Many women with polycystic ovary syndrome (PCOS) struggle with weight management due to insulin resistance and hormonal imbalances. Weight loss injections, particularly GLP-1 receptor agonists such as semaglutide (Wegovy) and liraglutide (Saxenda), are available in the UK for weight management and may be prescribed to women with PCOS who meet specific eligibility criteria. Whilst not licensed specifically for PCOS treatment, these medications can support weight loss and improve metabolic health when combined with lifestyle modifications. Access through the NHS depends on BMI thresholds, previous weight loss attempts, and referral to specialist weight management services. Understanding the options, evidence, and eligibility requirements is essential for informed decision-making.
Summary: Women with PCOS can access weight loss injections such as semaglutide (Wegovy) or liraglutide (Saxenda) if they meet NHS eligibility criteria based on BMI and weight-related comorbidities, though these medications are not specifically licensed for PCOS treatment.
- GLP-1 receptor agonists work by reducing appetite, slowing gastric emptying, and improving insulin sensitivity, addressing metabolic abnormalities common in PCOS.
- NHS eligibility typically requires BMI ≥35 kg/m² (or ≥30 kg/m² with comorbidities), referral to specialist weight management services, and documented previous weight loss attempts.
- Clinical evidence shows GLP-1 medications can improve weight, menstrual regularity, androgen levels, and insulin resistance in women with PCOS when combined with lifestyle changes.
- Common side effects include nausea, vomiting, diarrhoea, and constipation; effective contraception is recommended during treatment, with discontinuation required at least two months before planned pregnancy.
- Alternative options include metformin, orlistat, structured lifestyle programmes, and bariatric surgery for those meeting specific criteria or unable to access injectable medications.
Table of Contents
- Understanding PCOS and Weight Management Challenges
- Weight Loss Injections Available in the UK for PCOS
- How GLP-1 Medications Work for PCOS-Related Weight Loss
- NHS Eligibility and Prescription Criteria for PCOS Patients
- Effectiveness and Clinical Evidence for PCOS Treatment
- Alternative Weight Management Options for PCOS
- Frequently Asked Questions
Understanding PCOS and Weight Management Challenges
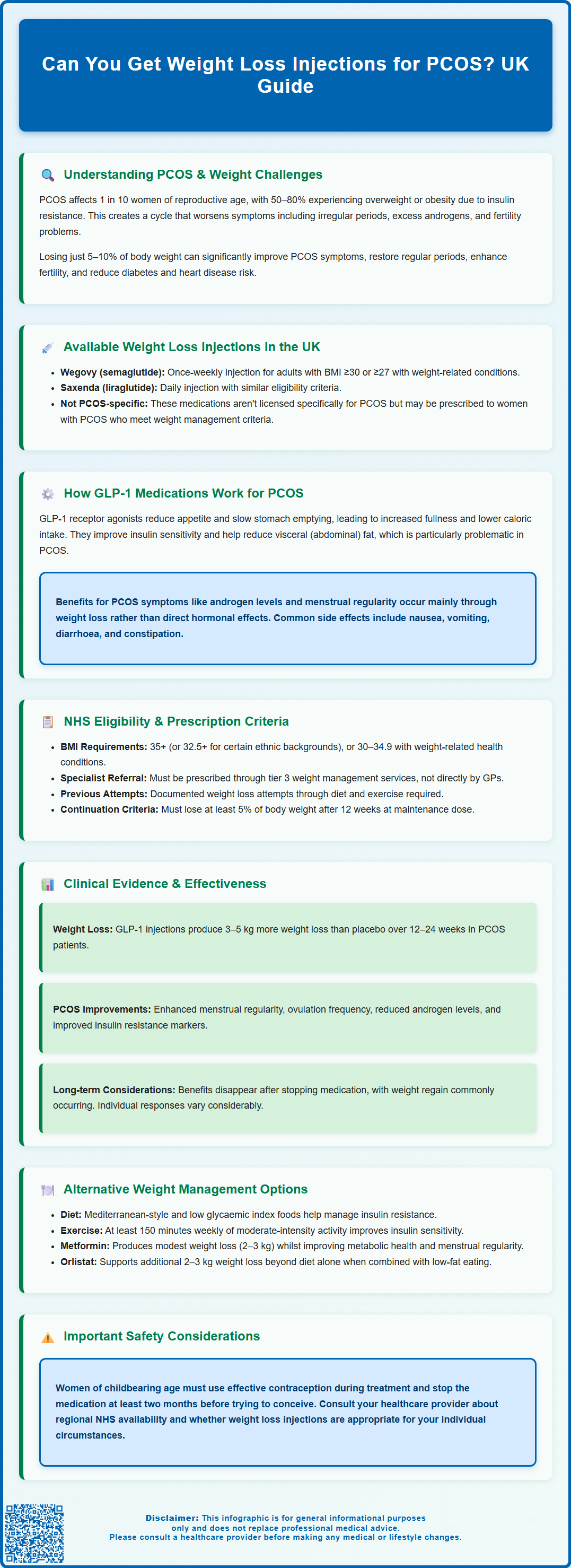
Polycystic ovary syndrome (PCOS) is a common endocrine disorder affecting approximately 1 in 10 women of reproductive age in the UK. The condition is characterised by hormonal imbalances, irregular menstrual cycles, and often (though not always) the presence of ovarian cysts. PCOS is diagnosed using the Rotterdam criteria, which require at least two of three features: irregular periods, elevated androgens, and polycystic ovaries on ultrasound.
One of the most challenging aspects of PCOS is its strong association with weight management difficulties, with an estimated 50–80% of women with PCOS experiencing overweight or obesity.
The relationship between PCOS and weight is complex and bidirectional. Many women with PCOS develop insulin resistance, a condition where the body's cells become less responsive to insulin, leading to elevated blood glucose and insulin levels. This metabolic dysfunction makes weight loss significantly more difficult and contributes to increased fat storage, particularly around the abdomen. Additionally, insulin resistance can worsen other PCOS symptoms, including irregular periods, excess androgen production, and fertility challenges.
Weight management is particularly important for women with PCOS because even modest weight loss of 5–10% of body weight can lead to substantial improvements in symptoms. Research demonstrates that weight reduction can help restore regular menstrual cycles, improve fertility outcomes, reduce androgen levels, and lower the risk of developing type 2 diabetes and cardiovascular disease. However, the metabolic challenges inherent to PCOS often make achieving and maintaining weight loss through diet and exercise alone extremely difficult.
For many women with PCOS, traditional weight loss approaches may prove insufficient, leading to frustration and a search for additional therapeutic options. This has prompted increased interest in pharmacological interventions, including weight loss injections, as potential adjuncts to lifestyle modifications for managing PCOS-related weight challenges.
Weight Loss Injections Available in the UK for PCOS
Several injectable medications originally developed for type 2 diabetes management have gained recognition for their weight loss effects and potential benefits in PCOS. The primary class of weight loss injections available in the UK belongs to the glucagon-like peptide-1 (GLP-1) receptor agonist family. The medications licensed specifically for weight management in the UK include semaglutide (marketed as Wegovy) and liraglutide (Saxenda).
Wegovy (semaglutide 2.4mg) is licensed by the MHRA for chronic weight management in adults with a BMI of 30 kg/m² or greater, or 27 kg/m² or greater with at least one weight-related comorbidity. Liraglutide (Saxenda) is similarly approved for weight management under comparable criteria. These medications are administered via subcutaneous injection, typically once weekly for semaglutide or once daily for liraglutide.
It is important to note that Ozempic (semaglutide at lower doses) and Victoza (liraglutide at lower doses) are licensed only for type 2 diabetes treatment, not weight management. Similarly, dulaglutide (Trulicity) is licensed only for type 2 diabetes and is not approved for weight management in the UK.
Whilst these medications are not specifically licensed for PCOS treatment, they may be prescribed for women with PCOS who meet the weight management criteria. The decision to prescribe these medications considers multiple factors, including BMI, presence of insulin resistance or prediabetes, previous weight loss attempts, and overall metabolic health. These injections are intended as adjuncts to, not replacements for, comprehensive lifestyle modifications including dietary changes and increased physical activity.
Women of childbearing age should be aware that effective contraception is recommended during treatment with GLP-1 receptor agonists, and the medications should be discontinued at least two months before a planned pregnancy. Common side effects include nausea, vomiting, diarrhoea and constipation, which are typically mild to moderate and tend to decrease over time.
Another medication sometimes considered is metformin, though this is typically administered orally rather than by injection. Metformin is commonly prescribed off-label for PCOS to address insulin resistance, and whilst it may support modest weight loss, it is not classified as a weight loss injection.
How GLP-1 Medications Work for PCOS-Related Weight Loss
GLP-1 receptor agonists work through multiple complementary mechanisms that address several metabolic abnormalities present in PCOS. GLP-1 is a naturally occurring incretin hormone released by the intestines in response to food intake. These medications mimic this hormone, binding to GLP-1 receptors throughout the body, particularly in the pancreas, brain, and gastrointestinal tract.
The primary mechanism involves appetite regulation through actions on the hypothalamus and brainstem regions that control satiety and hunger. By activating GLP-1 receptors in these areas, the medications increase feelings of fullness and reduce appetite, leading to decreased caloric intake. Additionally, GLP-1 agonists slow gastric emptying, meaning food remains in the stomach longer, which prolongs satiety after meals and reduces the frequency of hunger signals.
For women with PCOS, the insulin-sensitising effects of GLP-1 medications are particularly relevant. These drugs enhance glucose-dependent insulin secretion from pancreatic beta cells, meaning they stimulate insulin release only when blood glucose levels are elevated. This helps improve glycaemic control without causing hypoglycaemia. Furthermore, they reduce glucagon secretion, a hormone that raises blood glucose levels, thereby contributing to better overall glucose homeostasis.
The metabolic improvements extend beyond weight loss. Studies suggest that GLP-1 receptor agonists may help reduce visceral adiposity (abdominal fat), which is particularly problematic in PCOS and strongly associated with insulin resistance and cardiovascular risk. Some research indicates potential benefits on androgen levels and menstrual regularity, though these effects appear to be largely mediated through weight loss rather than direct hormonal action.
Common side effects include nausea, vomiting, diarrhoea and constipation. More serious but less common side effects include pancreatitis (persistent severe abdominal pain that may radiate to the back), gallbladder problems, and risk of dehydration that could affect kidney function. Patients should seek medical advice if they experience severe or persistent symptoms.
Whilst these medications have shown cardiovascular benefits in people with diabetes and obesity, it's important to note that the evidence base specifically for PCOS treatment continues to evolve, and long-term outcomes in PCOS populations are still being studied.
NHS Eligibility and Prescription Criteria for PCOS Patients
Access to weight loss injections through the NHS is governed by strict eligibility criteria established by NICE and local integrated care boards (ICBs). For women with PCOS seeking these medications, the primary consideration is whether they meet the general weight management criteria rather than having PCOS specifically, as these medications are not currently licensed solely for PCOS treatment.
According to NICE Technology Appraisal guidance (TA875 for semaglutide and TA664 for liraglutide), these medications may be considered for adults with a BMI of 35 kg/m² or greater (or 32.5 kg/m² or greater for people from South Asian, Chinese, other Asian, Middle Eastern, Black African or African-Caribbean family backgrounds) who have been referred to specialist weight management services (tier 3). For those with a BMI of 30–34.9 kg/m² (adjusted thresholds for certain ethnic groups), consideration may be given if they have weight-related comorbidities.
Important NHS prescribing conditions include:
-
Treatment must be initiated and supervised by a specialist weight management service
-
Treatment should only continue if at least 5% of total body weight is lost after 12 weeks at the maintenance dose
-
For semaglutide (Wegovy), treatment should not continue for longer than 2 years
-
Documented evidence of previous weight loss attempts through diet and exercise
-
Engagement with a structured weight management programme
-
Commitment to ongoing lifestyle modifications
Women with PCOS who have developed type 2 diabetes may be eligible for GLP-1 medications through diabetes treatment pathways, which have separate prescribing criteria. The presence of insulin resistance, prediabetes, or metabolic syndrome—all common in PCOS—may strengthen the case for prescription, but does not guarantee access.
NHS availability of these medications varies by region due to commissioning decisions and supply considerations. Some ICBs have implemented additional local criteria or temporary restrictions. Women interested in these treatments should discuss options with their GP, who can provide guidance on local availability, referral pathways to specialist services, and alternative approaches. For those considering private treatment, costs typically vary and should be discussed with the provider, along with ongoing monitoring requirements.
Effectiveness and Clinical Evidence for PCOS Treatment
The evidence base for GLP-1 receptor agonists in PCOS is growing but remains less extensive than for general weight management or diabetes treatment. Clinical trials specifically examining these medications in PCOS populations have shown promising results, though most studies have been relatively small and of short to moderate duration.
Systematic reviews examining GLP-1 agonists in PCOS have found that these medications led to significant weight reduction, with average weight loss ranging from 3–5 kg more than placebo over 12–24 weeks. More importantly, studies demonstrated improvements in several PCOS-related outcomes beyond weight loss. Women treated with GLP-1 agonists showed improvements in menstrual regularity, with increased frequency of ovulation and more regular cycles. Some studies reported reductions in androgen levels (testosterone and androstenedione) and improvements in markers of insulin resistance.
Liraglutide has been studied most extensively in PCOS populations. Research published in the Journal of Clinical Endocrinology & Metabolism demonstrated that liraglutide 3.0 mg daily, combined with lifestyle intervention, resulted in greater weight loss and improved metabolic parameters compared to lifestyle intervention alone. Participants experienced improvements in insulin sensitivity, lipid profiles, and blood pressure.
Semaglutide has shown superior weight loss efficacy in general obesity populations (with average weight loss of 10–15% of body weight in major trials). However, there are fewer specific studies in PCOS cohorts. While its mechanism of action suggests potential benefits for women with PCOS, it's important to note that extrapolation from general obesity data has limitations, and PCOS-specific outcomes may differ.
Important considerations include:
-
Individual response varies considerably—not all women will achieve the same degree of weight loss or symptom improvement
-
Benefits appear to be maintained only whilst taking the medication; weight regain commonly occurs after discontinuation
-
Most evidence comes from studies of 6–12 months duration; long-term safety and efficacy data in PCOS populations remain limited
-
The medications address weight and metabolic aspects of PCOS but may not resolve all symptoms, particularly in women without significant weight loss
Women considering these treatments should have realistic expectations and understand that these medications work best as part of a comprehensive management plan including dietary modification, regular physical activity, and management of other PCOS symptoms. Any suspected side effects should be reported to healthcare professionals or through the MHRA Yellow Card scheme.
Alternative Weight Management Options for PCOS
For women with PCOS who do not have access to or are not suitable candidates for weight loss injections, numerous evidence-based alternatives exist. A comprehensive, multifaceted approach often yields the best outcomes for managing PCOS-related weight challenges.
Lifestyle modifications remain the cornerstone of PCOS management. NICE recommends that all women with PCOS receive information about lifestyle management, including diet and exercise. A Mediterranean-style diet—rich in vegetables, fruits, whole grains, legumes, nuts, and olive oil, with moderate fish and poultry—has shown particular promise for PCOS. Some evidence suggests that low glycaemic index (GI) diets may help manage insulin resistance and support weight loss. Reducing refined carbohydrates and added sugars whilst ensuring adequate protein intake can help stabilise blood glucose and reduce insulin spikes.
Regular physical activity is crucial, with current recommendations suggesting at least 150 minutes of moderate-intensity exercise weekly. Both aerobic exercise and resistance training offer benefits; resistance training may be particularly valuable for improving insulin sensitivity and body composition.
Metformin remains a widely used pharmacological option for PCOS, particularly for women with insulin resistance or impaired glucose tolerance. Whilst typically producing modest weight loss (2–3 kg on average), metformin can improve metabolic parameters, restore menstrual regularity, and reduce diabetes risk. It is generally well-tolerated, though gastrointestinal side effects are common initially. Long-term use requires monitoring, including vitamin B12 levels, as deficiency can occur.
Orlistat, a lipase inhibitor that reduces dietary fat absorption, is available both on prescription and over-the-counter (as Alli in lower doses). It may support weight loss of approximately 2–3 kg beyond diet alone but requires adherence to a low-fat diet to minimise gastrointestinal side effects. Treatment should be reviewed after 12 weeks and discontinued if less than 5% of body weight has been lost.
Behavioural interventions including cognitive behavioural therapy (CBT), mindful eating approaches, and structured weight management programmes can address psychological aspects of eating and support sustainable lifestyle changes. Many areas offer NHS-funded weight management services, though availability varies by region.
For women with severe obesity (BMI ≥40 kg/m² or ≥35 kg/m² with comorbidities, with lower thresholds for certain ethnic groups and those with recent-onset type 2 diabetes) who have not achieved adequate weight loss through other means, bariatric surgery may be considered. Procedures such as gastric bypass or sleeve gastrectomy can produce substantial, sustained weight loss and dramatic improvements in PCOS symptoms, insulin resistance, and fertility outcomes.
Women with PCOS should work with their healthcare team—potentially including GPs, endocrinologists, dietitians, and fertility specialists—to develop an individualised management plan that addresses their specific symptoms, goals, and circumstances.
Frequently Asked Questions
Are weight loss injections specifically approved for PCOS treatment in the UK?
No, weight loss injections such as semaglutide (Wegovy) and liraglutide (Saxenda) are not specifically licensed for PCOS treatment but may be prescribed to women with PCOS who meet general weight management eligibility criteria based on BMI and comorbidities.
How much weight can women with PCOS expect to lose with GLP-1 injections?
Clinical studies in PCOS populations show variable individual responses, with research demonstrating improvements in weight, metabolic parameters, and PCOS symptoms when combined with lifestyle modifications. NHS treatment continues only if at least 5% of total body weight is lost after 12 weeks at the maintenance dose.
What happens if I don't meet NHS criteria for weight loss injections for PCOS?
Alternative evidence-based options include metformin for insulin resistance, orlistat, structured lifestyle programmes focusing on diet and exercise, behavioural interventions, and bariatric surgery for those meeting specific criteria. Your GP can discuss suitable alternatives based on your individual circumstances.
The health-related content published on this site is based on credible scientific sources and is periodically reviewed to ensure accuracy and relevance. Although we aim to reflect the most current medical knowledge, the material is meant for general education and awareness only.
The information on this site is not a substitute for professional medical advice. For any health concerns, please speak with a qualified medical professional. By using this information, you acknowledge responsibility for any decisions made and understand we are not liable for any consequences that may result.
Heading 1
Heading 2
Heading 3
Heading 4
Heading 5
Heading 6
Lorem ipsum dolor sit amet, consectetur adipiscing elit, sed do eiusmod tempor incididunt ut labore et dolore magna aliqua. Ut enim ad minim veniam, quis nostrud exercitation ullamco laboris nisi ut aliquip ex ea commodo consequat. Duis aute irure dolor in reprehenderit in voluptate velit esse cillum dolore eu fugiat nulla pariatur.
Block quote
Ordered list
- Item 1
- Item 2
- Item 3
Unordered list
- Item A
- Item B
- Item C
Bold text
Emphasis
Superscript
Subscript