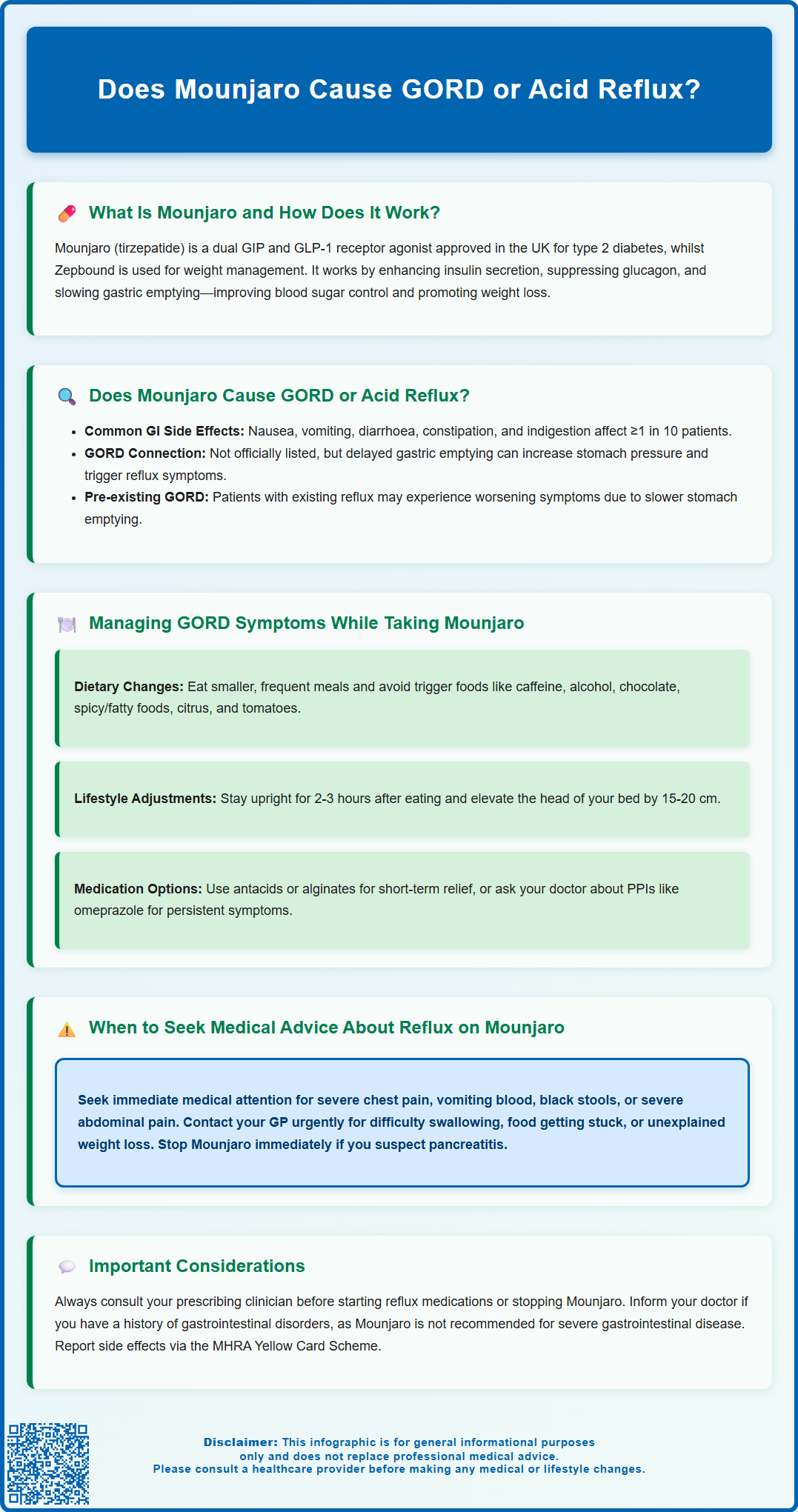
Mounjaro (tirzepatide) is a dual GIP and GLP-1 receptor agonist licensed in the UK for treating type 2 diabetes mellitus. Whilst gastro-oesophageal reflux disease (GORD) is not listed as a recognised adverse reaction in the Summary of Product Characteristics, gastrointestinal side effects—including nausea, dyspepsia, and abdominal discomfort—are very common. Mounjaro slows gastric emptying, which may theoretically contribute to reflux-like symptoms in some patients. Understanding the relationship between tirzepatide and GORD, alongside practical management strategies, is essential for patients and clinicians to optimise treatment outcomes and minimise discomfort.
Summary: Mounjaro does not directly cause GORD, but its effect on delaying gastric emptying may contribute to reflux-like symptoms in some patients.
- Tirzepatide is a dual GIP and GLP-1 receptor agonist licensed in the UK for type 2 diabetes mellitus.
- GORD is not listed as an adverse reaction, though gastrointestinal side effects such as nausea and dyspepsia are very common.
- Delayed gastric emptying may increase intra-gastric pressure and the likelihood of acid reflux into the oesophagus.
- Lifestyle modifications and pharmacological interventions such as PPIs can help manage reflux symptoms.
- Red flag symptoms including dysphagia, severe chest pain, or vomiting blood require urgent medical assessment.
Table of Contents
What Is Mounjaro and How Does It Work?
Mounjaro (tirzepatide) is a prescription medicine licensed in the UK for the treatment of type 2 diabetes mellitus. In the UK, tirzepatide for weight management in adults with obesity or overweight with weight-related comorbidities is marketed as Zepbound, not Mounjaro. Tirzepatide belongs to a novel class of medications known as dual glucose-dependent insulinotropic polypeptide (GIP) and glucagon-like peptide-1 (GLP-1) receptor agonists. By activating both GIP and GLP-1 receptors, tirzepatide offers a unique mechanism of action that distinguishes it from single-receptor GLP-1 agonists such as semaglutide.
The mechanism of action involves several physiological effects that contribute to improved glycaemic control and weight loss. Tirzepatide enhances insulin secretion from pancreatic beta cells in a glucose-dependent manner, meaning insulin is released primarily when blood glucose levels are elevated, thereby reducing the risk of hypoglycaemia (though this risk increases when used with insulin or sulfonylureas). Simultaneously, it suppresses glucagon secretion, which helps prevent excessive glucose production by the liver. Additionally, Mounjaro slows gastric emptying, prolonging the time food remains in the stomach, which contributes to increased satiety and reduced appetite. This delayed gastric emptying is central to its weight-loss effects but also underlies some of its gastrointestinal side effects and may affect the absorption of oral medicines, including oral contraceptives.
Mounjaro is administered as a once-weekly subcutaneous injection, with doses typically starting at 2.5 mg and gradually titrated upwards to minimise adverse effects. The Medicines and Healthcare products Regulatory Agency (MHRA) has approved Mounjaro for use in the UK, and the National Institute for Health and Care Excellence (NICE) provides guidance on its use within the NHS for eligible patients. Importantly, tirzepatide is not recommended in patients with severe gastrointestinal disease, including severe gastroparesis. Understanding how Mounjaro works is essential for recognising why certain gastrointestinal symptoms, including those resembling gastro-oesophageal reflux disease (GORD), may occur during treatment.
Does Mounjaro Cause GORD or Acid Reflux?
The relationship between Mounjaro and gastro-oesophageal reflux disease (GORD), also known as acid reflux, is an area of clinical interest, particularly given the medication's effects on the gastrointestinal system. GORD is not listed as an adverse reaction in the Summary of Product Characteristics (SmPC) for tirzepatide. However, gastrointestinal symptoms are among the most frequently reported side effects. These include nausea (very common, affecting ≥1 in 10 patients), vomiting (common, affecting ≥1 in 100 to <1 in 10), diarrhoea (very common), constipation (common), dyspepsia (indigestion), abdominal pain, and abdominal distension. Clinical trial data indicate that gastrointestinal adverse events occur in a significant proportion of patients, particularly during dose escalation.
While there is no established direct causal link between Mounjaro and the development of GORD, the medication's pharmacological action—specifically its effect on delaying gastric emptying—can theoretically contribute to reflux-like symptoms. When the stomach empties more slowly, gastric contents remain in the stomach for longer periods, which may increase intra-gastric pressure and the likelihood of acid refluxing into the oesophagus. Patients with pre-existing GORD or a history of reflux may be more susceptible to experiencing worsening symptoms while on Mounjaro.
It is important to distinguish between new-onset GORD and the exacerbation of pre-existing reflux symptoms. Some patients may experience dyspepsia or heartburn as part of the broader spectrum of gastrointestinal side effects without meeting the clinical criteria for GORD. Conversely, individuals with established GORD may notice an increase in symptom frequency or severity. If you experience persistent heartburn, regurgitation, or chest discomfort while taking Mounjaro, it is advisable to discuss these symptoms with your GP or diabetes specialist to determine whether they are related to the medication and to explore appropriate management strategies.
Managing GORD Symptoms While Taking Mounjaro
If you develop reflux-like symptoms while taking Mounjaro, several practical and pharmacological strategies can help manage discomfort and improve quality of life. Lifestyle modifications are often the first line of management and can be highly effective. These include:
-
Eating smaller, more frequent meals rather than large portions, which can reduce gastric distension and pressure.
-
Avoiding trigger foods and beverages such as caffeine, alcohol, chocolate, spicy or fatty foods, and acidic items like citrus fruits and tomatoes.
-
Remaining upright for at least two to three hours after eating to allow gravity to assist gastric emptying and reduce reflux risk.
-
Elevating the head of the bed by 15–20 cm, which can help prevent nocturnal reflux.
-
Maintaining a healthy weight and avoiding tight-fitting clothing around the abdomen.
In addition to lifestyle measures, pharmacological interventions may be appropriate, following a stepwise approach in line with NICE guidance. Antacids (such as calcium carbonate or magnesium hydroxide) and alginates (such as sodium alginate) can provide short-term symptomatic relief by neutralising stomach acid or forming a protective barrier. For more persistent symptoms, a short course of proton pump inhibitors (PPIs) such as omeprazole or lansoprazole may be recommended by your healthcare provider. If PPIs are not suitable, histamine-2 receptor antagonists (H2RAs) like famotidine might be considered. These medications reduce gastric acid production and should be reviewed regularly, with the lowest effective dose used for the shortest duration necessary.
It is essential to discuss any new or worsening reflux symptoms with your prescribing clinician before starting additional medications. They can assess whether dose adjustment of Mounjaro (such as slowing the titration schedule or temporarily reducing the dose) or alternative diabetes or weight-management therapies might be more appropriate. Your healthcare team can help balance the benefits of Mounjaro against any troublesome side effects. Do not discontinue Mounjaro without medical advice, as abrupt cessation may affect glycaemic control or weight-management progress.
If you experience persistent symptoms despite these measures, consult your GP for further assessment and management. Remember to report any suspected side effects to the MHRA Yellow Card Scheme (yellowcard.mhra.gov.uk).
When to Seek Medical Advice About Reflux on Mounjaro
While mild, intermittent reflux symptoms may be manageable with lifestyle changes and over-the-counter remedies, certain red flag symptoms warrant prompt medical evaluation. You should contact your GP or seek urgent medical attention if you experience:
-
Persistent or severe chest pain, particularly if it is new, unexplained, or associated with shortness of breath, as this may indicate a cardiac rather than gastrointestinal cause. For severe chest pain, call 999 immediately.
-
Difficulty swallowing (dysphagia) or a sensation of food getting stuck, which requires urgent assessment (2-week referral pathway) as this could suggest oesophageal complications or, rarely, malignancy.
-
Unintentional weight loss or loss of appetite beyond what is expected from Mounjaro's therapeutic effects, especially if you are aged 55 and over with additional upper gastrointestinal symptoms.
-
Vomiting blood or passing black, tarry stools (melaena), which may indicate gastrointestinal bleeding and requires immediate medical attention.
-
Severe, unrelenting abdominal pain, especially if radiating to the back and accompanied by vomiting, which could signal pancreatitis—a rare but serious adverse effect associated with GLP-1 receptor agonists. If pancreatitis is suspected, stop taking Mounjaro immediately and seek urgent medical assessment.
Additionally, if reflux symptoms are significantly impacting your quality of life, interfering with sleep, or not responding to initial management strategies, a review with your healthcare provider is advisable. Your GP may consider referral for upper gastrointestinal endoscopy based on NICE guidelines if there are concerns about complications such as oesophagitis, Barrett's oesophagus, or peptic ulcer disease.
It is also important to inform your clinician if you have a history of gastrointestinal disorders, including GORD, peptic ulcer disease, or gastroparesis, before starting Mounjaro, as tirzepatide is not recommended in severe gastrointestinal disease. Severe abdominal pain may also be caused by gallbladder disease, which has been associated with GLP-1-based therapies.
Regular follow-up appointments allow for monitoring of both therapeutic efficacy and tolerability, ensuring that any adverse effects are identified and managed promptly. Patient safety is paramount, and open communication with your healthcare team is key to optimising outcomes while on Mounjaro.
Frequently Asked Questions
Can Mounjaro worsen existing GORD symptoms?
Yes, Mounjaro may worsen pre-existing GORD symptoms due to delayed gastric emptying, which can increase intra-gastric pressure and reflux risk. Patients with a history of reflux should discuss this with their GP before starting treatment.
What should I do if I experience heartburn while taking Mounjaro?
Lifestyle modifications such as eating smaller meals, avoiding trigger foods, and remaining upright after eating can help. If symptoms persist, consult your GP, who may recommend antacids, alginates, or proton pump inhibitors.
When should I seek urgent medical advice for reflux symptoms on Mounjaro?
Seek urgent medical attention if you experience severe chest pain, difficulty swallowing, vomiting blood, black stools, or severe abdominal pain, as these may indicate serious complications requiring immediate assessment.
The health-related content published on this site is based on credible scientific sources and is periodically reviewed to ensure accuracy and relevance. Although we aim to reflect the most current medical knowledge, the material is meant for general education and awareness only.
The information on this site is not a substitute for professional medical advice. For any health concerns, please speak with a qualified medical professional. By using this information, you acknowledge responsibility for any decisions made and understand we are not liable for any consequences that may result.
Heading 1
Heading 2
Heading 3
Heading 4
Heading 5
Heading 6
Lorem ipsum dolor sit amet, consectetur adipiscing elit, sed do eiusmod tempor incididunt ut labore et dolore magna aliqua. Ut enim ad minim veniam, quis nostrud exercitation ullamco laboris nisi ut aliquip ex ea commodo consequat. Duis aute irure dolor in reprehenderit in voluptate velit esse cillum dolore eu fugiat nulla pariatur.
Block quote
Ordered list
- Item 1
- Item 2
- Item 3
Unordered list
- Item A
- Item B
- Item C
Bold text
Emphasis
Superscript
Subscript










