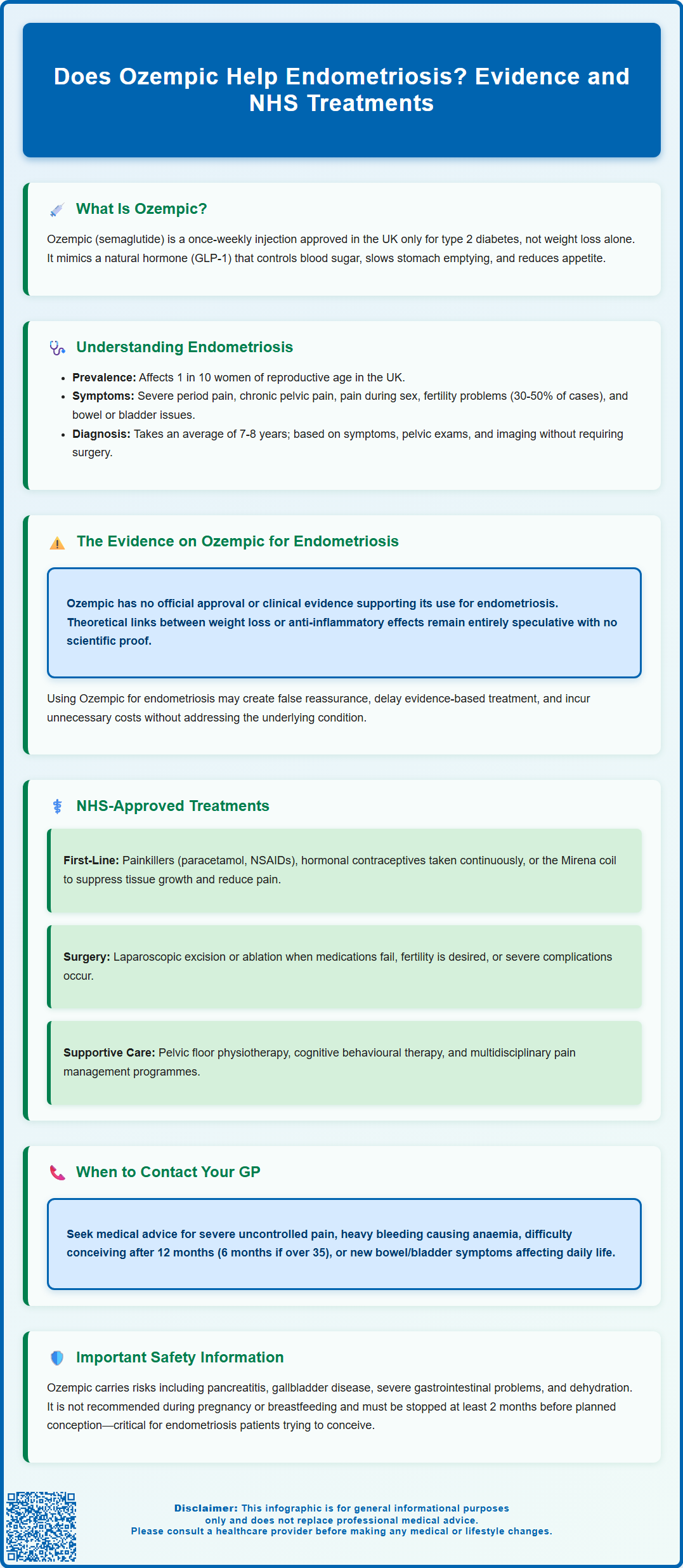
Ozempic (semaglutide) is a GLP-1 receptor agonist licensed in the UK exclusively for type 2 diabetes management, not for endometriosis treatment. Endometriosis, affecting approximately 1 in 10 women of reproductive age, is a chronic gynaecological condition causing pelvic pain, painful periods, and fertility challenges. Whilst some have speculated about potential metabolic or anti-inflammatory benefits of Ozempic for endometriosis, there is currently no clinical evidence or regulatory approval supporting this use. This article examines the science behind Ozempic, explores why it is not indicated for endometriosis, and outlines NHS-approved, evidence-based treatments that effectively manage this debilitating condition.
Summary: Ozempic (semaglutide) is not approved or clinically proven to treat endometriosis and should not be used for this condition.
- Ozempic is a GLP-1 receptor agonist licensed exclusively for type 2 diabetes management in the UK, not for endometriosis.
- No robust clinical trials have investigated semaglutide's efficacy or safety for endometriosis treatment.
- Off-label use carries risks including gastrointestinal adverse effects, pancreatitis, gallbladder disease, and is not recommended during pregnancy.
- Evidence-based endometriosis treatments include hormonal contraceptives, progestogens, GnRH analogues, and surgical interventions guided by NICE.
- Patients with suspected endometriosis should consult their GP or gynaecologist for appropriate NHS-approved management options.
Table of Contents
What Is Ozempic and How Does It Work?
Ozempic (semaglutide) is a prescription medication licensed in the UK for the treatment of type 2 diabetes mellitus. It belongs to a class of drugs known as glucagon-like peptide-1 (GLP-1) receptor agonists. The Medicines and Healthcare products Regulatory Agency (MHRA) has approved Ozempic specifically for glycaemic control in adults with type 2 diabetes, either as monotherapy or in combination with other glucose-lowering medicines.
The mechanism of action centres on mimicking the naturally occurring hormone GLP-1, which is released by the intestine in response to food intake. Semaglutide works by:
-
Stimulating insulin secretion from pancreatic beta cells in a glucose-dependent manner
-
Suppressing glucagon release, which reduces hepatic glucose production
-
Slowing gastric emptying, leading to reduced appetite and food intake
-
Acting on appetite centres in the brain, promoting satiety
These combined effects result in improved blood glucose control and, as a secondary benefit, significant weight loss in many patients. The medication is administered once weekly via subcutaneous injection, typically starting at 0.25 mg and titrating up to maintenance doses of 0.5 mg, 1 mg or 2 mg depending on individual response and tolerability.
Whilst Ozempic has gained considerable attention for its weight management effects, it is important to emphasise that it is not licensed for weight loss alone in the UK. A related formulation, Wegovy (also semaglutide but at higher doses), has separate MHRA approval specifically for weight management.
Common adverse effects of Ozempic include nausea, vomiting, diarrhoea, constipation, and abdominal discomfort, particularly during dose escalation. Important safety considerations include:
-
Not recommended during pregnancy or breastfeeding; effective contraception should be used during treatment
-
Should be discontinued at least 2 months before a planned pregnancy
-
Risk of pancreatitis – seek urgent medical attention for severe, persistent abdominal pain
-
Increased risk of gallbladder disease including cholelithiasis and cholecystitis
-
Potential risk of diabetic retinopathy complications in people with type 2 diabetes
-
Risk of hypoglycaemia when used with insulin or sulfonylureas
-
Risk of dehydration leading to acute kidney injury, particularly during initial treatment
If you experience side effects, report them through the MHRA Yellow Card Scheme (yellowcard.mhra.gov.uk).
Understanding Endometriosis: Symptoms and Current Treatments
Endometriosis is a chronic gynaecological condition affecting approximately 1 in 10 women and people assigned female at birth of reproductive age in the UK. It occurs when tissue similar to the endometrium (the lining of the womb) grows outside the uterus, commonly on the ovaries, fallopian tubes, pelvic peritoneum, and occasionally on more distant organs. This ectopic endometrial-like tissue responds to hormonal changes during the menstrual cycle, leading to inflammation, scarring, and adhesion formation.
Common symptoms include:
-
Chronic pelvic pain, often cyclical and worsening during menstruation
-
Dysmenorrhoea (painful periods) that may be severe and debilitating
-
Dyspareunia (pain during or after sexual intercourse)
-
Subfertility or infertility, affecting approximately 30–50% of women with endometriosis
-
Gastrointestinal symptoms such as painful bowel movements, bloating, and altered bowel habit
-
Urinary symptoms including dysuria and frequency
-
Chronic fatigue and reduced quality of life
Diagnosis can be challenging, with an average delay of 7–8 years from symptom onset to confirmed diagnosis in the UK. Diagnosis may involve pelvic examination and imaging (transvaginal ultrasound is typically first-line, with MRI used for suspected deep disease). It's important to note that normal imaging does not exclude endometriosis. While laparoscopy remains an important diagnostic tool, NICE guidance supports diagnosis and treatment based on clinical features and imaging without necessarily requiring histological confirmation.
The pathophysiology of endometriosis is multifactorial, involving retrograde menstruation, genetic predisposition, immune dysfunction, and inflammatory processes. Some research suggests possible associations between endometriosis and metabolic factors including insulin resistance, though these relationships remain under investigation and are not definitively established. Current evidence-based treatments focus on symptom management and fertility preservation rather than cure.
Potential Benefits and Risks of Ozempic for Endometriosis
There is currently no official link or clinical evidence supporting the use of Ozempic (semaglutide) for the treatment of endometriosis. The medication is not licensed by the MHRA for this indication, and no robust clinical trials have investigated its efficacy or safety specifically for endometriosis management. It is crucial that patients understand this distinction, as off-label use carries potential risks without established benefits.
Some theoretical considerations have emerged in scientific discussion, though these remain speculative and unproven:
-
Weight management: Given that obesity may exacerbate inflammatory processes and some endometriosis symptoms, weight loss achieved through GLP-1 agonists might theoretically improve overall metabolic health. However, there is no evidence that weight loss specifically improves endometriosis lesions or core symptoms.
-
Insulin resistance: Emerging research suggests possible links between insulin resistance and endometriosis severity, though causality remains unclear. Whilst semaglutide improves insulin sensitivity in diabetic patients, extrapolating this to endometriosis treatment is scientifically unfounded.
-
Anti-inflammatory effects: GLP-1 receptor agonists demonstrate some anti-inflammatory properties in preclinical studies, but whether these translate to meaningful effects on endometriosis-related inflammation is entirely unknown.
Potential risks of using Ozempic without appropriate indication include:
-
Gastrointestinal adverse effects (nausea, vomiting, diarrhoea) that may worsen quality of life
-
Risk of pancreatitis – seek urgent medical attention for severe, persistent abdominal pain
-
Increased risk of gallbladder disease including gallstones and inflammation
-
Not recommended during pregnancy or breastfeeding – particularly relevant for those with endometriosis who may be trying to conceive
-
Should be discontinued at least 2 months before planned pregnancy
-
Risk of hypoglycaemia when used with insulin or sulfonylureas
-
Risk of dehydration leading to acute kidney injury
-
Unnecessary cost and diversion from evidence-based treatments
-
False reassurance that may delay appropriate endometriosis management
Of note, while semaglutide slows gastric emptying, the UK product information states it does not have a clinically relevant effect on the absorption of oral contraceptives.
Patients considering any off-label medication should have thorough discussions with their GP or specialist gynaecologist about evidence-based alternatives. Any suspected side effects should be reported via the MHRA Yellow Card Scheme.
NHS-Approved Treatments for Endometriosis Management
The National Institute for Health and Care Excellence (NICE) provides comprehensive guidance (NG73) on the diagnosis and management of endometriosis. Treatment approaches are individualised based on symptom severity, fertility wishes, and patient preferences, typically following a stepwise approach. Importantly, treatment should not be delayed while awaiting diagnostic laparoscopy if endometriosis is suspected.
First-line pharmacological management includes:
-
Analgesia: Paracetamol and non-steroidal anti-inflammatory drugs (NSAIDs) such as ibuprofen or mefenamic acid for pain relief
-
Hormonal contraceptives: Combined oral contraceptive pill (COCP) or progestogen-only pill, often used continuously to suppress menstruation
-
Progestogens: Including norethisterone, desogestrel, or medroxyprogesterone acetate, which suppress endometrial tissue growth
-
Levonorgestrel intrauterine system (LNG-IUS): The Mirena coil provides local progestogenic effects and may reduce dysmenorrhoea and menstrual bleeding
Second-line hormonal treatments (typically initiated by specialists):
- GnRH analogues (goserelin, leuprorelin): Create a temporary menopausal state, highly effective for pain relief. While typically used for up to 6 months initially, longer-term use may be considered with appropriate add-back hormone replacement therapy (HRT) under specialist supervision.
Surgical interventions are considered when:
-
Medical management fails to control symptoms adequately
-
Fertility is a primary concern
-
Endometriomas (ovarian cysts) or severe adhesions are present
-
Deep infiltrating endometriosis affects bowel or bladder
Laparoscopic excision or ablation of endometriotic lesions, performed in specialist endometriosis centres, can provide significant symptom relief. In severe, refractory cases, hysterectomy with bilateral salpingo-oophorectomy may be discussed, though this is reserved for women who have completed their families.
Supportive measures include:
-
Physiotherapy: Pelvic floor physiotherapy for chronic pelvic pain
-
Psychological support: Cognitive behavioural therapy (CBT) or counselling
-
Pain management programmes: Multidisciplinary approaches for chronic pain
When to contact your GP:
-
Severe pelvic pain not controlled by over-the-counter analgesia
-
Heavy menstrual bleeding causing anaemia or significantly affecting quality of life
-
Difficulty conceiving after 12 months of regular unprotected intercourse (or 6 months if over 35)
-
New or worsening bowel or bladder symptoms
-
Symptoms significantly impacting daily activities, work, or relationships
Seek urgent medical attention if you experience sudden severe pelvic pain, fainting, suspected ectopic pregnancy, or symptoms of bowel obstruction.
Patients should be referred to gynaecology services if endometriosis is suspected or if first-line treatments prove inadequate. Specialist endometriosis centres, designated by the British Society for Gynaecological Endoscopy (BSGE), provide multidisciplinary care for complex cases. The NHS also supports patient access to endometriosis support groups and educational resources through organisations such as Endometriosis UK, which can provide valuable peer support and evidence-based information.
Frequently Asked Questions
Is Ozempic approved for treating endometriosis in the UK?
No, Ozempic (semaglutide) is not approved by the MHRA for endometriosis treatment. It is licensed exclusively for type 2 diabetes management, and no clinical evidence supports its use for endometriosis.
What are the NHS-recommended treatments for endometriosis?
NHS-approved treatments include hormonal contraceptives, progestogens, the levonorgestrel intrauterine system (Mirena coil), GnRH analogues, and surgical interventions such as laparoscopic excision. NICE guidance (NG73) recommends individualised, stepwise management based on symptoms and fertility wishes.
What are the risks of using Ozempic without appropriate medical indication?
Off-label use of Ozempic carries risks including gastrointestinal adverse effects, pancreatitis, gallbladder disease, and is not recommended during pregnancy or breastfeeding. It may also delay appropriate endometriosis management and incur unnecessary costs without proven benefit.
The health-related content published on this site is based on credible scientific sources and is periodically reviewed to ensure accuracy and relevance. Although we aim to reflect the most current medical knowledge, the material is meant for general education and awareness only.
The information on this site is not a substitute for professional medical advice. For any health concerns, please speak with a qualified medical professional. By using this information, you acknowledge responsibility for any decisions made and understand we are not liable for any consequences that may result.
Heading 1
Heading 2
Heading 3
Heading 4
Heading 5
Heading 6
Lorem ipsum dolor sit amet, consectetur adipiscing elit, sed do eiusmod tempor incididunt ut labore et dolore magna aliqua. Ut enim ad minim veniam, quis nostrud exercitation ullamco laboris nisi ut aliquip ex ea commodo consequat. Duis aute irure dolor in reprehenderit in voluptate velit esse cillum dolore eu fugiat nulla pariatur.
Block quote
Ordered list
- Item 1
- Item 2
- Item 3
Unordered list
- Item A
- Item B
- Item C
Bold text
Emphasis
Superscript
Subscript