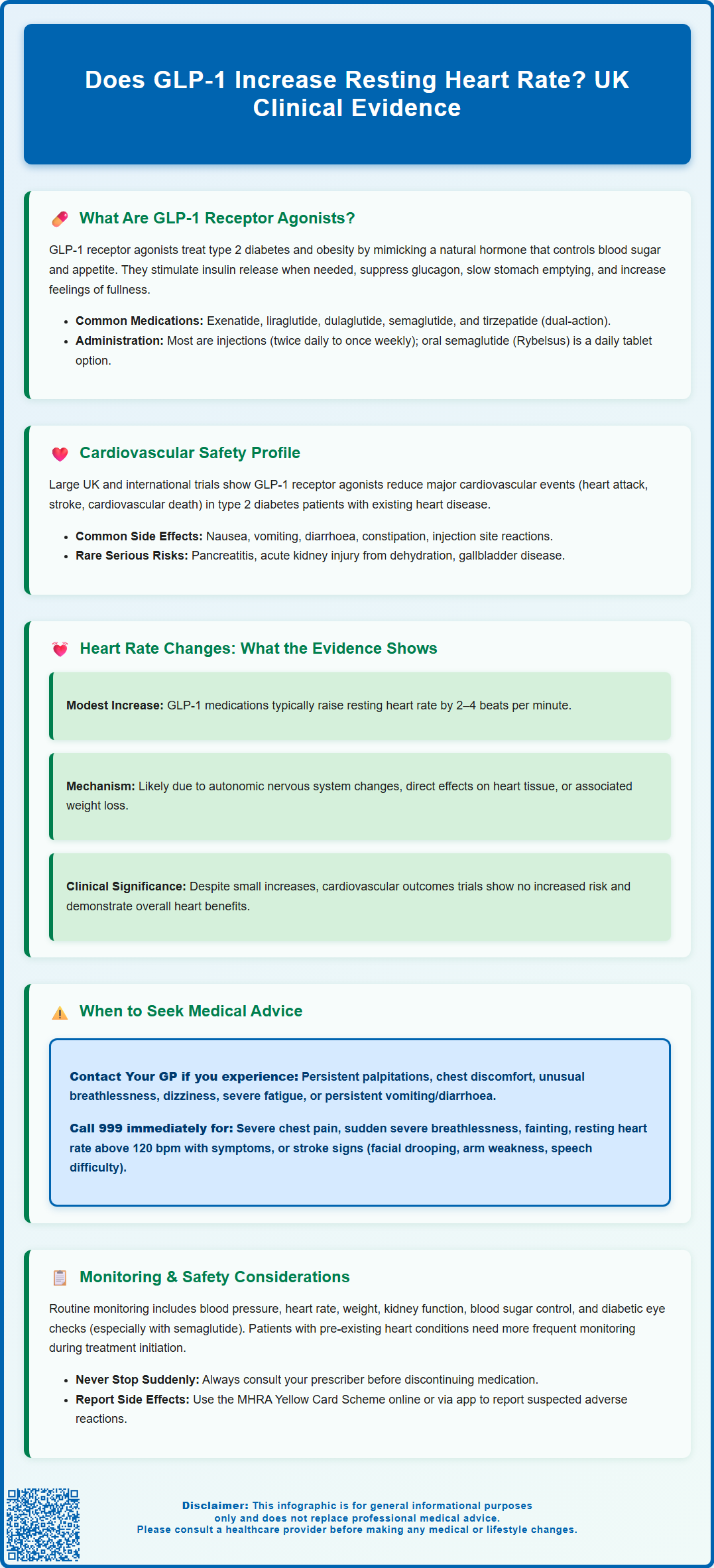
GLP-1 receptor agonists are increasingly prescribed for type 2 diabetes and weight management in the UK. A common question among patients and clinicians is: does GLP-1 increase resting heart rate? Clinical evidence indicates that these medications are associated with modest heart rate elevations, typically 2–4 beats per minute. Whilst this physiological change has been consistently observed in cardiovascular outcomes trials, it has not translated into increased cardiovascular risk. Understanding the clinical significance of heart rate changes, when to seek medical advice, and how these medications fit within UK prescribing guidance is essential for safe, effective use.
Summary: GLP-1 receptor agonists are associated with modest increases in resting heart rate, typically 2–4 beats per minute, which have not been linked to increased cardiovascular risk.
- GLP-1 receptor agonists mimic natural GLP-1 hormone to stimulate glucose-dependent insulin secretion and promote satiety.
- Heart rate increases are dose-dependent, agent-specific, occur early in treatment, and are generally clinically modest.
- Cardiovascular outcomes trials demonstrate favourable safety profiles with some agents reducing major adverse cardiovascular events.
- Proposed mechanisms include autonomic nervous system modulation and potential direct cardiac effects via GLP-1 receptors.
- Patients should seek medical advice for palpitations, chest discomfort, breathlessness, or persistent gastrointestinal symptoms.
- Routine monitoring includes heart rate, blood pressure, renal function, and glycaemic control in accordance with NICE guidance.
Table of Contents
What Are GLP-1 Receptor Agonists?
Glucagon-like peptide-1 (GLP-1) receptor agonists are a class of medications primarily used to manage type 2 diabetes mellitus and, more recently, for weight management in adults with obesity or overweight with weight-related comorbidities. These medicines work by mimicking the action of the naturally occurring hormone GLP-1, which is released from the intestine in response to food intake.
The mechanism of action involves several physiological processes. GLP-1 receptor agonists bind to GLP-1 receptors on pancreatic beta cells, stimulating glucose-dependent insulin secretion. This means insulin is released only when blood glucose levels are elevated, reducing the risk of hypoglycaemia compared with some other diabetes medications. Additionally, these agents suppress glucagon secretion from pancreatic alpha cells, slow gastric emptying, and promote satiety through central nervous system pathways, leading to reduced food intake and weight loss.
Commonly prescribed GLP-1 receptor agonists in the UK include:
-
Exenatide (Byetta, Bydureon)
-
Liraglutide (Victoza for diabetes; Saxenda for weight management)
-
Dulaglutide (Trulicity)
-
Semaglutide (Ozempic for diabetes; Wegovy for weight management; Rybelsus as an oral tablet)
Tirzepatide (Mounjaro) is a dual GIP/GLP-1 receptor agonist that works through similar but distinct mechanisms.
Most of these medications are administered via subcutaneous injection, with dosing frequencies ranging from twice daily to once weekly depending on the specific agent. Oral semaglutide (Rybelsus) is taken once daily as a tablet. NICE guidance supports their use in type 2 diabetes for people with established cardiovascular disease or high cardiovascular risk, or when additional therapy is needed despite metformin and/or SGLT2 inhibitors. For weight management, specific eligibility criteria apply. These medicines are licensed in the UK with specific indications, and prescribing should follow current clinical guidelines.
Cardiovascular Safety of GLP-1 Receptor Agonists
Cardiovascular outcomes trials have been a cornerstone of GLP-1 receptor agonist development, with regulatory bodies including the MHRA and EMA requiring robust cardiovascular safety data. These large-scale studies have generally demonstrated favourable cardiovascular profiles, with some agents showing significant reductions in major adverse cardiovascular events (MACE) in patients with type 2 diabetes and established cardiovascular disease.
Notably, liraglutide (LEADER trial) and semaglutide (SUSTAIN-6 trial) have demonstrated cardiovascular benefits, including reductions in cardiovascular death, non-fatal myocardial infarction, and non-fatal stroke. Dulaglutide (REWIND trial) similarly showed cardiovascular risk reduction. These findings have led to NICE recommendations supporting the use of certain GLP-1 receptor agonists in patients with type 2 diabetes and established cardiovascular disease or at high cardiovascular risk.
Common adverse effects of GLP-1 receptor agonists include:
-
Gastrointestinal symptoms (nausea, vomiting, diarrhoea, constipation)
-
Injection site reactions
-
Headache
-
Fatigue
-
Dizziness
Important safety considerations include:
-
Risk of hypoglycaemia when used with insulin or sulfonylureas (dose reduction of these agents may be needed)
-
Potential worsening of diabetic retinopathy with semaglutide in patients with pre-existing retinopathy
-
Risk of dehydration and acute kidney injury from persistent vomiting or diarrhoea
-
Pancreatitis, gallbladder disease, and potential thyroid C-cell tumours (observed in rodent studies, though human relevance remains uncertain)
Patients should be counselled about persistent severe abdominal pain as a potential warning sign of pancreatitis requiring immediate medical attention.
Regarding cardiovascular parameters, clinical trials have consistently observed modest increases in resting heart rate with GLP-1 receptor agonists, typically in the range of 2–4 beats per minute. However, this has not translated into increased cardiovascular risk; indeed, the overall cardiovascular safety profile remains favourable. The mechanism underlying heart rate changes is not fully elucidated but may involve autonomic nervous system modulation or direct cardiac effects.
Does GLP-1 Increase Resting Heart Rate?
Clinical evidence from cardiovascular outcomes trials and post-marketing surveillance indicates that GLP-1 receptor agonists are associated with modest increases in resting heart rate. Meta-analyses of randomised controlled trials have demonstrated mean increases of approximately 2–4 beats per minute, with variation depending on the specific agent, dose, and patient population.
The characteristics of heart rate increase appear to be:
-
Dose-dependent: Higher doses generally produce greater increases
-
Agent-specific: Some GLP-1 receptor agonists may have more pronounced effects than others
-
Time-dependent: Heart rate changes typically occur early in treatment and may stabilise over time
-
Clinically modest: The absolute increase is generally small and within normal physiological variation
Proposed mechanisms for heart rate elevation include modulation of autonomic nervous system activity, with potential reduction in parasympathetic (vagal) tone or increase in sympathetic activity. GLP-1 receptors are expressed in various cardiovascular tissues, including the sinoatrial node, and direct cardiac effects cannot be excluded. Weight loss associated with these medications may also influence cardiovascular parameters, though the relationship is complex.
Clinical significance of these heart rate changes remains an area of ongoing research. Importantly, despite modest heart rate increases, cardiovascular outcomes trials have not demonstrated increased cardiovascular risk. In fact, as noted previously, several GLP-1 receptor agonists have shown cardiovascular benefits. No consistent increase in arrhythmias has been demonstrated in cardiovascular outcomes trials.
Patients with pre-existing cardiac conditions, particularly those with heart failure or significant arrhythmias, should be monitored appropriately when initiating GLP-1 receptor agonist therapy. However, there is no official contraindication based solely on heart rate considerations, and these medications can be used safely in most patients with cardiovascular disease under appropriate medical supervision.
When to Seek Medical Advice About Heart Rate Changes
Patients prescribed GLP-1 receptor agonists should be aware of normal physiological responses versus symptoms requiring medical attention. While modest heart rate increases are expected and generally well-tolerated, certain symptoms warrant prompt evaluation.
Contact your GP or healthcare provider if you experience:
-
Palpitations: Awareness of rapid, forceful, or irregular heartbeat, particularly if persistent or distressing
-
Chest discomfort: Any chest pain, pressure, or tightness, especially with exertion
-
Breathlessness: Unusual shortness of breath, particularly if worsening or occurring at rest
-
Dizziness or lightheadedness: Especially if associated with near-fainting episodes
-
Fatigue: Marked, unexplained tiredness that interferes with daily activities
-
Persistent vomiting or diarrhoea: Which could lead to dehydration and kidney problems
If you're unsure whether you need urgent care and cannot contact your GP, call NHS 111.
Seek immediate medical attention (call 999 or attend A&E) if you experience:
-
Severe chest pain or pressure
-
Sudden severe breathlessness
-
Loss of consciousness or fainting
-
Rapid heart rate (>120 beats per minute at rest) with associated symptoms
-
Symptoms suggestive of stroke (facial drooping, arm weakness, speech difficulty)
Routine monitoring is important for patients on GLP-1 receptor agonists. Your healthcare team will typically assess:
-
Blood pressure and heart rate at follow-up appointments
-
Glycaemic control (HbA1c) in diabetes patients
-
Weight and body mass index
-
Renal function
-
Diabetic retinopathy (particularly with semaglutide if you have pre-existing retinopathy)
-
Symptoms and tolerability
Patients with pre-existing cardiovascular conditions may require more frequent monitoring, particularly during treatment initiation and dose escalation. If you have concerns about heart rate changes or any other symptoms while taking a GLP-1 receptor agonist, do not discontinue the medication without consulting your prescriber. Your healthcare provider can assess whether symptoms are related to the medication, require investigation, or necessitate treatment adjustment.
If you suspect you are experiencing side effects from your medication, you can report these through the MHRA Yellow Card Scheme (yellowcard.mhra.gov.uk or via the Yellow Card app). NICE guidance emphasises individualised care, and treatment decisions should be made collaboratively between patients and healthcare professionals, considering the overall benefit-risk profile for each individual.
Frequently Asked Questions
How much does GLP-1 increase heart rate?
Clinical trials show GLP-1 receptor agonists typically increase resting heart rate by 2–4 beats per minute. This modest elevation is dose-dependent and generally occurs early in treatment, stabilising over time.
Is the heart rate increase from GLP-1 dangerous?
No, the modest heart rate increase has not been associated with increased cardiovascular risk in large clinical trials. Several GLP-1 receptor agonists have demonstrated cardiovascular benefits despite these small heart rate changes.
Should I monitor my heart rate whilst taking GLP-1 medication?
Your healthcare team will routinely monitor heart rate and blood pressure at follow-up appointments. Contact your GP if you experience palpitations, chest discomfort, breathlessness, or dizziness whilst taking GLP-1 receptor agonists.
The health-related content published on this site is based on credible scientific sources and is periodically reviewed to ensure accuracy and relevance. Although we aim to reflect the most current medical knowledge, the material is meant for general education and awareness only.
The information on this site is not a substitute for professional medical advice. For any health concerns, please speak with a qualified medical professional. By using this information, you acknowledge responsibility for any decisions made and understand we are not liable for any consequences that may result.
Heading 1
Heading 2
Heading 3
Heading 4
Heading 5
Heading 6
Lorem ipsum dolor sit amet, consectetur adipiscing elit, sed do eiusmod tempor incididunt ut labore et dolore magna aliqua. Ut enim ad minim veniam, quis nostrud exercitation ullamco laboris nisi ut aliquip ex ea commodo consequat. Duis aute irure dolor in reprehenderit in voluptate velit esse cillum dolore eu fugiat nulla pariatur.
Block quote
Ordered list
- Item 1
- Item 2
- Item 3
Unordered list
- Item A
- Item B
- Item C
Bold text
Emphasis
Superscript
Subscript