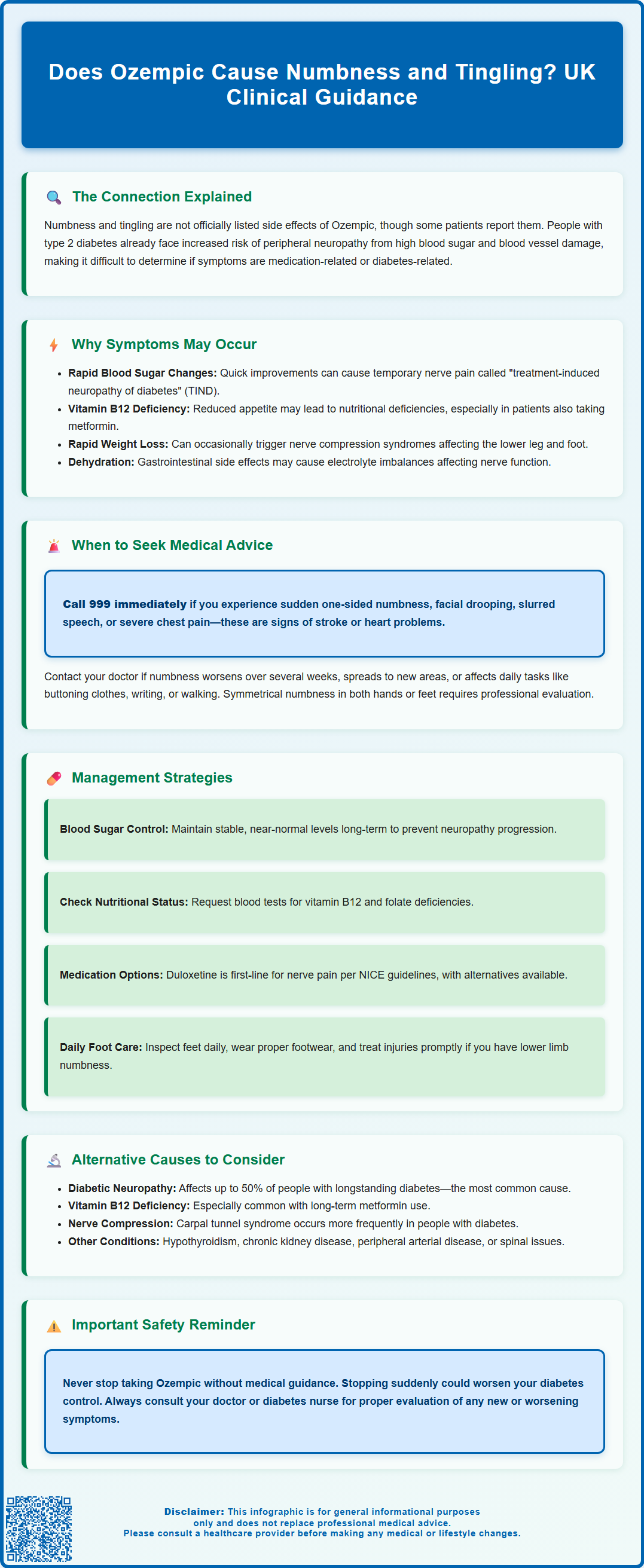
Does Ozempic cause numbness and tingling? Whilst paraesthesia is not listed as a recognised adverse reaction in UK product information, some patients report these sensations during treatment. Ozempic (semaglutide) is a GLP-1 receptor agonist licensed for type 2 diabetes management. No direct causal link exists between semaglutide and peripheral numbness in clinical trials. However, indirect mechanisms—including rapid glycaemic improvement, nutritional deficiencies, or underlying diabetic neuropathy—may explain these symptoms. People with type 2 diabetes already face increased neuropathy risk due to chronic hyperglycaemia. If you experience new or worsening numbness whilst taking Ozempic, consult your GP or diabetes specialist for thorough assessment.
Summary: Ozempic does not directly cause numbness and tingling according to UK product information, though some patients report paraesthesia through indirect mechanisms such as rapid glycaemic improvement or nutritional deficiencies.
- Semaglutide (Ozempic) is a GLP-1 receptor agonist licensed in the UK for type 2 diabetes treatment.
- Paraesthesia is not listed as an adverse reaction in the Summary of Product Characteristics or patient information leaflet.
- Rapid blood glucose improvement may trigger treatment-induced neuropathy of diabetes, causing temporary nerve symptoms.
- Vitamin B12 deficiency—common with metformin use—is a recognised cause of peripheral neuropathy and tingling.
- Progressive, bilateral, or functionally impairing numbness requires GP assessment to identify reversible causes.
- NICE recommends duloxetine as first-line treatment for painful diabetic neuropathy if symptomatic relief is needed.
Table of Contents
Does Ozempic Cause Numbness and Tingling?
Ozempic (semaglutide) is a glucagon-like peptide-1 (GLP-1) receptor agonist licensed in the UK for the treatment of type 2 diabetes mellitus. For weight management, a different semaglutide product called Wegovy is licensed in the UK. Whilst numbness and tingling (paraesthesia) are not listed as adverse reactions in the Summary of Product Characteristics (SmPC) or patient information leaflet for Ozempic, some individuals have reported these sensations during treatment.
There is no established causal link between Ozempic and peripheral paraesthesia in clinical trial data. However, several indirect mechanisms may explain why some patients experience numbness or tingling whilst on this medication. These sensations can occur in the hands, feet, fingers, or toes, and may be transient or persistent depending on the underlying cause.
It is important to recognise that people with type 2 diabetes are already at increased risk of developing peripheral neuropathy due to chronic hyperglycaemia and microvascular damage. Therefore, distinguishing between medication-related effects and diabetes-related complications can be challenging. Additionally, rapid metabolic changes—such as improved glycaemic control—can sometimes temporarily affect nerve function.
If you are experiencing new or worsening numbness and tingling after starting Ozempic, it is essential to discuss these symptoms with your GP or diabetes specialist nurse. A thorough clinical assessment can help determine whether the symptoms are related to the medication, underlying diabetes, nutritional deficiencies, or other medical conditions. Do not stop taking Ozempic without medical advice, as abrupt discontinuation may affect your diabetes control.
Why Numbness and Tingling May Occur During Ozempic Treatment
Several mechanisms may contribute to the development of numbness and tingling in patients taking Ozempic, although these are largely indirect rather than a direct pharmacological effect of semaglutide itself.
Rapid glycaemic improvement is one potential explanation. When blood glucose levels drop quickly after starting Ozempic, some patients experience a phenomenon known as "treatment-induced neuropathy of diabetes" (TIND) or acute painful diabetic neuropathy. This paradoxical worsening of nerve symptoms can occur when glucose control improves too rapidly (typically a significant drop in HbA1c over a short period), leading to temporary metabolic stress on peripheral nerves. Whilst uncomfortable, this typically resolves over weeks to months as the body adjusts.
Nutritional deficiencies may also play a role, particularly in patients experiencing significant gastrointestinal side effects. Ozempic commonly causes nausea, vomiting, and reduced appetite, which can lead to decreased food intake and potential deficiencies in nutrients essential for nerve health. Vitamin B12 deficiency is particularly relevant, as many people with diabetes also take metformin, which the MHRA has identified as reducing vitamin B12 levels with long-term use. B12 deficiency is a well-recognised cause of peripheral neuropathy and paraesthesia.
Weight loss, whilst generally beneficial, can occasionally be associated with certain nerve compression syndromes. Rapid weight loss has been associated with peroneal neuropathy (affecting the outer part of the lower leg and top of the foot). It's worth noting that obesity and diabetes themselves are risk factors for compression neuropathies such as carpal tunnel syndrome.
Dehydration and electrolyte imbalances (particularly sodium, calcium, or magnesium) resulting from gastrointestinal side effects could theoretically affect nerve function, though this is less commonly reported. These mechanisms are speculative in many cases, and individual patient factors will vary considerably.
When to Seek Medical Advice About Numbness While Taking Ozempic
Whilst mild, transient tingling may not always require urgent attention, certain features warrant prompt medical assessment. Patients should contact their GP or diabetes care team if they experience any of the following:
-
Progressive or worsening symptoms: Numbness or tingling that spreads, intensifies, or does not improve over several weeks should be evaluated. Progressive peripheral neuropathy requires investigation to identify reversible causes.
-
Functional impairment: Difficulty with fine motor tasks (such as buttoning clothes or writing), weakness in the hands or feet, or problems with balance and walking indicate more significant nerve involvement and require clinical assessment.
-
Bilateral and symmetrical symptoms: Numbness affecting both feet or both hands in a "glove and stocking" distribution may suggest diabetic peripheral neuropathy or nutritional deficiency, both of which require investigation and management.
-
Associated symptoms: Seek medical advice if numbness is accompanied by severe pain, burning sensations, muscle weakness, changes in vision, confusion, or signs of infection. These may indicate complications requiring urgent attention. Vision changes should be assessed promptly, as rapid improvement in blood glucose can sometimes worsen diabetic retinopathy in some patients.
-
Diabetic foot problems: If you develop a new foot ulcer, signs of infection (redness, warmth, swelling, discharge), severe pain, or colour changes in your foot, seek same-day referral to a multidisciplinary foot care service as per NICE guidance.
Seek immediate medical attention (call 999 or attend A&E) if you experience sudden onset of numbness affecting one side of the body, facial drooping, slurred speech, or severe chest pain, as these may indicate stroke or other serious cardiovascular events. If urgent advice is needed and your GP is unavailable, contact NHS 111.
Your healthcare provider will likely perform a thorough neurological examination and may arrange blood tests to check HbA1c, vitamin B12, folate, thyroid function, and renal function. Depending on findings, referral to a neurologist or diabetologist may be appropriate. Never discontinue Ozempic without consulting your prescriber, as this may compromise your diabetes management.
Managing Numbness and Tingling on Ozempic
Management of numbness and tingling in patients taking Ozempic depends on identifying and addressing the underlying cause. A stepwise approach is recommended, guided by clinical assessment and investigation results.
Optimising diabetes control remains fundamental. Whilst rapid glucose reduction can paradoxically worsen neuropathic symptoms initially, maintaining stable, near-normal glycaemic control over the long term is the most effective strategy for preventing progression of diabetic neuropathy. Your diabetes team may adjust your Ozempic dose or titration schedule if symptoms are thought to be related to rapid metabolic changes.
Nutritional assessment and supplementation should be considered, particularly if dietary intake has been reduced due to gastrointestinal side effects. Blood tests can identify deficiencies in vitamin B12, folate, or other nutrients. If B12 deficiency is confirmed, treatment typically involves intramuscular hydroxocobalamin injections as per UK guidelines. Oral cyanocobalamin supplements are generally only recommended for dietary deficiency or maintenance therapy where appropriate. Ensuring adequate protein intake and a balanced diet supports overall nerve health.
Symptomatic relief may be necessary for troublesome paraesthesia. NICE guidance (CG173) on neuropathic pain recommends duloxetine as first-line treatment for painful diabetic neuropathy. If duloxetine is contraindicated or not tolerated, alternatives include amitriptyline, gabapentin, or pregabalin. These should be initiated at low doses and titrated according to response and tolerability. Gabapentinoids require dose adjustment in renal impairment and can cause sedation affecting driving ability. Simple analgesia is generally ineffective for neuropathic symptoms, and routine use of opioids is not recommended.
Lifestyle modifications can also help. Regular gentle exercise improves circulation and may reduce neuropathic symptoms. Avoiding alcohol, which can worsen nerve damage, is advisable. Proper foot care is essential for people with diabetes experiencing lower limb numbness—daily inspection, appropriate footwear, and prompt attention to any injuries can prevent serious complications.
If symptoms persist despite these measures, or if an alternative diagnosis is suspected, your GP may refer you to a neurologist for specialist assessment, which may include nerve conduction studies or other investigations.
Alternative Causes of Numbness in People With Type 2 Diabetes
It is crucial to recognise that numbness and tingling in people with type 2 diabetes often have causes unrelated to Ozempic. A comprehensive differential diagnosis should be considered to ensure appropriate investigation and management.
Diabetic peripheral neuropathy is the most common cause of paraesthesia in this population, affecting up to 50% of people with longstanding diabetes. This condition results from chronic hyperglycaemia causing microvascular damage and metabolic changes that impair nerve function. It typically presents as symmetrical numbness, tingling, or burning sensations in a "glove and stocking" distribution, starting in the feet and progressing proximally. Risk factors include poor glycaemic control, longer diabetes duration, hypertension, and dyslipidaemia.
Vitamin B12 deficiency is particularly relevant in people with diabetes, especially those taking metformin long-term, as this medication can reduce B12 levels. The MHRA advises checking B12 levels in patients on metformin who develop symptoms of deficiency, and considering periodic monitoring in those with risk factors. Deficiency causes peripheral neuropathy that may be clinically indistinguishable from diabetic neuropathy.
Nerve compression syndromes such as carpal tunnel syndrome (median nerve compression at the wrist) or ulnar neuropathy (compression at the elbow) are more common in people with diabetes. These typically cause numbness in specific distributions—for example, the thumb, index, and middle fingers in carpal tunnel syndrome.
Other metabolic and systemic causes include hypothyroidism, chronic kidney disease (common in diabetes), alcohol excess, and certain medications. Cervical or lumbar radiculopathy from spinal nerve root compression can cause dermatomal numbness and may be exacerbated by obesity.
Peripheral arterial disease, more prevalent in people with diabetes, can cause exertional calf pain (claudication), cold feet, absent pulses, and delayed healing. Severe cases may present with rest pain, colour changes, or ulceration. A thorough vascular assessment, including examination of peripheral pulses, is important if PAD is suspected.
A comprehensive clinical assessment, alongside appropriate investigations, will help identify the underlying cause and guide targeted treatment. Your healthcare team can coordinate these assessments and ensure you receive appropriate specialist input where needed.
If you believe you have experienced side effects from Ozempic or any other medication, you can report these through the MHRA Yellow Card scheme at yellowcard.mhra.gov.uk.
Frequently Asked Questions
Is numbness a recognised side effect of Ozempic?
No, numbness and tingling are not listed as adverse reactions in UK product information for Ozempic. However, some patients report these symptoms, which may result from indirect mechanisms such as rapid glycaemic improvement or nutritional deficiencies rather than a direct drug effect.
When should I see my GP about numbness whilst taking Ozempic?
Contact your GP if numbness is progressive, affects both hands or feet symmetrically, impairs function (such as difficulty with fine motor tasks), or is accompanied by weakness, severe pain, or vision changes. Never stop Ozempic without medical advice.
Can vitamin B12 deficiency cause tingling in people taking Ozempic?
Yes, vitamin B12 deficiency is a well-recognised cause of peripheral neuropathy and tingling. This is particularly relevant for people with diabetes taking metformin long-term, as the MHRA advises that metformin can reduce B12 levels.
The health-related content published on this site is based on credible scientific sources and is periodically reviewed to ensure accuracy and relevance. Although we aim to reflect the most current medical knowledge, the material is meant for general education and awareness only.
The information on this site is not a substitute for professional medical advice. For any health concerns, please speak with a qualified medical professional. By using this information, you acknowledge responsibility for any decisions made and understand we are not liable for any consequences that may result.
Heading 1
Heading 2
Heading 3
Heading 4
Heading 5
Heading 6
Lorem ipsum dolor sit amet, consectetur adipiscing elit, sed do eiusmod tempor incididunt ut labore et dolore magna aliqua. Ut enim ad minim veniam, quis nostrud exercitation ullamco laboris nisi ut aliquip ex ea commodo consequat. Duis aute irure dolor in reprehenderit in voluptate velit esse cillum dolore eu fugiat nulla pariatur.
Block quote
Ordered list
- Item 1
- Item 2
- Item 3
Unordered list
- Item A
- Item B
- Item C
Bold text
Emphasis
Superscript
Subscript