Mounjaro (tirzepatide) and testosterone replacement therapy are increasingly prescribed to men with type 2 diabetes and hypogonadism, respectively. As these conditions frequently coexist in middle-aged and older populations, understanding potential interactions between these medications is essential for safe prescribing. Whilst no direct pharmacokinetic interactions are documented, indirect metabolic effects warrant careful consideration. This article examines the evidence regarding Mounjaro and testosterone interactions, providing practical guidance on concurrent use, monitoring requirements, and safety considerations for UK clinicians managing patients receiving both treatments.
Summary: No direct drug interaction exists between Mounjaro (tirzepatide) and testosterone, but indirect metabolic effects require careful monitoring when used concurrently.
- Tirzepatide is a dual GIP/GLP-1 receptor agonist for type 2 diabetes; testosterone treats clinically confirmed hypogonadism
- No documented pharmacokinetic or pharmacodynamic interaction exists between these medications
- Weight loss from tirzepatide may improve testosterone levels in obesity-related functional hypogonadism
- Concurrent use requires monitoring of glycaemic control, testosterone levels, haematocrit, and cardiovascular risk factors
- Both medications independently affect metabolic parameters and cardiovascular health through different mechanisms
Table of Contents
Understanding Mounjaro (Tirzepatide) and Testosterone Therapy
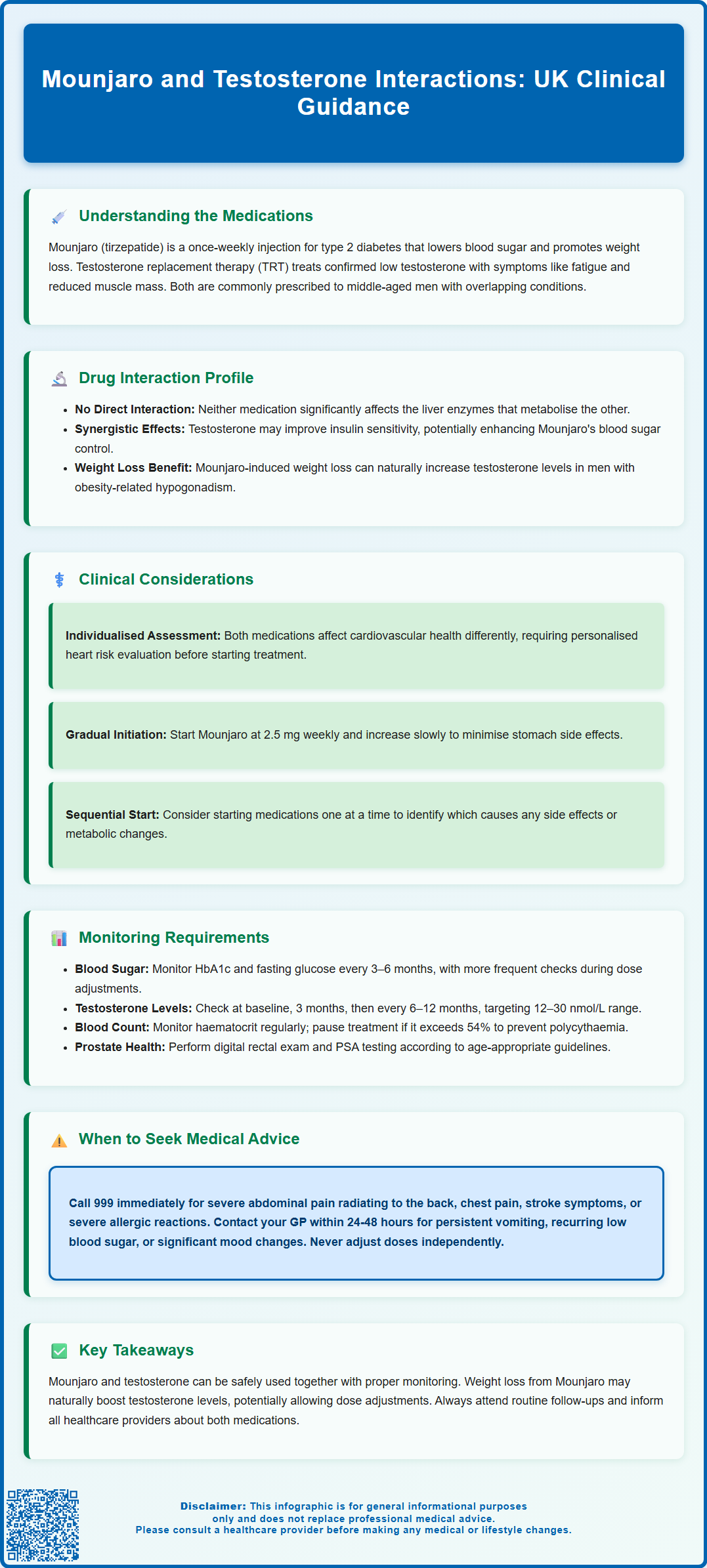
Mounjaro (tirzepatide) is a dual glucose-dependent insulinotropic polypeptide (GIP) and glucagon-like peptide-1 (GLP-1) receptor agonist licensed in the UK for the treatment of type 2 diabetes mellitus. Administered as a once-weekly subcutaneous injection, tirzepatide works by enhancing insulin secretion in response to elevated blood glucose levels, suppressing glucagon release, slowing gastric emptying, and reducing appetite. Clinical trials have shown improvements in glycaemic control and weight reduction in patients with type 2 diabetes, particularly those with obesity.
Testosterone replacement therapy (TRT) is prescribed to men with clinically confirmed hypogonadism—a condition characterised by low testosterone levels accompanied by relevant symptoms such as reduced libido, erectile dysfunction, fatigue, decreased muscle mass, and mood disturbances. Diagnosis requires confirmation of low morning total testosterone on two separate occasions, along with assessment of luteinising hormone (LH), follicle-stimulating hormone (FSH), and prolactin, plus evaluation of reversible causes such as obesity, obstructive sleep apnoea, and opioid use. In the UK, testosterone is commonly available as intramuscular injections and transdermal gels, with patches and oral preparations having limited availability. Importantly, testosterone therapy suppresses spermatogenesis and should be avoided in men seeking fertility, who may require alternative treatments such as gonadotrophins.
As both Mounjaro and testosterone therapy are commonly prescribed to middle-aged and older men—populations that frequently present with metabolic syndrome, type 2 diabetes, and hypogonadism—questions naturally arise regarding potential interactions between these medications. Understanding the pharmacological profiles of both treatments is essential for clinicians managing patients who may require concurrent therapy. Whilst each medication has distinct mechanisms of action, their combined use necessitates careful consideration of metabolic effects, monitoring requirements, and patient-specific factors to ensure safe and effective treatment outcomes.
Known Drug Interactions Between Mounjaro and Testosterone
Currently, there is no official pharmacokinetic or pharmacodynamic interaction documented between tirzepatide and testosterone in the Summary of Product Characteristics (SmPC) for Mounjaro or in guidance from the Medicines and Healthcare products Regulatory Agency (MHRA). Neither medication is known to significantly affect the hepatic cytochrome P450 enzyme system in ways that would alter the metabolism of the other. Tirzepatide is metabolised primarily through proteolytic cleavage, whilst testosterone undergoes hepatic metabolism via various pathways including reduction and conjugation.
However, indirect metabolic interactions warrant consideration. Testosterone therapy can influence body composition by increasing lean muscle mass and potentially affecting insulin sensitivity. Some studies suggest testosterone replacement may improve insulin sensitivity in hypogonadal men with type 2 diabetes, though evidence is mixed and population-specific. This could theoretically enhance the glucose-lowering effects of tirzepatide. Conversely, weight loss associated with Mounjaro may influence endogenous testosterone production, as obesity is associated with lower testosterone levels through increased aromatase activity in adipose tissue.
Gastrointestinal effects of tirzepatide—including nausea, vomiting, and delayed gastric emptying—could theoretically affect the absorption of oral medications. The Mounjaro SmPC specifically cautions that tirzepatide can delay absorption of oral medicines requiring rapid gastrointestinal absorption, such as oral contraceptives. This is less relevant for injectable or transdermal testosterone formulations commonly used in UK practice.
It is worth noting that testosterone may enhance the anticoagulant effect of warfarin and other coumarin anticoagulants, requiring INR monitoring if these medications are used concurrently.
Importantly, both medications can independently affect cardiovascular risk factors, lipid profiles, and body composition, necessitating comprehensive monitoring when used together. Clinicians should remain vigilant for additive effects on metabolic parameters whilst recognising that direct drug-drug interactions are not established.
Clinical Considerations for Concurrent Use
When prescribing Mounjaro and testosterone therapy concurrently, several clinical considerations should guide decision-making. Firstly, the metabolic benefits of both treatments may be complementary. Weight loss achieved with tirzepatide can improve testosterone levels naturally in men with obesity-related functional hypogonadism, potentially reducing the required dose of testosterone replacement. However, this would not apply to men with primary or classical hypogonadism, where TRT should not be withdrawn without endocrine specialist review. Clinicians should consider baseline testosterone levels and reassess after significant weight loss has occurred.
Cardiovascular risk assessment is paramount, as both medications influence cardiovascular health through different mechanisms. Testosterone therapy has complex cardiovascular effects, with some evidence suggesting increased risk in certain populations. NICE guidance emphasises individualised cardiovascular risk assessment for patients with type 2 diabetes, and this becomes particularly important when multiple therapies are involved. Patients with pre-existing cardiovascular disease require careful evaluation before initiating either treatment.
Patient selection should account for contraindications to each medication. According to the UK SmPC, Mounjaro is contraindicated in patients with hypersensitivity to the active substance or excipients, with caution advised in severe gastrointestinal disease such as gastroparesis. Testosterone therapy is contraindicated in men with prostate cancer, breast cancer, or known/suspected androgen-dependent tumours. Severe heart failure is a caution rather than an absolute contraindication for testosterone therapy, requiring monitoring for fluid retention and oedema. A comprehensive risk-benefit analysis is essential for each patient.
Dose titration strategies for Mounjaro should follow standard protocols, starting at 2.5 mg weekly and increasing gradually to minimise gastrointestinal adverse effects. When initiating or up-titrating tirzepatide, consider reducing doses of insulin or sulfonylureas to minimise hypoglycaemia risk. Testosterone dosing should be individualised based on serum testosterone levels and clinical response. The timing of initiating these therapies—whether simultaneously or sequentially—should be determined by clinical urgency, patient tolerance, and monitoring capacity. Sequential initiation may facilitate clearer attribution of adverse effects and metabolic changes to specific medications.
Monitoring and Safety Recommendations
Comprehensive monitoring protocols are essential for patients receiving both Mounjaro and testosterone therapy. For tirzepatide, baseline and ongoing monitoring should include:
-
Glycaemic control: HbA1c and fasting glucose levels should be assessed at baseline and every 3–6 months, with more frequent monitoring during dose titration or if hypoglycaemia risk is elevated (particularly in patients on concomitant insulin or sulphonylureas).
-
Renal function: Serum creatinine and estimated glomerular filtration rate (eGFR) should be monitored, especially in patients experiencing significant gastrointestinal adverse effects that may lead to dehydration.
-
Body weight and composition: Regular weight measurements help assess treatment efficacy and guide dose adjustments.
-
Retinopathy monitoring: Patients with pre-existing diabetic retinopathy should have ophthalmology review, particularly if experiencing rapid improvement in HbA1c.
For testosterone replacement therapy, monitoring should encompass:
-
Testosterone levels: Serum testosterone should be measured at baseline, 3 months after initiation, and then 6–12 monthly. For injectable preparations, measure trough levels before the next dose. Target levels typically range between 12–30 nmol/L, though individualisation is appropriate.
-
Haematocrit and haemoglobin: Testosterone can stimulate erythropoiesis, potentially leading to polycythaemia. Full blood count should be checked at baseline, 3–6 months, and annually thereafter. If haematocrit exceeds 0.54 (54%), consider pausing or adjusting TRT, investigating causes, and possibly arranging venesection.
-
Prostate monitoring: Digital rectal examination and prostate-specific antigen (PSA) testing should be performed at baseline and monitored according to age-appropriate guidelines. Consider urgent urology referral for PSA above age-specific range or abnormal DRE findings, in line with NICE NG12 guidance.
-
Lipid profile and liver function: Both should be assessed periodically, as testosterone can affect lipid metabolism and, rarely, hepatic function.
Safety considerations include vigilance for signs of pancreatitis (severe abdominal pain) with tirzepatide, gallbladder disease (right upper quadrant pain, fever, jaundice), and monitoring for symptoms of cardiovascular events, mood changes, or sleep apnoea exacerbation with testosterone therapy. Patients should be educated about potential adverse effects of both medications and encouraged to report suspected side effects via the MHRA Yellow Card Scheme.
When to Seek Medical Advice
Patients receiving both Mounjaro and testosterone therapy should be clearly informed about circumstances requiring urgent medical attention. Immediate contact with healthcare services (999 or emergency department) is warranted if patients experience:
-
Severe abdominal pain, particularly if persistent and radiating to the back, which may indicate pancreatitis—a rare but serious adverse effect of GLP-1 receptor agonists. Same-day urgent assessment is needed for suspected pancreatitis unless life-threatening features are present.
-
Chest pain, shortness of breath, or symptoms of stroke (facial drooping, arm weakness, speech difficulties), as both medications can influence cardiovascular risk factors.
-
Signs of severe allergic reaction, including facial swelling, difficulty breathing, or widespread rash.
-
Right upper quadrant pain, fever, or jaundice, which may indicate gallbladder disease associated with GLP-1 receptor agonists.
-
Sudden visual changes, which could reflect worsening diabetic retinopathy or other eye conditions requiring prompt assessment.
Patients should contact their GP or diabetes specialist nurse within 24–48 hours if they experience:
-
Persistent nausea, vomiting, or diarrhoea lasting more than 48 hours, which may lead to dehydration and acute kidney injury.
-
Symptoms of hypoglycaemia (tremor, sweating, confusion, palpitations), particularly if recurrent or severe.
-
New or worsening symptoms potentially related to testosterone therapy, such as significant mood changes, increased aggression, difficulty urinating, or ankle swelling.
-
Symptoms suggestive of erythrocytosis (new headaches, facial flushing, dizziness) or acute urinary retention requiring urgent clinical review.
-
Unexplained weight changes, either insufficient weight loss with tirzepatide or unexpected weight gain.
Routine follow-up should be maintained as scheduled, typically every 3–6 months initially, then annually once stable. Patients should never adjust doses of either medication without medical supervision, and should inform all healthcare providers (including dentists and pharmacists) about both treatments. If considering discontinuation of either therapy, this should be discussed with the prescribing clinician, as abrupt cessation may affect metabolic control or hormonal balance. Maintaining open communication with healthcare providers ensures optimal safety and therapeutic outcomes when using these medications concurrently.
Scientific References
- Mounjaro KwikPen 2.5mg solution for injection in pre-filled pen - Summary of Product Characteristics.
- Mounjaro - European Public Assessment Report.
- Metabolic Effects of Testosterone Replacement Therapy in Patients with Type 2 Diabetes or Metabolic Syndrome: A Meta-Analysis.
- Drug-Drug Interactions Between Glucagon-Like Peptide 1 Receptor Agonists and Other Medications.
- The 'male menopause'.
Frequently Asked Questions
Can I take Mounjaro and testosterone therapy together?
Yes, there is no documented direct interaction between Mounjaro (tirzepatide) and testosterone replacement therapy. However, both medications affect metabolic parameters and require comprehensive monitoring when used concurrently, including regular assessment of blood glucose, testosterone levels, and cardiovascular risk factors.
Does Mounjaro affect testosterone levels?
Mounjaro does not directly affect testosterone levels, but weight loss achieved with tirzepatide may naturally improve testosterone in men with obesity-related functional hypogonadism. Testosterone levels should be reassessed after significant weight loss has occurred.
What monitoring is needed when taking both Mounjaro and testosterone?
Monitoring should include HbA1c and glucose levels every 3–6 months, testosterone levels at 3 months then 6–12 monthly, full blood count for haematocrit, prostate-specific antigen testing, renal function, and cardiovascular risk assessment. More frequent monitoring may be required during dose titration or if adverse effects occur.
The health-related content published on this site is based on credible scientific sources and is periodically reviewed to ensure accuracy and relevance. Although we aim to reflect the most current medical knowledge, the material is meant for general education and awareness only.
The information on this site is not a substitute for professional medical advice. For any health concerns, please speak with a qualified medical professional. By using this information, you acknowledge responsibility for any decisions made and understand we are not liable for any consequences that may result.
Heading 1
Heading 2
Heading 3
Heading 4
Heading 5
Heading 6
Lorem ipsum dolor sit amet, consectetur adipiscing elit, sed do eiusmod tempor incididunt ut labore et dolore magna aliqua. Ut enim ad minim veniam, quis nostrud exercitation ullamco laboris nisi ut aliquip ex ea commodo consequat. Duis aute irure dolor in reprehenderit in voluptate velit esse cillum dolore eu fugiat nulla pariatur.
Block quote
Ordered list
- Item 1
- Item 2
- Item 3
Unordered list
- Item A
- Item B
- Item C
Bold text
Emphasis
Superscript
Subscript