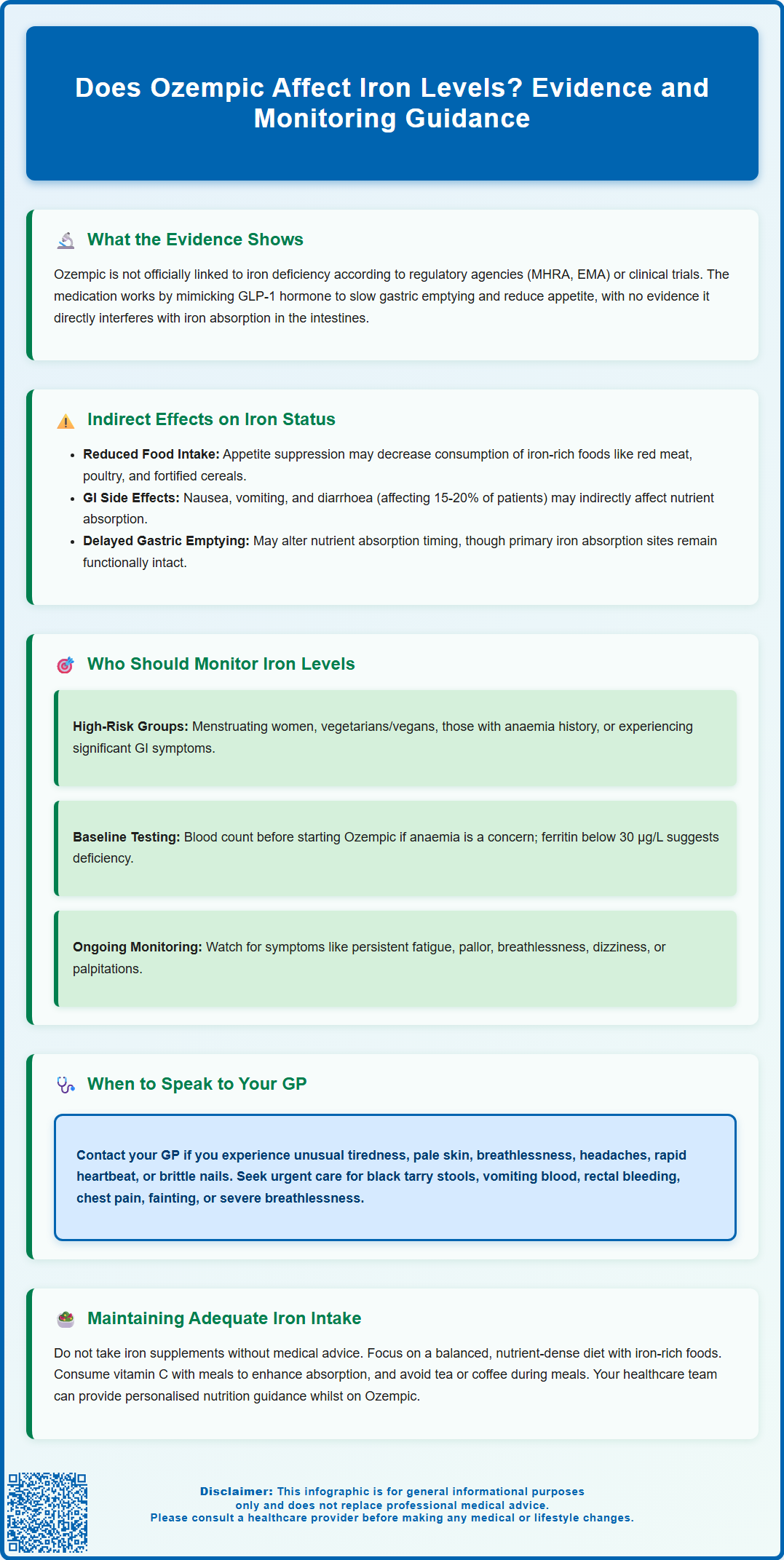
Does Ozempic affect iron levels? This is a common question amongst patients prescribed semaglutide for type 2 diabetes. Ozempic (semaglutide) is a GLP-1 receptor agonist licensed in the UK for glycaemic control. Whilst there is no established direct link between Ozempic and iron deficiency according to the MHRA or clinical trials, the medication's gastrointestinal effects—including nausea, vomiting, and appetite suppression—may indirectly influence nutritional intake. Understanding the relationship between Ozempic and iron status helps patients and healthcare professionals monitor nutritional adequacy during treatment, particularly in those with pre-existing risk factors for iron deficiency.
Summary: Ozempic does not directly affect iron levels, but its gastrointestinal side effects may indirectly influence nutritional intake and iron status in susceptible individuals.
- Ozempic (semaglutide) is a GLP-1 receptor agonist licensed in the UK for type 2 diabetes, not weight management.
- Iron deficiency is not listed as a recognised adverse effect by the MHRA or in the Summary of Product Characteristics.
- Gastrointestinal effects such as nausea, vomiting, and appetite suppression may reduce dietary iron intake indirectly.
- Routine iron monitoring is not required, but targeted testing may be appropriate for high-risk groups including menstruating women and vegetarians.
- Patients experiencing persistent fatigue, pallor, or breathlessness should seek medical review for possible iron deficiency anaemia.
Table of Contents
Does Ozempic Affect Iron Levels?
Ozempic (semaglutide) is a glucagon-like peptide-1 (GLP-1) receptor agonist licensed in the UK for the treatment of type 2 diabetes mellitus. A higher dose formulation of semaglutide (Wegovy) is licensed for weight management, but Ozempic itself is not approved for this purpose. Whilst Ozempic has demonstrated significant efficacy in glycaemic control and modest weight reduction, patients and healthcare professionals often enquire about its potential effects on micronutrient status, including iron levels.
Currently, there is no established link between Ozempic and iron deficiency according to the Summary of Product Characteristics (SmPC) or major clinical trials. The Medicines and Healthcare products Regulatory Agency (MHRA) and the European Medicines Agency (EMA) do not list iron deficiency or anaemia as recognised adverse effects of semaglutide. However, the gastrointestinal effects of Ozempic—particularly nausea, vomiting, and diarrhoea—may indirectly influence nutritional intake and absorption, which could theoretically affect iron status in susceptible individuals.
It is important to distinguish between a direct pharmacological effect on iron metabolism and indirect consequences of treatment. Ozempic works by mimicking the incretin hormone GLP-1, which slows gastric emptying, enhances insulin secretion, and reduces appetite. There is currently no evidence that these mechanisms directly interfere with iron absorption pathways in the duodenum and proximal jejunum. Nonetheless, patients experiencing significant gastrointestinal side effects or substantial dietary changes may be at risk of suboptimal nutrient intake, including iron. Individuals with pre-existing risk factors for iron deficiency—such as menstruating women, vegetarians, or those with a history of anaemia—should be particularly mindful of maintaining adequate dietary iron whilst taking Ozempic.
Potential Effects of Ozempic on Nutrient Absorption
Whilst Ozempic does not appear to directly impair iron absorption, its gastrointestinal effects may indirectly influence nutritional status. The most commonly reported adverse effects of Ozempic include nausea (occurring in approximately 15-20% of patients according to the SmPC), vomiting, diarrhoea, constipation, and abdominal discomfort. These symptoms are typically most pronounced during dose titration and often improve with continued treatment.
Delayed gastric emptying, a key mechanism of Ozempic's action, may alter the timing of nutrient absorption, though this effect may attenuate with continued treatment. The Ozempic SmPC notes that despite this effect, there is no clinically relevant impact on the absorption of most orally administered medications. The duodenum and proximal jejunum—the primary sites of iron absorption—remain functionally intact during semaglutide therapy.
The more significant concern relates to reduced dietary intake. Patients taking Ozempic often experience appetite suppression and early satiety, which can lead to lower caloric consumption. If dietary variety and quality are compromised, intake of iron-rich foods (such as red meat, poultry, fish, pulses, and fortified cereals) may decline. This is particularly relevant for individuals following restrictive diets or those who develop food aversions due to nausea.
Weight loss associated with Ozempic for type 2 diabetes is typically modest compared to the higher doses used in Wegovy for weight management. However, even moderate weight loss should be managed with attention to nutritional adequacy. NICE guidance on obesity management (CG189) emphasises the importance of nutritional adequacy during pharmacological weight loss interventions. Healthcare professionals should encourage patients to maintain a balanced, nutrient-dense diet and consider whether supplementation may be appropriate in high-risk groups.
Monitoring Iron Levels While Taking Ozempic
Routine monitoring of iron levels is not specifically required for all patients taking Ozempic, as iron deficiency is not a recognised adverse effect of the medication. However, targeted monitoring may be appropriate for individuals with risk factors for iron deficiency or those experiencing symptoms suggestive of anaemia.
Patients who may benefit from iron level monitoring include:
-
Women of childbearing age, particularly those with heavy menstrual bleeding
-
Individuals following vegetarian or vegan diets
-
Patients with a history of iron deficiency anaemia
-
Those experiencing significant gastrointestinal symptoms or dietary restriction
-
Individuals with malabsorptive conditions (e.g., coeliac disease, inflammatory bowel disease)
-
Patients undergoing rapid or substantial weight loss
Baseline assessment before initiating Ozempic should include a full blood count (FBC) if there are pre-existing concerns about anaemia. If iron deficiency is suspected during treatment, appropriate investigations include FBC, serum ferritin, transferrin saturation (TSAT), and total iron-binding capacity. In the UK, a ferritin level below 30 µg/L generally suggests iron deficiency in uncomplicated cases, though higher thresholds (with TSAT <20%) may be considered in patients with inflammatory conditions.
Symptoms that may warrant investigation include persistent fatigue, pallor, breathlessness on exertion, dizziness, palpitations, or restless legs syndrome. It is important to note that these symptoms are non-specific and may have multiple causes, including the underlying diabetes, other medications, or concurrent medical conditions.
Healthcare professionals should maintain a low threshold for investigating unexplained anaemia in patients taking Ozempic. According to British Society of Gastroenterology (BSG) guidelines, adult men and postmenopausal women with confirmed iron deficiency anaemia generally warrant gastrointestinal investigation. Adults aged 60 or over with iron deficiency anaemia meet NICE criteria (NG12) for urgent suspected cancer referral. Testing for coeliac disease is also recommended in all patients with iron deficiency anaemia.
When to Speak to Your GP About Iron Deficiency
Patients taking Ozempic should contact their GP if they develop symptoms that may indicate iron deficiency or anaemia. Early recognition and management of iron deficiency can prevent progression to more severe anaemia and its associated complications.
Key symptoms that warrant medical review include:
-
Unusual tiredness or weakness that interferes with daily activities
-
Noticeable pallor of the skin, inner eyelids, or nail beds
-
Breathlessness during normal activities or mild exertion
-
Persistent headaches or difficulty concentrating
-
Rapid or irregular heartbeat (palpitations)
-
Sore or unusually smooth tongue
-
Brittle nails or hair loss
-
Unusual cravings for non-food items (pica)
Seek urgent medical attention if you experience black tarry stools, vomiting blood, rectal bleeding, chest pain, fainting, or severe breathlessness, as these may indicate serious conditions requiring immediate assessment.
It is particularly important to seek medical advice if you are experiencing persistent gastrointestinal side effects from Ozempic that are affecting your ability to maintain a balanced diet, or if you have lost a significant amount of weight rapidly. Your GP can assess whether your symptoms are related to iron deficiency, your diabetes medication, or another underlying cause.
Do not self-prescribe iron supplements without medical advice, as excessive iron intake can cause side effects and may mask other important diagnoses. If iron deficiency is confirmed, your GP will recommend appropriate treatment, which typically involves oral iron supplementation (such as ferrous sulphate or ferrous fumarate) and dietary advice. In cases of severe deficiency or intolerance to oral iron, intravenous iron therapy may be considered.
Your healthcare team can provide personalised nutritional guidance to help you maintain adequate iron intake whilst taking Ozempic. This may include advice on iron-rich foods, strategies to enhance iron absorption (such as consuming vitamin C with meals), and avoiding substances that inhibit absorption (such as tea or coffee with meals). Regular follow-up ensures that any nutritional concerns are addressed promptly, allowing you to benefit from Ozempic treatment whilst maintaining optimal health.
If you suspect you are experiencing side effects from Ozempic, you can report these through the MHRA Yellow Card scheme, which helps monitor the safety of medicines in the UK.
Frequently Asked Questions
Can Ozempic cause iron deficiency anaemia?
Ozempic does not directly cause iron deficiency anaemia. However, gastrointestinal side effects such as nausea and reduced appetite may indirectly affect dietary iron intake, particularly in individuals with pre-existing risk factors.
Do I need to have my iron levels checked whilst taking Ozempic?
Routine iron monitoring is not required for all patients taking Ozempic. However, targeted testing may be appropriate if you have risk factors for iron deficiency, experience symptoms of anaemia, or have significant gastrointestinal side effects affecting your diet.
What symptoms suggest I might have low iron levels whilst on Ozempic?
Symptoms of iron deficiency include unusual tiredness, pallor, breathlessness on exertion, headaches, palpitations, and difficulty concentrating. If you experience these symptoms whilst taking Ozempic, contact your GP for assessment and appropriate blood tests.
The health-related content published on this site is based on credible scientific sources and is periodically reviewed to ensure accuracy and relevance. Although we aim to reflect the most current medical knowledge, the material is meant for general education and awareness only.
The information on this site is not a substitute for professional medical advice. For any health concerns, please speak with a qualified medical professional. By using this information, you acknowledge responsibility for any decisions made and understand we are not liable for any consequences that may result.
Heading 1
Heading 2
Heading 3
Heading 4
Heading 5
Heading 6
Lorem ipsum dolor sit amet, consectetur adipiscing elit, sed do eiusmod tempor incididunt ut labore et dolore magna aliqua. Ut enim ad minim veniam, quis nostrud exercitation ullamco laboris nisi ut aliquip ex ea commodo consequat. Duis aute irure dolor in reprehenderit in voluptate velit esse cillum dolore eu fugiat nulla pariatur.
Block quote
Ordered list
- Item 1
- Item 2
- Item 3
Unordered list
- Item A
- Item B
- Item C
Bold text
Emphasis
Superscript
Subscript