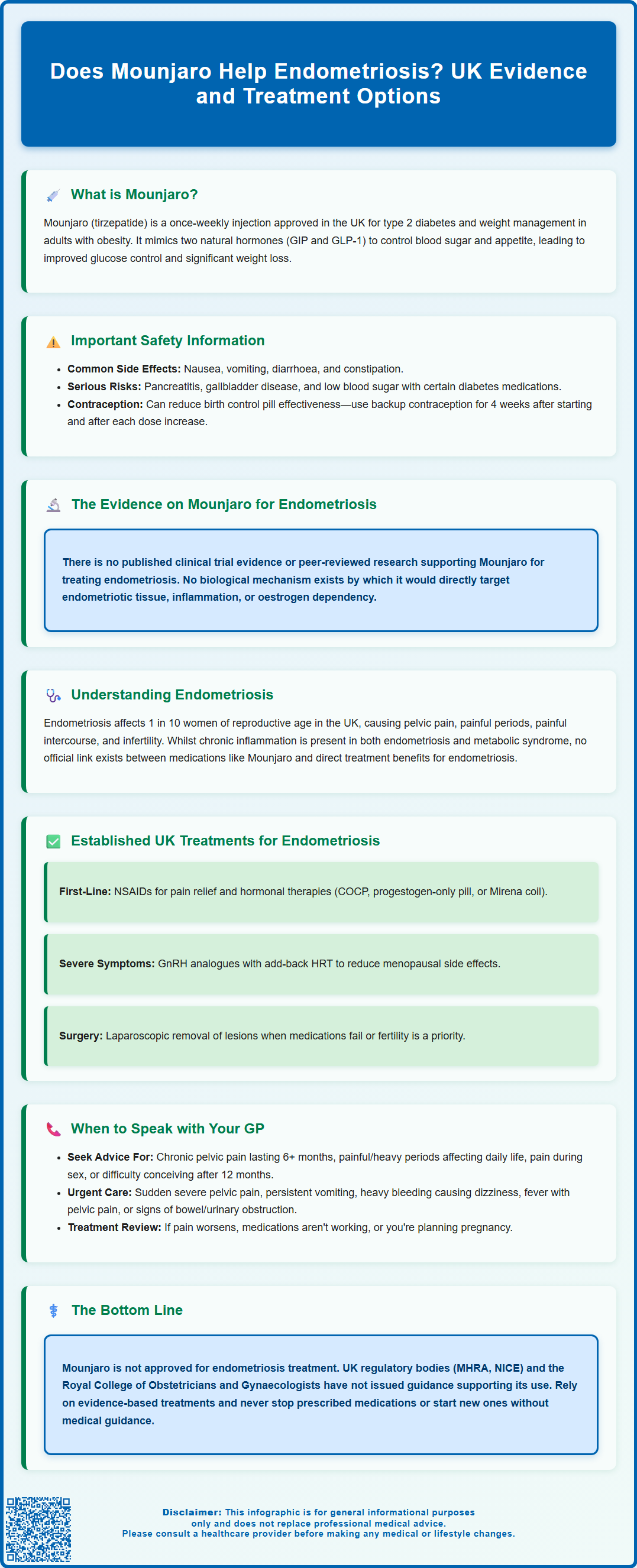
Mounjaro (tirzepatide) is a dual GIP/GLP-1 receptor agonist licensed in the UK for type 2 diabetes and weight management, but does Mounjaro help endometriosis? Currently, there is no clinical evidence supporting its use for endometriosis treatment. Whilst emerging research explores links between metabolic health and endometriosis, Mounjaro is not approved by the MHRA or EMA for this condition. This article examines the current evidence, established endometriosis treatments, and when to seek medical advice for symptom management.
Summary: Mounjaro (tirzepatide) is not approved for endometriosis treatment and no clinical evidence supports its use for this condition.
- Mounjaro is a dual GIP/GLP-1 receptor agonist licensed in the UK only for type 2 diabetes and weight management.
- No published clinical trials or peer-reviewed research have investigated Mounjaro for endometriosis treatment.
- The MHRA, NICE, and RCOG have not issued guidance supporting Mounjaro use for endometriosis.
- Established UK treatments include NSAIDs, hormonal therapies (COCP, progestogens, LNG-IUS), GnRH analogues, and laparoscopic surgery.
- Off-label use carries risks including unforeseen adverse effects and potential interactions with established endometriosis treatments.
- Patients should discuss any novel therapies with their GP or specialist through shared decision-making aligned with NICE guidelines.
Table of Contents
Understanding Mounjaro and Its Primary Use
Mounjaro (tirzepatide) is a prescription medicine licensed in the UK for the treatment of type 2 diabetes mellitus and, more recently, for weight management in adults with obesity or overweight with weight-related comorbidities. It belongs to a novel class of medications known as dual glucose-dependent insulinotropic polypeptide (GIP) and glucagon-like peptide-1 (GLP-1) receptor agonists.
The drug works by mimicking two naturally occurring hormones that regulate blood sugar levels and appetite. By activating both GIP and GLP-1 receptors, Mounjaro enhances insulin secretion when blood glucose is elevated, suppresses glucagon release, slows gastric emptying, and reduces appetite. These combined effects lead to improved glycaemic control in people with type 2 diabetes and significant weight loss in those using it for obesity management.
Mounjaro is administered as a once-weekly subcutaneous injection, with doses gradually increased over time to minimise gastrointestinal side effects. Common adverse effects include nausea, vomiting, diarrhoea, constipation, and reduced appetite. More serious but rare complications can include pancreatitis, gallbladder disease, and hypoglycaemia (primarily when used alongside insulin or sulfonylureas). Severe gastrointestinal side effects may lead to dehydration, so it's important to maintain fluid intake and seek medical advice if unable to keep fluids down.
Important safety information: Mounjaro can reduce the effectiveness of oral contraceptive pills due to delayed gastric emptying. If you use oral contraceptives, you should use additional or alternative contraception for 4 weeks after starting Mounjaro and after each dose increase. The medication is not recommended during pregnancy or breastfeeding, and women of childbearing potential should use effective contraception while taking it.
It is important to note that Mounjaro is not currently licensed or approved by the Medicines and Healthcare products Regulatory Agency (MHRA) or the European Medicines Agency (EMA) for the treatment of endometriosis. Its use remains confined to metabolic conditions, and any application outside these indications would be considered off-label. Patients should always discuss the appropriateness of any medication with their healthcare provider before considering its use for conditions beyond its licensed indications.
The Link Between Weight, Metabolism and Endometriosis
Endometriosis is a chronic inflammatory condition in which tissue similar to the lining of the uterus (endometrium) grows outside the womb, commonly affecting the ovaries, fallopian tubes, and pelvic peritoneum. It affects approximately 1 in 10 women and people assigned female at birth of reproductive age in the UK and is associated with pelvic pain, painful periods (dysmenorrhoea), pain during intercourse (dyspareunia), and infertility.
Emerging research suggests complex relationships between body weight, metabolic health, and endometriosis, though the evidence remains nuanced and limited. Some observational studies indicate that individuals with a lower body mass index (BMI) may have a slightly increased risk of developing endometriosis, whilst obesity appears to have a more variable association. The hormonal environment plays a crucial role: adipose (fat) tissue produces oestrogen, and endometriosis is an oestrogen-dependent condition. However, the relationship is not straightforward, as obesity is also associated with chronic low-grade inflammation, which may influence endometriosis pathophysiology.
Metabolic factors have been observed in some people with endometriosis, though the exact mechanisms and relationships remain unclear. Chronic inflammation—a hallmark of both metabolic syndrome and endometriosis—may create a systemic environment that could potentially influence symptoms, but robust causal links between specific metabolic pathways and endometriosis are not yet established.
Whilst weight management and metabolic optimisation are important aspects of overall health, there is no official link established between medications like Mounjaro and direct therapeutic benefit for endometriosis itself. Any potential effects would likely be indirect, mediated through improvements in metabolic parameters or weight reduction, rather than through a direct action on endometriotic tissue. More research is needed to understand these complex relationships.
Current Evidence on Mounjaro for Endometriosis
At present, there is no published clinical trial evidence or peer-reviewed research specifically investigating the use of Mounjaro (tirzepatide) for the treatment of endometriosis. Searches of clinical trial registries such as ClinicalTrials.gov and the ISRCTN registry confirm that the drug has not been studied in this patient population, and no data exist to support its efficacy, safety, or appropriateness for managing endometriosis symptoms or disease progression.
Whilst GLP-1 receptor agonists (a related class of medications) have been explored in various research contexts—including polycystic ovary syndrome (PCOS), another hormone-related condition—these findings cannot be extrapolated to endometriosis. The pathophysiology of endometriosis is distinct, involving aberrant endometrial-like tissue growth, chronic inflammation, immune dysregulation, and oestrogen dependency. There is no established mechanism by which Mounjaro would directly target or modify these disease processes.
Some patients and online communities have speculated about potential benefits based on the drug's effects on weight loss, insulin sensitivity, and inflammation. However, such hypotheses remain entirely theoretical and unsupported by clinical evidence. It is crucial to distinguish between scientifically validated treatments and anecdotal reports or conjecture.
The MHRA, NICE, and professional bodies such as the Royal College of Obstetricians and Gynaecologists (RCOG) have not issued guidance supporting the use of Mounjaro for endometriosis. Off-label prescribing of medications carries inherent risks, including unforeseen adverse effects, lack of efficacy, and potential interactions with established endometriosis treatments. Off-label use outside of properly designed clinical trials is not recommended.
Patients considering any novel or off-label therapy should engage in shared decision-making with their GP or specialist. Evidence-based treatments remain the cornerstone of safe and effective endometriosis management, and experimental approaches should only be considered within the context of properly designed clinical trials with appropriate ethical oversight.
Established Treatments for Endometriosis in the UK
The management of endometriosis in the UK follows NICE guidelines (NG73), which recommend a stepwise, individualised approach based on symptom severity, fertility considerations, and patient preferences. Treatment aims to reduce pain, improve quality of life, and preserve fertility where desired. Importantly, NICE guidance allows for empirical treatment to be started based on clinical suspicion, even before a definitive diagnosis is made.
First-line pharmacological management typically involves:
-
Analgesia: Paracetamol and non-steroidal anti-inflammatory drugs (NSAIDs) such as ibuprofen or mefenamic acid for pain relief
-
Hormonal therapies: Combined oral contraceptive pill (COCP), progestogen-only pill, or the levonorgestrel intrauterine system (LNG-IUS/Mirena coil) to suppress endometrial tissue growth and reduce menstrual flow
-
GnRH analogues: Gonadotrophin-releasing hormone agonists (e.g., goserelin) may be used for more severe symptoms, often with add-back hormone replacement therapy (HRT) to mitigate menopausal side effects. GnRH antagonists may also be considered in specialist settings for some patients
Surgical intervention is considered when medical management is insufficient or when fertility is a priority. Laparoscopic excision or ablation of endometriotic lesions can provide symptom relief and improve fertility outcomes. In severe, refractory cases, hysterectomy with or without oophorectomy may be discussed, though this is typically reserved for women who have completed their families.
Multidisciplinary support is essential, particularly for people with deep infiltrating endometriosis affecting the bowel, bladder, or other organs. NICE recommends referral to specialist endometriosis centres for complex cases. Additionally, psychological support, physiotherapy (including pelvic floor therapy), and pain management services play important roles in comprehensive care.
Lifestyle modifications, including regular exercise, a balanced diet, and stress management, may help some individuals manage symptoms, though evidence for specific dietary interventions remains limited. Patients should be empowered to explore these alongside conventional treatments, always under medical supervision.
When to Speak with Your GP About Endometriosis Management
Women and people with endometriosis symptoms should seek medical advice promptly. Key symptoms warranting GP consultation include:
-
Chronic pelvic pain lasting six months or more
-
Painful, heavy, or irregular periods that interfere with daily activities
-
Pain during or after sexual intercourse
-
Pain with bowel movements or urination, particularly during menstruation
-
Difficulty conceiving after 12 months of regular unprotected intercourse (or six months if aged over 35)
Urgent medical attention is needed for:
-
Sudden, severe pelvic pain
-
Persistent vomiting or inability to keep fluids down
-
Heavy bleeding causing dizziness or fainting
-
Fever with pelvic pain
-
Signs of bowel or urinary obstruction
Your GP will take a detailed history, perform an examination if appropriate, and may arrange investigations such as pelvic ultrasound or refer you to gynaecology for further assessment. Definitive diagnosis often requires laparoscopy (keyhole surgery), though treatment may be initiated based on clinical suspicion alone, in line with NICE guidance.
If you are already diagnosed with endometriosis and your current treatment is not adequately controlling symptoms, do not hesitate to request a review. This is particularly important if:
-
Pain is worsening or not responding to prescribed analgesia or hormonal therapy
-
You are experiencing significant side effects from medications
-
You are planning pregnancy and wish to discuss fertility options
-
You have concerns about new or unusual symptoms
Patients with deep infiltrating endometriosis or organ involvement should be referred to a specialist endometriosis centre for comprehensive care.
Patients interested in novel therapies, including medications like Mounjaro, should raise these discussions with their GP or specialist. Your healthcare provider can explain the current evidence base, discuss potential risks and benefits, and help you make informed decisions aligned with established clinical guidelines.
Never discontinue prescribed treatments or start new medications without medical advice. If you experience side effects from any medication, report them via the MHRA Yellow Card scheme at yellowcard.mhra.gov.uk or via the Yellow Card app. Endometriosis management is most effective when delivered through a collaborative, evidence-based approach tailored to your individual circumstances and preferences.
Frequently Asked Questions
Is Mounjaro approved for treating endometriosis in the UK?
No, Mounjaro (tirzepatide) is not approved by the MHRA or EMA for endometriosis treatment. It is licensed only for type 2 diabetes and weight management in adults with obesity or overweight with weight-related comorbidities.
What are the established treatments for endometriosis recommended by NICE?
NICE guidelines recommend a stepwise approach including NSAIDs for pain relief, hormonal therapies (combined oral contraceptive pill, progestogens, or LNG-IUS), GnRH analogues for severe symptoms, and laparoscopic surgery when medical management is insufficient or fertility is a priority.
When should I see my GP about endometriosis symptoms?
Consult your GP if you experience chronic pelvic pain lasting six months or more, painful or heavy periods interfering with daily activities, pain during intercourse, or difficulty conceiving after 12 months of trying. Seek urgent care for sudden severe pelvic pain, persistent vomiting, heavy bleeding causing dizziness, or fever with pelvic pain.
The health-related content published on this site is based on credible scientific sources and is periodically reviewed to ensure accuracy and relevance. Although we aim to reflect the most current medical knowledge, the material is meant for general education and awareness only.
The information on this site is not a substitute for professional medical advice. For any health concerns, please speak with a qualified medical professional. By using this information, you acknowledge responsibility for any decisions made and understand we are not liable for any consequences that may result.
Heading 1
Heading 2
Heading 3
Heading 4
Heading 5
Heading 6
Lorem ipsum dolor sit amet, consectetur adipiscing elit, sed do eiusmod tempor incididunt ut labore et dolore magna aliqua. Ut enim ad minim veniam, quis nostrud exercitation ullamco laboris nisi ut aliquip ex ea commodo consequat. Duis aute irure dolor in reprehenderit in voluptate velit esse cillum dolore eu fugiat nulla pariatur.
Block quote
Ordered list
- Item 1
- Item 2
- Item 3
Unordered list
- Item A
- Item B
- Item C
Bold text
Emphasis
Superscript
Subscript