Does It Work?
Saxenda (liraglutide 3.0 mg) is a prescription medicine licensed in the UK for weight management in adults with obesity (BMI ≥30 kg/m²) or overweight (BMI ≥27 kg/m²) with at least one weight-related comorbidity, such as type 2 diabetes, hypertension, or dyslipidaemia. It is also licensed for weight management in adolescents aged 12 years and above with obesity and body weight above 60 kg. Saxenda is administered as a once-daily subcutaneous injection and should be used alongside a reduced-calorie diet and increased physical activity.
The active ingredient, liraglutide, is a glucagon-like peptide-1 (GLP-1) receptor agonist. GLP-1 is a naturally occurring hormone that plays a key role in regulating appetite and glucose metabolism. Saxenda works by mimicking the effects of GLP-1, binding to receptors in the brain (particularly in areas that control appetite) and the gastrointestinal tract. This mechanism leads to increased feelings of fullness (satiety), reduced hunger, and delayed gastric emptying, which collectively help individuals consume fewer calories.
In addition to its effects on appetite, liraglutide also influences insulin secretion in a glucose-dependent manner, meaning it stimulates insulin release when blood glucose levels are elevated. This dual action on appetite regulation and glucose homeostasis makes Saxenda particularly beneficial for individuals with obesity and metabolic complications. Clinical trials (SCALE programme) have demonstrated that Saxenda, when combined with lifestyle modifications, can lead to clinically significant weight loss—typically around 5–10% of initial body weight over one year.
It is important to note that Saxenda is not suitable for everyone. The UK SmPC includes special warnings regarding thyroid C-cell tumours observed in rodent studies, though the clinical relevance to humans remains uncertain. Saxenda should not be used in patients with type 1 diabetes or diabetic ketoacidosis, and caution is advised in those with severe gastrointestinal disease including gastroparesis. It should not be used during pregnancy (and should be discontinued if pregnancy occurs) or breastfeeding. Treatment starts with a dose of 0.6 mg daily, increasing weekly by 0.6 mg to the maintenance dose of 3.0 mg daily. Saxenda should not be used in combination with other GLP-1 receptor agonists. Patients should always consult their GP or specialist before starting treatment to ensure it is appropriate for their individual circumstances.
Safety Considerations for Autoimmune Conditions
Individuals with autoimmune diseases often face unique challenges when considering weight management medications like Saxenda. Autoimmune conditions—such as rheumatoid arthritis, systemic lupus erythematosus, inflammatory bowel disease, psoriasis, and thyroid disorders—occur when the immune system mistakenly attacks the body's own tissues. Many people with autoimmune diseases take immunosuppressive or immunomodulatory medications, and concerns naturally arise about potential drug interactions or effects on immune function.
Evidence specifically examining Saxenda use in patients with autoimmune conditions is limited, as these populations are often underrepresented in clinical trials. Liraglutide's mechanism of action primarily targets GLP-1 receptors involved in metabolic regulation rather than directly modulating immune system activity. However, decisions about using Saxenda in autoimmune disease should be made on a case-by-case basis, ideally in consultation with relevant specialists.
Certain adverse effects of Saxenda warrant particular attention in autoimmune disease patients. Gastrointestinal side effects—including nausea, vomiting, diarrhoea, and constipation—are common, especially during dose escalation. For individuals with inflammatory bowel disease (Crohn's disease or ulcerative colitis), these symptoms may complicate disease monitoring or be mistaken for disease flares. Patients should be counselled about the risk of dehydration from gastrointestinal effects, which could potentially affect renal function. Additionally, Saxenda has been associated with acute pancreatitis in rare cases; patients with autoimmune pancreatitis or those taking medications that increase pancreatitis risk should be counselled accordingly.
Thyroid considerations are also important. Saxenda carries a warning regarding thyroid C-cell tumours observed in rodent studies, though relevance to humans remains uncertain. Patients with autoimmune thyroid disease (Hashimoto's thyroiditis or Graves' disease) should have thyroid function monitored as clinically indicated for their underlying condition. Any new neck swelling, hoarseness, or difficulty swallowing should prompt immediate medical review. Saxenda may also increase the risk of gallbladder disease, with symptoms including right upper quadrant pain and jaundice requiring prompt medical attention.
If you experience any suspected side effects while taking Saxenda, report them through the MHRA Yellow Card Scheme.
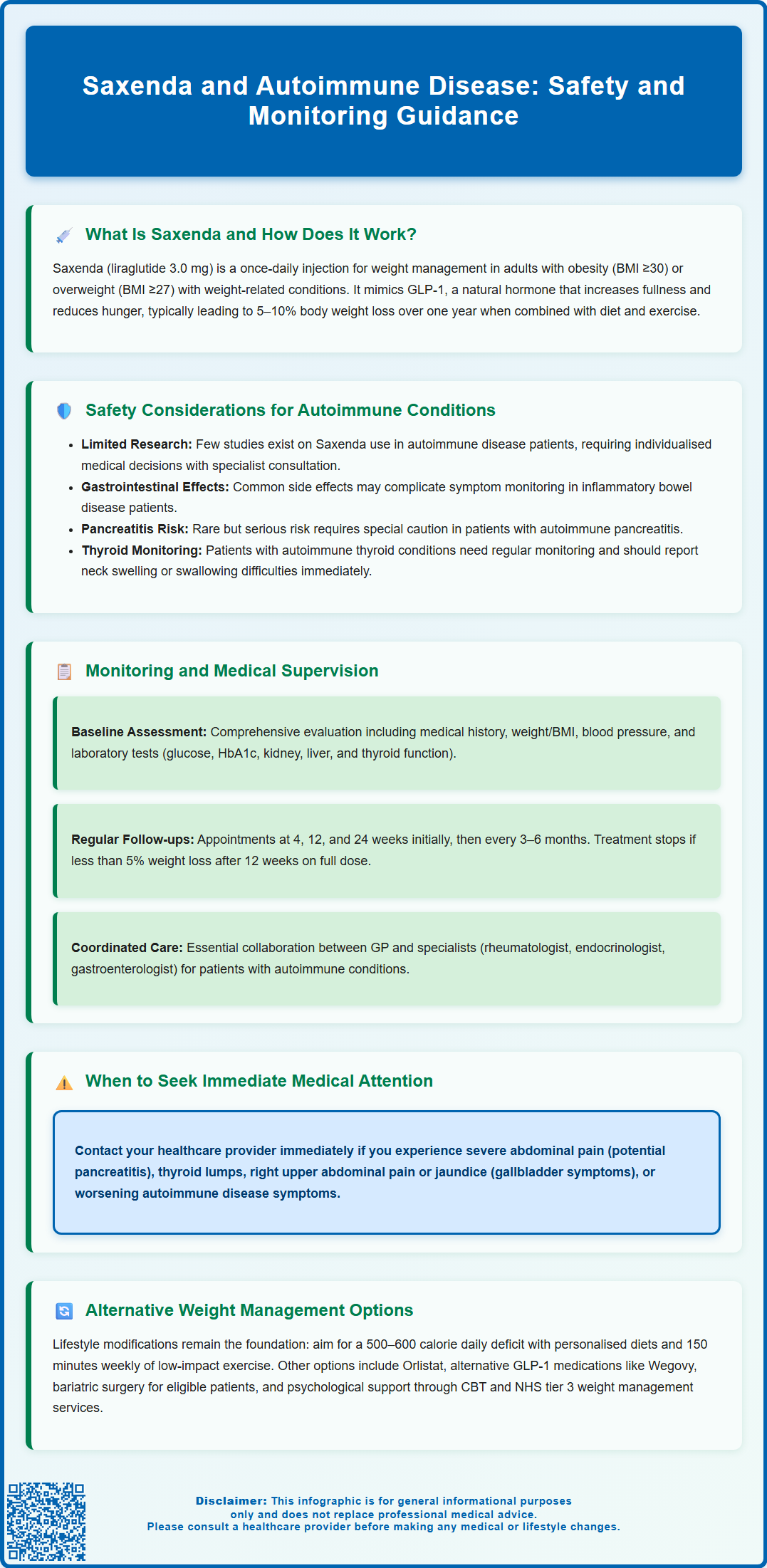
Monitoring and Medical Supervision While Taking Saxenda
Close medical supervision is essential for anyone taking Saxenda, particularly those with underlying autoimmune conditions or complex medical histories. Before initiating treatment, a comprehensive assessment should include a detailed medical history, current medications (including over-the-counter and herbal supplements), baseline weight and BMI, blood pressure, and relevant laboratory investigations.
Baseline investigations typically considered in clinical practice include:
-
Fasting glucose and HbA1c – to assess glycaemic control, especially in patients with diabetes or prediabetes
-
Lipid profile – to evaluate cardiovascular risk factors
-
Renal function (eGFR and creatinine) – while no routine dose adjustment is required for renal impairment, monitoring is prudent, especially if dehydration occurs from gastrointestinal side effects
-
Liver function tests – to establish baseline hepatic function
-
Thyroid function tests (TSH, free T4) – particularly important in patients with known or suspected thyroid disease
During treatment, patients should be reviewed regularly—typically at 4, 12, and 24 weeks initially, then every 3–6 months. At each visit, clinicians should assess:
-
Weight loss progress – Saxenda should be discontinued if patients have not lost at least 5% of initial body weight after 12 weeks on the 3.0 mg daily dose
-
Tolerability and adverse effects – particularly gastrointestinal symptoms, which usually improve over time
-
Blood glucose monitoring – especially in diabetic patients, as weight loss and liraglutide's effects may necessitate adjustment of other glucose-lowering medications (particularly sulfonylureas or insulin) to prevent hypoglycaemia
-
Blood pressure and heart rate – liraglutide can cause modest increases in heart rate
-
Autoimmune disease activity – any changes in symptoms or disease control should be discussed with the relevant specialist
Patients should be advised to contact their GP immediately if they experience severe abdominal pain (possible pancreatitis), signs of thyroid masses, symptoms of gallbladder disease (right upper quadrant pain, jaundice), or worsening of their autoimmune condition. Saxenda should not be used alongside other GLP-1 receptor agonists. Shared decision-making between the patient, GP, and specialist (rheumatologist, endocrinologist, gastroenterologist) ensures coordinated, safe care.
Alternative Weight Management Options for Autoimmune Disease
For individuals with autoimmune diseases who are unable to take Saxenda or prefer alternative approaches, several evidence-based weight management strategies are available. The cornerstone of any weight management programme remains lifestyle modification, including dietary changes and physical activity tailored to individual capabilities and disease limitations.
Dietary interventions should be personalised and may include:
-
Calorie-controlled diets – aiming for a 500–600 kcal daily deficit to achieve gradual, sustainable weight loss
-
Mediterranean-style diets – rich in fruits, vegetables, whole grains, and healthy fats, with anti-inflammatory properties that may benefit autoimmune conditions
-
Low-glycaemic index diets – helpful for managing insulin resistance and metabolic syndrome
-
Referral to specialist dietitians – particularly valuable for patients with inflammatory bowel disease or food intolerances
Physical activity recommendations must account for disease-specific limitations. Patients with rheumatoid arthritis or lupus may benefit from low-impact exercises such as swimming, cycling, or tai chi. The UK Chief Medical Officers recommend at least 150 minutes of moderate-intensity activity weekly, but this should be adapted to individual functional capacity and disease activity. Physiotherapy referral can help develop safe, effective exercise programmes.
Alternative pharmacological options include:
-
Orlistat – a lipase inhibitor that reduces dietary fat absorption; available over-the-counter (Alli 60 mg) or on prescription (Xenical 120 mg). Gastrointestinal side effects may limit use in inflammatory bowel disease
-
Semaglutide 2.4 mg (Wegovy) – another GLP-1 receptor agonist with similar considerations to Saxenda
-
Naltrexone-bupropion (Mysimba) – licensed in the UK but not currently recommended by NICE and has limited NHS availability. Contraindicated in patients taking opioid medications and those with seizure disorders
Bariatric surgery (gastric bypass, sleeve gastrectomy) may be considered for patients with BMI ≥40 kg/m² or ≥35 kg/m² with comorbidities who have not achieved adequate weight loss with non-surgical methods. NICE guidance also includes specific criteria for patients with type 2 diabetes at lower BMI thresholds. Multidisciplinary assessment is essential, particularly regarding immunosuppressive medication management perioperatively.
Psychological support through cognitive behavioural therapy (CBT) or weight management programmes can address emotional eating, body image concerns, and the psychological impact of chronic disease. Many NHS areas offer tier 3 weight management services that provide comprehensive, multidisciplinary support tailored to complex medical needs.
Frequently Asked Questions
Can I take Saxenda if I have an autoimmune disease?
Saxenda may be suitable for some patients with autoimmune conditions, but decisions must be made individually in consultation with your GP and relevant specialists. Limited specific evidence exists for autoimmune populations, so careful monitoring and consideration of your particular condition and medications are essential.
Does Saxenda affect the immune system?
Saxenda primarily targets GLP-1 receptors involved in appetite regulation and glucose metabolism rather than directly modulating immune system activity. However, any new medication should be discussed with your healthcare team to ensure it is appropriate for your individual circumstances.
What monitoring is needed when taking Saxenda with an autoimmune condition?
Regular monitoring should include weight loss progress, tolerability, blood glucose (especially in diabetes), thyroid function if relevant, and autoimmune disease activity. Reviews typically occur at 4, 12, and 24 weeks initially, then every 3–6 months, with coordination between your GP and specialist.
The health-related content published on this site is based on credible scientific sources and is periodically reviewed to ensure accuracy and relevance. Although we aim to reflect the most current medical knowledge, the material is meant for general education and awareness only.
The information on this site is not a substitute for professional medical advice. For any health concerns, please speak with a qualified medical professional. By using this information, you acknowledge responsibility for any decisions made and understand we are not liable for any consequences that may result.
Heading 1
Heading 2
Heading 3
Heading 4
Heading 5
Heading 6
Lorem ipsum dolor sit amet, consectetur adipiscing elit, sed do eiusmod tempor incididunt ut labore et dolore magna aliqua. Ut enim ad minim veniam, quis nostrud exercitation ullamco laboris nisi ut aliquip ex ea commodo consequat. Duis aute irure dolor in reprehenderit in voluptate velit esse cillum dolore eu fugiat nulla pariatur.
Block quote
Ordered list
- Item 1
- Item 2
- Item 3
Unordered list
- Item A
- Item B
- Item C
Bold text
Emphasis
Superscript
Subscript