Many people taking Ozempic (semaglutide) for type 2 diabetes wonder whether grapefruit interferes with their medication. Unlike numerous oral drugs metabolised by liver enzymes that grapefruit affects, Ozempic is administered as a subcutaneous injection and follows a different metabolic pathway. No interaction between grapefruit and Ozempic is documented in UK regulatory guidance, including the MHRA Summary of Product Characteristics or the British National Formulary. Understanding how semaglutide works in your body and which dietary factors genuinely influence treatment outcomes helps you manage your diabetes safely and effectively whilst maintaining a balanced, enjoyable diet.
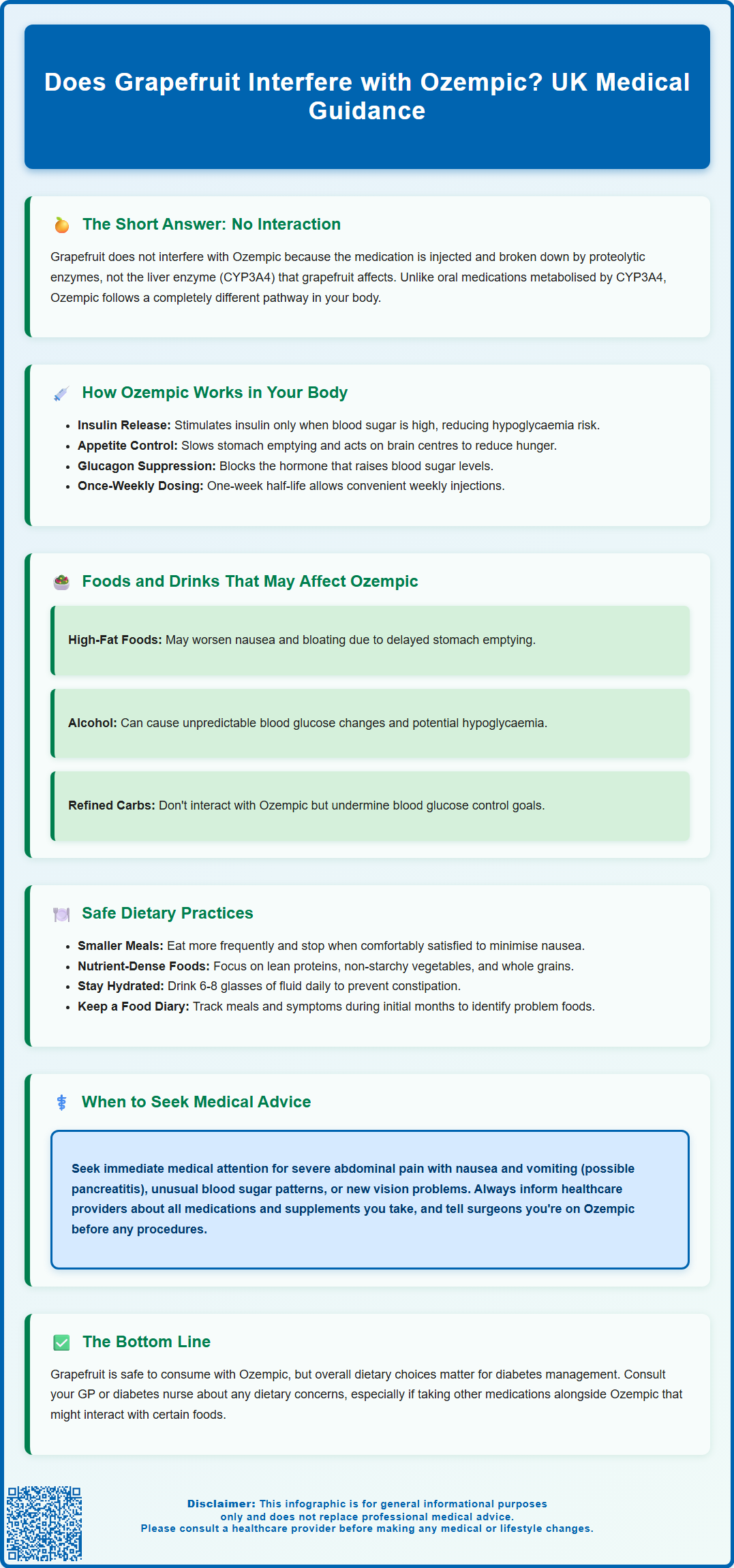
Summary: Grapefruit does not interfere with Ozempic (semaglutide) as no interaction is listed in UK regulatory guidance.
- Ozempic is a GLP-1 receptor agonist administered by subcutaneous injection, not metabolised by the CYP450 enzyme system that grapefruit affects.
- Semaglutide is broken down by proteolytic enzymes rather than liver pathways influenced by grapefruit compounds.
- The MHRA Summary of Product Characteristics and British National Formulary list no grapefruit-Ozempic interaction.
- Whilst grapefruit is safe with Ozempic, high-fat foods and alcohol may affect tolerability and blood glucose control.
- Patients taking warfarin alongside semaglutide should have INR monitoring when initiating treatment.
- Always inform your GP or pharmacist about all medications and supplements to identify potential interactions with other drugs.
Table of Contents
Does Grapefruit Interfere with Ozempic?
No interaction between grapefruit and Ozempic (semaglutide) is expected, and none is listed in the MHRA Summary of Product Characteristics (SmPC) or British National Formulary (BNF). Unlike many oral medications that are metabolised by specific liver enzymes, Ozempic is administered as a subcutaneous injection and follows a different metabolic pathway that is not affected by compounds found in grapefruit.
Grapefruit is well known for interacting with numerous medications, particularly those metabolised by the cytochrome P450 3A4 (CYP3A4) enzyme system in the liver and intestines. Compounds called furanocoumarins in grapefruit can inhibit this enzyme, leading to increased blood levels of certain drugs and potentially causing adverse effects. However, semaglutide is a glucagon-like peptide-1 (GLP-1) receptor agonist that is broken down by proteolytic enzymes rather than the CYP450 system.
Whilst grapefruit does not directly interfere with Ozempic's metabolism, patients should still consider their overall dietary choices when managing type 2 diabetes. Grapefruit itself has a low glycaemic index and contains beneficial nutrients, but portion control remains important. The absence of a direct drug interaction does not mean dietary considerations are irrelevant to your treatment outcomes.
If you have concerns about specific foods or beverages whilst taking Ozempic, it is always advisable to discuss these with your GP or diabetes specialist nurse. Individual circumstances, including other medications you may be taking alongside Ozempic, can influence dietary recommendations. Your healthcare team can provide personalised guidance based on your complete medical history and treatment plan.
How Ozempic Works in Your Body
Ozempic contains semaglutide, a GLP-1 receptor agonist (analogue) that mimics the action of the body's own incretin hormones released after eating. Understanding how Ozempic functions helps clarify why certain food interactions are unlikely whilst others may affect treatment outcomes.
When administered as a once-weekly subcutaneous injection, semaglutide binds to GLP-1 receptors found throughout the body, particularly in the pancreas, brain, and gastrointestinal tract. In the pancreas, it stimulates insulin secretion in a glucose-dependent manner, meaning insulin is only released when blood glucose levels are elevated. This mechanism significantly reduces the risk of hypoglycaemia compared to some other diabetes medications. Simultaneously, semaglutide suppresses the release of glucagon, a hormone that raises blood glucose levels, further contributing to improved glycaemic control.
Beyond its effects on glucose regulation, Ozempic slows gastric emptying, which means food remains in the stomach for longer periods. This delayed emptying contributes to increased feelings of fullness and reduced appetite. It's worth noting that this gastric-emptying effect is greatest initially and tends to diminish with continued treatment, as stated in the SmPC. The medication also acts on appetite centres in the brain, reducing hunger signals and food cravings.
Semaglutide has a half-life of approximately one week, which allows for once-weekly dosing. This prolonged action is due to strong albumin binding and its metabolic pathway. The medication is gradually broken down by proteolytic cleavage and beta-oxidation of the fatty-acid side chain, rather than through the liver's cytochrome P450 system. This metabolic pathway is why grapefruit, which affects CYP450 enzymes, does not interfere with Ozempic's effectiveness or safety profile.
Patients should be aware that rapid improvement in blood glucose control has been associated with temporary worsening of diabetic retinopathy in some cases. If you experience any new or worsening visual symptoms while taking Ozempic, seek prompt medical advice.
Foods and Drinks That May Affect Ozempic
Whilst grapefruit does not interact with Ozempic at a pharmacological level, certain dietary choices can influence how well you tolerate the medication and how effectively it helps manage your blood glucose. Understanding these relationships enables you to optimise your treatment outcomes and minimise potential side effects.
High-fat and greasy foods may exacerbate the gastrointestinal side effects commonly associated with Ozempic, particularly during the initial weeks of treatment or after dose increases. Because semaglutide slows gastric emptying, consuming fatty meals can lead to prolonged feelings of fullness, nausea, bloating, and discomfort. Many patients find that choosing lighter, lower-fat options helps them tolerate the medication more comfortably whilst still achieving their therapeutic goals.
Alcohol consumption warrants careful consideration when taking Ozempic. Whilst there is no direct pharmacological interaction, alcohol can affect blood glucose levels unpredictably—sometimes causing hypoglycaemia, particularly if you are taking other diabetes medications alongside semaglutide such as insulin or sulfonylureas. Regular blood glucose monitoring is advisable when consuming alcohol. The UK Chief Medical Officers' guidelines recommend limiting alcohol intake to no more than 14 units per week, spread over three or more days, with several alcohol-free days each week.
Foods with a high glycaemic index, such as refined carbohydrates and sugary items, do not interact with Ozempic's mechanism but can work against your treatment objectives. Whilst the medication helps regulate blood glucose, maintaining a balanced diet with appropriate portions of complex carbohydrates, lean proteins, and vegetables supports optimal diabetes management. The NHS Eatwell Guide and resources from Diabetes UK provide practical advice on creating balanced meals. Highly processed foods may also contribute to gastrointestinal discomfort when combined with Ozempic's effect on gastric emptying. Working with a dietitian can help you develop an eating plan that complements your medication regimen and addresses your individual health goals.
Safe Dietary Practices While Taking Ozempic
Adopting sensible dietary habits whilst taking Ozempic enhances both the medication's effectiveness and your overall wellbeing. NICE guideline NG28 (Type 2 diabetes in adults: management) emphasises that pharmacological interventions for type 2 diabetes should always be accompanied by lifestyle modifications, including dietary changes and increased physical activity.
Begin by eating smaller, more frequent meals rather than large portions. Because Ozempic slows gastric emptying, consuming large meals can lead to uncomfortable fullness, nausea, and potential vomiting. Many patients find that eating slowly and stopping when comfortably satisfied—rather than completely full—significantly improves their experience with the medication. This approach also aligns with mindful eating practices that support sustainable blood glucose management.
Prioritise nutrient-dense foods that provide essential vitamins, minerals, and fibre without excessive calories. Lean proteins such as chicken, fish, eggs, and legumes help maintain muscle mass and promote satiety. Non-starchy vegetables should form a substantial portion of your meals, providing fibre that supports digestive health and helps regulate blood glucose. Whole grains in appropriate portions offer sustained energy without causing rapid glucose spikes.
Hydration is particularly important when taking Ozempic. According to NHS guidance, adequate fluid intake (6-8 glasses of fluid daily) helps prevent constipation, a common side effect of GLP-1 receptor agonists, and supports overall metabolic function. Limiting caffeinated and sugary beverages helps avoid empty calories and potential blood glucose fluctuations.
Consider keeping a food diary during the initial months of treatment. Recording what you eat, when you eat, and any symptoms you experience can help identify patterns and trigger foods that may worsen side effects. This information is valuable when discussing your progress with your healthcare team and can inform adjustments to your dietary approach. If gastrointestinal symptoms persist or significantly impact your quality of life, discuss with your prescriber about adjusting the titration pace or temporarily modifying your dose. Remember that individual responses vary, and what works well for one person may not suit another.
When to Seek Medical Advice About Drug Interactions
Whilst grapefruit does not interact with Ozempic, it is essential to remain vigilant about potential interactions with other medications and to recognise situations requiring professional medical input. Open communication with your healthcare team ensures safe, effective treatment and helps prevent complications.
Always inform your GP, diabetes specialist nurse, or pharmacist about all medications you are taking, including prescription drugs, over-the-counter medicines, herbal supplements, and vitamins. Some medications may interact with Ozempic or require dose adjustments when used concurrently. For instance, if you take insulin or sulfonylureas alongside semaglutide, your risk of hypoglycaemia increases, and your healthcare provider may need to reduce doses of these other medications.
If you are taking warfarin or other coumarin anticoagulants, the MHRA SmPC advises that INR monitoring should be performed when initiating semaglutide treatment. Additionally, semaglutide may delay the absorption rate of some oral medicines due to its effect on gastric emptying. Consult your pharmacist if you are taking any medications with a narrow therapeutic index.
Seek prompt medical advice (contact NHS 111 or arrange a same-day GP appointment) if you experience severe or persistent gastrointestinal symptoms such as severe abdominal pain, particularly if accompanied by nausea and vomiting. Whilst mild nausea is common when starting Ozempic, severe symptoms could indicate pancreatitis, a rare but serious adverse effect requiring immediate medical attention. Other warning signs include persistent vomiting that prevents adequate fluid intake, signs of dehydration, or symptoms of gallbladder problems such as pain in the upper right abdomen.
Contact your healthcare provider if you notice unusual changes in your blood glucose patterns, particularly unexplained hypoglycaemia or persistently elevated readings despite medication adherence. These changes might indicate the need for dose adjustments or could signal interactions with newly started medications or supplements. Additionally, seek prompt review if you experience any new or worsening visual symptoms, as rapid improvement in blood glucose control can sometimes temporarily worsen diabetic retinopathy.
Before starting any new medication or supplement, including those purchased without prescription, consult your pharmacist or GP. They can review your complete medication list and advise on potential interactions. If you are planning surgery or dental procedures, inform the healthcare professionals involved that you are taking Ozempic, as this may influence perioperative management. The Centre for Perioperative Care (CPOC) and Association of Anaesthetists provide guidance on managing GLP-1 receptor agonists around the time of surgery due to potential aspiration risk. Your proactive engagement in your healthcare ensures the safest, most effective treatment outcomes.
Scientific References
- Type 2 diabetes in adults: management (NG28).
- Ozempic 0.25 mg, 0.5 mg, 1 mg solution for injection in pre-filled pen - Summary of Product Characteristics (SmPC).
- Semaglutide.
- Ozempic (semaglutide) - European Public Assessment Report.
- The Eatwell Guide.
- UK Chief Medical Officers' Low Risk Drinking Guidelines.
- Centre for Perioperative Care (CPOC) and Association of Anaesthetists - Guidance on perioperative management of GLP-1 receptor agonists.
Frequently Asked Questions
Can I eat grapefruit while taking Ozempic?
Yes, you can safely eat grapefruit whilst taking Ozempic as there is no documented interaction between grapefruit and semaglutide. Unlike many oral medications, Ozempic is not metabolised by the liver enzymes that grapefruit affects.
What foods should I avoid when taking Ozempic?
Whilst no foods are strictly prohibited with Ozempic, high-fat and greasy foods may worsen gastrointestinal side effects such as nausea and bloating. Limiting refined carbohydrates and sugary items supports optimal blood glucose management alongside your medication.
Does Ozempic interact with any other medications?
Ozempic may increase hypoglycaemia risk when taken with insulin or sulfonylureas, requiring dose adjustments of these medications. Patients taking warfarin should have INR monitoring when starting semaglutide, and the medication may delay absorption of some oral medicines due to slowed gastric emptying.
The health-related content published on this site is based on credible scientific sources and is periodically reviewed to ensure accuracy and relevance. Although we aim to reflect the most current medical knowledge, the material is meant for general education and awareness only.
The information on this site is not a substitute for professional medical advice. For any health concerns, please speak with a qualified medical professional. By using this information, you acknowledge responsibility for any decisions made and understand we are not liable for any consequences that may result.
Heading 1
Heading 2
Heading 3
Heading 4
Heading 5
Heading 6
Lorem ipsum dolor sit amet, consectetur adipiscing elit, sed do eiusmod tempor incididunt ut labore et dolore magna aliqua. Ut enim ad minim veniam, quis nostrud exercitation ullamco laboris nisi ut aliquip ex ea commodo consequat. Duis aute irure dolor in reprehenderit in voluptate velit esse cillum dolore eu fugiat nulla pariatur.
Block quote
Ordered list
- Item 1
- Item 2
- Item 3
Unordered list
- Item A
- Item B
- Item C
Bold text
Emphasis
Superscript
Subscript












