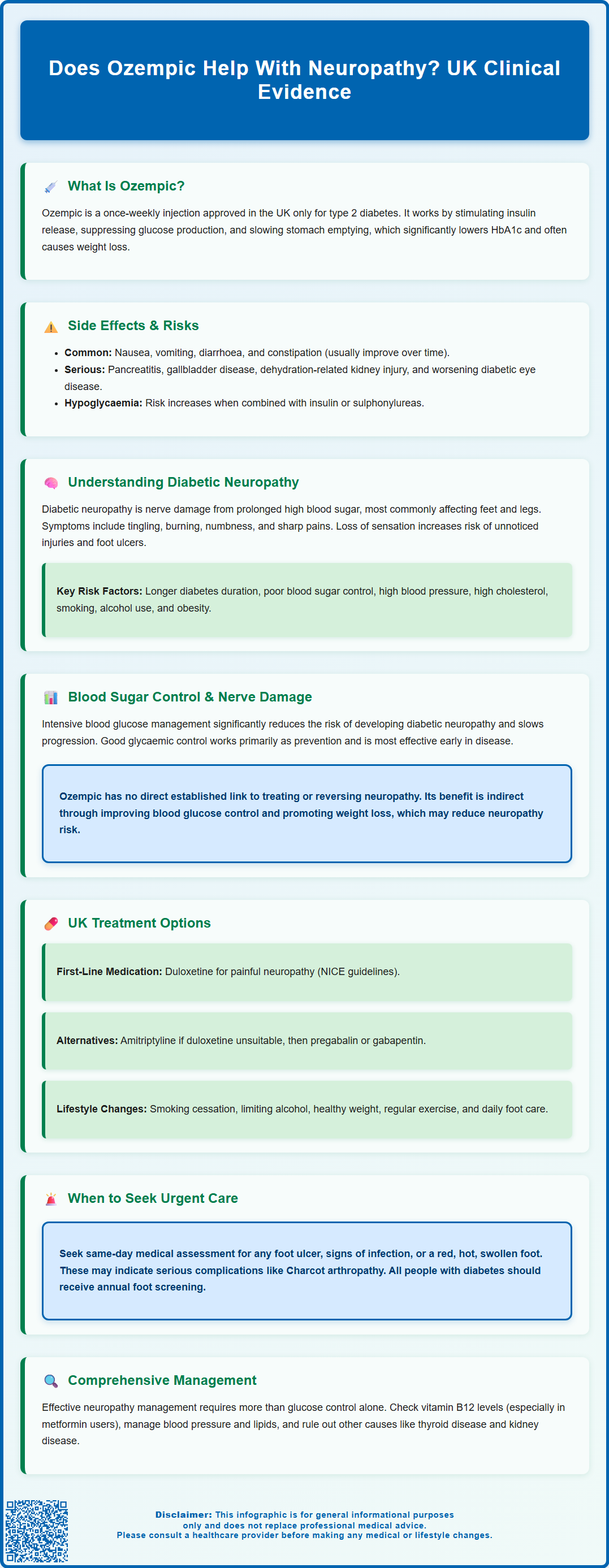
Does Ozempic help with neuropathy? Many people with type 2 diabetes wonder whether this GLP-1 receptor agonist can address nerve damage alongside blood sugar control. Ozempic (semaglutide) is licensed in the UK exclusively for managing type 2 diabetes mellitus. Whilst it does not directly treat diabetic neuropathy, its ability to improve glycaemic control and support weight loss may indirectly reduce the risk of developing nerve damage or slow its progression. Understanding how blood glucose management influences neuropathy is essential for anyone living with diabetes and experiencing symptoms such as tingling, numbness, or pain in the extremities.
Summary: Ozempic does not directly treat diabetic neuropathy, but may indirectly reduce the risk or slow progression by improving blood glucose control and promoting weight loss.
- Ozempic (semaglutide) is a GLP-1 receptor agonist licensed in the UK only for type 2 diabetes mellitus treatment.
- The medication works by stimulating insulin secretion, suppressing glucagon release, and slowing gastric emptying in a glucose-dependent manner.
- Improved glycaemic control through medications like Ozempic helps prevent or slow diabetic neuropathy by reducing nerve exposure to toxic glucose metabolites.
- NICE guidance recommends duloxetine as first-line treatment for painful diabetic neuropathy, with amitriptyline, pregabalin, or gabapentin as alternatives.
- All people with diabetes should receive annual foot screening, and urgent assessment is required for any foot ulcer or signs of infection.
Table of Contents
What Is Ozempic and How Does It Work?
Ozempic (semaglutide) is a prescription medication licensed in the UK for the treatment of type 2 diabetes mellitus only. It belongs to a class of drugs known as glucagon-like peptide-1 (GLP-1) receptor agonists, which work by mimicking the action of a naturally occurring hormone that regulates blood glucose levels.
The mechanism of action of Ozempic involves several key processes. Firstly, it stimulates insulin secretion from the pancreas in a glucose-dependent manner, meaning insulin is released only when blood sugar levels are elevated. Secondly, Ozempic suppresses glucagon release, a hormone that raises blood glucose by promoting glucose production in the liver. Thirdly, it slows gastric emptying, which helps to moderate the rise in blood sugar after meals. Additionally, many patients experience reduced appetite and weight loss, which can further improve glycaemic control.
Ozempic is administered as a once-weekly subcutaneous injection, starting at 0.25 mg for 4 weeks, then increasing to 0.5 mg, with a possible further increase to 1 mg if needed. According to NICE guidance (NG28), GLP-1 receptor agonists like Ozempic may be considered as part of a comprehensive diabetes management plan in specific circumstances, such as when a person has a BMI of 35 kg/m² or above, or when weight loss would benefit obesity-related comorbidities.
The medication has been shown in clinical trials to significantly reduce HbA1c levels (a measure of average blood glucose over three months) and is generally well tolerated. Common side effects include nausea, vomiting, diarrhoea, and constipation, which often improve over time. When used with insulin or sulfonylureas, there is an increased risk of hypoglycaemia, and dose adjustments of these medications may be needed.
Important safety considerations include the risk of pancreatitis (seek urgent medical attention for severe, persistent abdominal pain), gallbladder disease, dehydration leading to acute kidney injury (particularly with vomiting or diarrhoea), and potential worsening of diabetic retinopathy in those with pre-existing disease. Ozempic is not recommended during pregnancy or breastfeeding.
Patients should be monitored regularly by their healthcare team to assess treatment response and manage any adverse effects. If you experience side effects, report them via the MHRA Yellow Card Scheme (yellowcard.mhra.gov.uk).
Understanding Diabetic Neuropathy and Its Causes
Diabetic neuropathy is one of the most common complications of diabetes, affecting a significant proportion of people with diabetes at some point during their illness. It refers to nerve damage caused by prolonged exposure to elevated blood glucose levels, which can affect various parts of the nervous system. The most prevalent form is peripheral neuropathy, which typically affects the feet and legs, though hands and arms may also be involved.
The underlying pathophysiology of diabetic neuropathy is complex and multifactorial. Chronic hyperglycaemia leads to metabolic and vascular changes that damage nerve fibres. High glucose levels cause the accumulation of sorbitol and fructose within nerve cells through the polyol pathway, leading to osmotic stress and cellular dysfunction. Additionally, elevated blood sugar promotes the formation of advanced glycation end products (AGEs), which trigger inflammatory responses and oxidative stress, further damaging nerve tissue.
Vascular factors also play a crucial role. Diabetes affects the small blood vessels (microvascular disease) that supply nerves with oxygen and nutrients. Reduced blood flow impairs nerve function and regeneration, contributing to progressive nerve damage. Other risk factors that increase the likelihood of developing diabetic neuropathy include:
-
Duration of diabetes – longer disease duration increases risk
-
Poor glycaemic control – persistently high HbA1c levels
-
Hypertension and dyslipidaemia – cardiovascular risk factors
-
Smoking and excessive alcohol consumption
-
Obesity – particularly central adiposity
Symptoms of peripheral neuropathy vary but commonly include tingling, burning sensations, numbness, and sharp pains in the affected areas. Some patients experience loss of sensation, which increases the risk of unnoticed injuries and foot ulcers. Autonomic neuropathy can affect internal organs, causing problems with digestion, heart rate, blood pressure, and bladder function.
It's important to note that other conditions can cause similar symptoms, and these should be ruled out. In particular, people taking metformin should have their vitamin B12 levels checked if neuropathy symptoms develop, as metformin can reduce B12 absorption. Other causes to consider include thyroid disease, alcohol misuse, and renal disease. Early recognition, comprehensive assessment and management are essential to prevent progression and complications.
How Blood Sugar Control Affects Nerve Damage
The relationship between glycaemic control and diabetic neuropathy is well established through decades of clinical research. The landmark Diabetes Control and Complications Trial (DCCT) in type 1 diabetes and the UK Prospective Diabetes Study (UKPDS) in type 2 diabetes both demonstrated that intensive blood glucose management significantly reduces the risk of developing neuropathy and slows its progression in those already affected.
Maintaining blood glucose levels within target ranges helps to minimise the metabolic disturbances that damage nerve tissue. NICE recommends individualised HbA1c targets for people with type 2 diabetes, commonly 48 mmol/mol (6.5%) for those not on medications that cause hypoglycaemia, and 53 mmol/mol (7%) for those taking insulin or sulfonylureas. When blood glucose is well-controlled, the exposure of nerves to toxic glucose metabolites is reduced. This decreases oxidative stress, limits AGE formation, and preserves the function of the small blood vessels supplying peripheral nerves.
However, it is important to note that improved glycaemic control works primarily as a preventive measure and is most effective when implemented early in the disease course. Once significant nerve damage has occurred, the potential for reversal is limited, though further deterioration can often be slowed or halted. Some patients may experience a rare phenomenon called treatment-induced neuropathy, where rapid improvement in blood glucose control temporarily worsens neuropathic symptoms. If this occurs, patients should discuss it with their diabetes team, as it typically resolves over time.
Regarding Ozempic specifically, there is no official direct link established between semaglutide and the treatment or reversal of existing diabetic neuropathy. The medication's primary benefit for nerve health is indirect, achieved through its ability to improve overall glycaemic control and promote weight loss. By helping patients achieve and maintain lower HbA1c levels, Ozempic may contribute to reducing the risk of developing neuropathy or slowing its progression as part of comprehensive diabetes management.
Patients should understand that neuropathy management requires a multifaceted approach beyond glucose control alone, including blood pressure management, lipid control, lifestyle modifications, and specific symptomatic treatments when needed.
Treatment Options for Diabetic Neuropathy in the UK
Management of diabetic neuropathy in the UK follows NICE clinical guideline CG173, which emphasises both disease-modifying strategies and symptomatic relief. The cornerstone of treatment remains optimising glycaemic control through appropriate diabetes medications, dietary modifications, and regular physical activity. All patients should aim for individualised HbA1c targets as recommended by their healthcare team.
Lifestyle interventions play a crucial role in neuropathy management. Patients are advised to:
-
Stop smoking – smoking impairs circulation and worsens nerve damage
-
Limit alcohol intake – excessive alcohol is directly neurotoxic
-
Maintain a healthy weight – obesity contributes to poor glycaemic control
-
Engage in regular exercise – improves circulation and glucose metabolism
-
Practice meticulous foot care – daily inspection, appropriate footwear, and prompt treatment of injuries
For symptomatic relief of painful diabetic neuropathy, NICE recommends a stepwise approach to pharmacological treatment. Duloxetine (a serotonin-norepinephrine reuptake inhibitor) is the recommended first-line treatment. If duloxetine is contraindicated or not tolerated, amitriptyline (a tricyclic antidepressant) may be considered. If these are ineffective, pregabalin or gabapentin may be offered as alternatives. For localised neuropathic pain, topical capsaicin cream might be suitable when oral treatments are inappropriate. Opioid analgesics are generally not recommended for long-term use due to risks of dependence and side effects, though tramadol may be considered for short-term rescue therapy only.
Non-pharmacological approaches can complement medication and include:
-
Physiotherapy – to maintain mobility and strength
-
Psychological support – chronic pain can significantly impact mental health
When to seek medical attention: Patients should contact their GP or diabetes care team if they experience new or worsening symptoms such as numbness, tingling, or pain in their extremities. Urgent same-day assessment by a multidisciplinary foot service is required for any foot ulcer, signs of infection, or a red, hot, swollen foot (which may indicate Charcot arthropathy). All people with diabetes should receive annual diabetic foot screening to detect early signs of neuropathy and assess risk. Those at moderate or high risk should be referred to a foot protection service.
Specialist referral to a diabetologist or neurologist may be appropriate for complex cases or when symptoms are difficult to control with standard treatments. Remember that neuropathy symptoms can sometimes be caused by other conditions, including vitamin B12 deficiency (particularly in those taking metformin), which should be investigated and treated appropriately.
Scientific References
Frequently Asked Questions
Can Ozempic reverse existing diabetic neuropathy?
No, Ozempic cannot reverse established nerve damage. However, by improving blood glucose control, it may help slow the progression of diabetic neuropathy and reduce the risk of further nerve damage when used as part of comprehensive diabetes management.
What is the first-line treatment for painful diabetic neuropathy in the UK?
According to NICE guidance, duloxetine is the recommended first-line pharmacological treatment for painful diabetic neuropathy. If duloxetine is unsuitable, amitriptyline may be considered, followed by pregabalin or gabapentin as alternatives.
How does good blood sugar control prevent diabetic neuropathy?
Maintaining blood glucose within target ranges reduces nerve exposure to toxic glucose metabolites, decreases oxidative stress, limits formation of advanced glycation end products, and preserves function of small blood vessels supplying peripheral nerves, thereby preventing or slowing neuropathy development.
The health-related content published on this site is based on credible scientific sources and is periodically reviewed to ensure accuracy and relevance. Although we aim to reflect the most current medical knowledge, the material is meant for general education and awareness only.
The information on this site is not a substitute for professional medical advice. For any health concerns, please speak with a qualified medical professional. By using this information, you acknowledge responsibility for any decisions made and understand we are not liable for any consequences that may result.
Heading 1
Heading 2
Heading 3
Heading 4
Heading 5
Heading 6
Lorem ipsum dolor sit amet, consectetur adipiscing elit, sed do eiusmod tempor incididunt ut labore et dolore magna aliqua. Ut enim ad minim veniam, quis nostrud exercitation ullamco laboris nisi ut aliquip ex ea commodo consequat. Duis aute irure dolor in reprehenderit in voluptate velit esse cillum dolore eu fugiat nulla pariatur.
Block quote
Ordered list
- Item 1
- Item 2
- Item 3
Unordered list
- Item A
- Item B
- Item C
Bold text
Emphasis
Superscript
Subscript