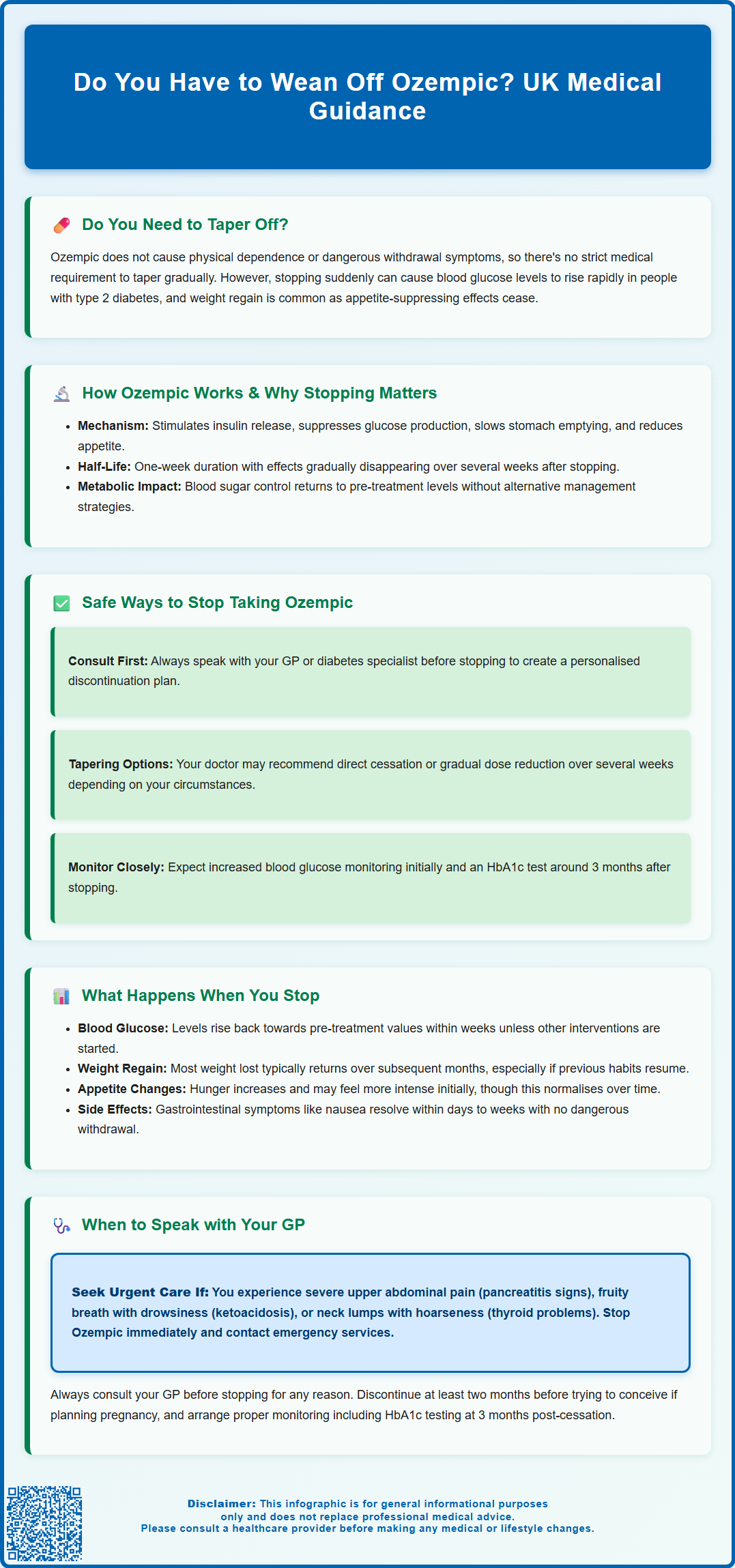
Do you have to wean off Ozempic? Many patients wonder whether stopping this diabetes medication requires a gradual tapering process. Whilst Ozempic (semaglutide) does not cause physical dependence or withdrawal symptoms, discontinuing it can lead to significant metabolic changes, particularly for people with type 2 diabetes. Blood glucose levels may rise, and weight regain is common. Although there is no strict medical requirement to taper the dose, the decision to stop should always be made in consultation with your GP or diabetes specialist, who can provide personalised guidance and arrange appropriate monitoring during the transition period.
Summary: There is no strict medical requirement to wean off Ozempic gradually, as it does not cause physical dependence or withdrawal symptoms, but stopping should be discussed with your GP due to potential metabolic consequences.
- Ozempic (semaglutide) is a GLP-1 receptor agonist licensed in the UK for type 2 diabetes treatment, administered as a once-weekly subcutaneous injection.
- Stopping Ozempic does not cause withdrawal symptoms, but blood glucose levels typically rise within weeks in people with diabetes, and weight regain is common.
- The medication has a one-week half-life, meaning its glucose-lowering and appetite-suppressing effects diminish over several weeks after discontinuation.
- Some healthcare professionals may recommend gradual dose reduction to allow time for alternative management strategies and smoother metabolic transition.
- Always consult your GP or diabetes specialist before stopping to ensure appropriate monitoring and alternative treatments are in place.
Table of Contents
Do You Have to Wean Off Ozempic?
The short answer is that there is no strict medical requirement to wean off Ozempic (semaglutide) gradually, unlike some medications where abrupt cessation can cause dangerous withdrawal symptoms. Ozempic is not associated with physical dependence or withdrawal syndromes in the traditional sense. However, the decision to stop should always be made in consultation with your GP or diabetes specialist, as stopping suddenly can have important metabolic consequences.
In the UK, Ozempic is licensed specifically for treating type 2 diabetes, while Wegovy (also semaglutide, but at a higher dose) is licensed for weight management. If you're using Ozempic for weight loss, this is considered off-label use.
Whilst you can technically stop Ozempic immediately without experiencing withdrawal effects, doing so may lead to a rapid return of elevated blood glucose levels, particularly in people with type 2 diabetes. The medication works by enhancing insulin secretion and reducing glucagon release, effects that diminish over several weeks after discontinuation due to semaglutide's approximately one-week half-life. For individuals using Ozempic primarily for weight management, stopping abruptly may result in weight regain, as the appetite-suppressing effects will cease.
Some healthcare professionals may recommend a gradual reduction in dose before stopping completely, not because of withdrawal concerns, but to allow time for alternative management strategies to be implemented. This approach can help smooth the transition and prevent sudden metabolic changes. The decision should be individualised based on your specific circumstances, including why you were prescribed Ozempic, your current health status, and what alternative treatments might be appropriate.
It is essential to discuss any plans to stop Ozempic with your healthcare team rather than making this decision independently, as they can provide guidance tailored to your medical needs and help monitor your condition during the transition period.
How Ozempic Works and Why Stopping Matters
Ozempic contains semaglutide, a glucagon-like peptide-1 (GLP-1) receptor agonist that mimics the action of naturally occurring GLP-1 hormones in the body. The medication works through several complementary mechanisms to improve glycaemic control and promote weight loss. It stimulates insulin secretion from pancreatic beta cells in a glucose-dependent manner, meaning insulin is released only when blood glucose levels are elevated, which reduces the risk of hypoglycaemia compared to some other diabetes medications.
Additionally, semaglutide suppresses glucagon secretion from pancreatic alpha cells, thereby reducing hepatic glucose production. It also slows gastric emptying, which helps moderate post-meal blood glucose spikes and contributes to increased satiety. The medication acts on appetite centres in the brain, reducing hunger and food intake, which explains its effectiveness for weight management. Ozempic has a long half-life of approximately one week, which is why it is administered as a once-weekly subcutaneous injection.
Understanding these mechanisms helps explain why stopping matters. When you discontinue Ozempic, these beneficial effects cease relatively quickly, though they wane over several weeks as the drug clears from your system. Blood glucose regulation returns to its pre-treatment state unless other interventions are in place. For people with type 2 diabetes, this means their HbA1c levels may rise, potentially increasing the risk of both acute hyperglycaemia and long-term diabetic complications. The appetite-suppressing effects also disappear, often leading to increased hunger and subsequent weight regain.
While there is no withdrawal syndrome, the metabolic changes that occur after stopping can be significant, particularly for those with advanced diabetes. In some vulnerable patients, the return to poor glycaemic control could lead to symptomatic hyperglycaemia (increased thirst, frequent urination, fatigue) or, rarely, more serious conditions. This is why planning for discontinuation is important, ensuring that alternative management strategies—whether lifestyle modifications, other medications, or both—are ready to be implemented.
Safe Ways to Stop Taking Ozempic
The safest approach to stopping Ozempic begins with a conversation with your GP or diabetes specialist. They will assess your individual circumstances, including your current glycaemic control, weight management goals, reasons for discontinuation, and overall health status. Based on this assessment, they can recommend the most appropriate strategy for you.
For some patients, particularly those with well-controlled diabetes who have made significant lifestyle changes, a direct cessation may be appropriate. Your healthcare team will likely arrange follow-up appointments to monitor your blood glucose levels after stopping, with home blood glucose monitoring intensified during the initial weeks. An HbA1c check should be scheduled at around 3 months after stopping, as earlier measurements may not fully reflect the change in glycaemic control.
Alternatively, your doctor might suggest a gradual dose reduction, stepping down from your current dose (whether 0.5 mg, 1 mg, or 2 mg weekly) to a lower dose for several weeks before stopping completely. This approach allows your body to adjust more gradually and provides an opportunity to implement or optimise other management strategies. During this tapering period, you might work with a dietitian to reinforce dietary changes, increase physical activity, or begin alternative medications.
If you're also taking insulin or sulfonylureas, your doctor will provide specific guidance on adjusting these medications when stopping Ozempic to avoid the risk of hypoglycaemia or hyperglycaemia.
If Ozempic is being stopped due to side effects, your healthcare team can explore other GLP-1 receptor agonists or different classes of diabetes medications that might be better tolerated. NICE guidelines recommend individualised treatment approaches for type 2 diabetes, considering factors such as HbA1c targets, cardiovascular risk, renal function, and patient preferences.
While medical guidance is strongly recommended before stopping Ozempic, you should seek urgent medical advice and stop immediately if you experience symptoms of serious adverse effects such as severe abdominal pain (which might indicate pancreatitis). Contact NHS 111 or your GP urgently if you develop concerning symptoms after stopping, or call 999 if you become severely unwell.
What Happens When You Stop Ozempic
The most immediate and predictable effect of stopping Ozempic is the return of elevated blood glucose levels in people with type 2 diabetes. Clinical studies have demonstrated that glycaemic control typically deteriorates within weeks of discontinuation, with HbA1c levels rising back towards pre-treatment values unless other interventions are implemented. The speed and extent of this rise depend on various factors, including the severity of your underlying diabetes, your lifestyle habits, and whether alternative medications are started.
Weight regain is another common consequence reported by many patients after stopping Ozempic. Research from clinical trials, particularly the STEP 1 extension study (primarily using the higher 2.4 mg Wegovy dose), indicates that much of the weight lost during treatment may return over subsequent months, particularly if dietary and exercise habits revert to pre-treatment patterns. Similar trends may occur at the lower doses used for diabetes. This occurs because the appetite-suppressing effects of semaglutide cease, often leading to increased hunger and caloric intake. Some patients report feeling significantly hungrier after stopping compared to before they started the medication, though this typically normalises over time.
Gastrointestinal symptoms that some people experience while taking Ozempic—such as nausea, reduced appetite, or altered bowel habits—generally resolve within days to weeks after stopping, as the medication clears from the system over several weeks. For individuals who found these effects troublesome, this represents a welcome improvement. However, those who benefited from reduced appetite may find the return of normal hunger challenging to manage.
There is no evidence of dangerous withdrawal symptoms or rebound effects beyond the return of the underlying metabolic condition. You will not experience physical dependence or acute withdrawal syndromes. However, the psychological adjustment to stopping can be significant, particularly regarding appetite changes and concerns about weight regain. Cardiovascular benefits observed during treatment in studies such as SUSTAIN-6 are dependent on continued therapy; while protection is demonstrated during active treatment, the long-term effects after stopping are not well established. This is an important consideration for patients with established cardiovascular disease.
When to Speak with Your GP About Stopping Ozempic
You should contact your GP or diabetes specialist before making any decision to stop Ozempic. This conversation is essential whether you are considering stopping due to side effects, cost concerns, achievement of treatment goals, or any other reason. Your healthcare team can assess whether discontinuation is appropriate and help develop a safe transition plan tailored to your circumstances.
Specific situations that warrant urgent discussion include:
-
Severe or persistent side effects such as severe nausea, vomiting, abdominal pain, or signs of pancreatitis (severe upper abdominal pain radiating to the back)—seek immediate medical attention and stop taking Ozempic if pancreatitis is suspected
-
Symptoms of thyroid problems, including a lump in the neck, hoarseness, difficulty swallowing, or shortness of breath (rodent studies showed C-cell tumours with semaglutide, though the relevance to humans remains uncertain)
-
Signs of diabetic ketoacidosis (DKA) such as abdominal pain, nausea, vomiting, deep breathing, drowsiness or fruity-smelling breath—call NHS 111 or 999 if you suspect DKA
-
Symptoms of gallbladder disease such as persistent right-upper abdominal pain, fever, or yellowing of the skin/eyes
-
Pregnancy or planning pregnancy, as GLP-1 receptor agonists should be discontinued at least two months before conception
-
Significant changes in renal function or symptoms suggesting kidney problems
You should also arrange a planned discussion if:
-
You have achieved your target HbA1c and weight goals and wish to explore whether continued treatment is necessary
-
You are experiencing financial difficulties affording the medication
-
You are concerned about long-term use or potential risks
-
You are planning surgery or other medical procedures—inform your surgical and anaesthetic teams about your Ozempic use
Your GP can arrange appropriate monitoring after stopping, including home blood glucose checks, HbA1c measurements at around 3 months, and weight monitoring. They can also discuss alternative management strategies, whether lifestyle-based or pharmacological, to maintain the benefits achieved during Ozempic treatment. NICE recommends regular review of all diabetes medications to ensure they remain appropriate and effective, so discussing your treatment plan is an important part of ongoing diabetes care.
If you experience any suspected side effects from Ozempic, these can be reported through the MHRA Yellow Card scheme, which helps monitor the safety of medicines in the UK. Never feel hesitant to raise concerns about your medication—open communication with your healthcare team is fundamental to safe and effective diabetes management.
Frequently Asked Questions
Can I stop taking Ozempic suddenly without medical supervision?
Whilst Ozempic does not cause dangerous withdrawal symptoms, you should always consult your GP or diabetes specialist before stopping, as blood glucose levels may rise rapidly and weight regain is common. Your healthcare team can arrange appropriate monitoring and alternative management strategies.
What happens to my blood sugar levels after stopping Ozempic?
Blood glucose levels typically rise within weeks of stopping Ozempic, with HbA1c returning towards pre-treatment values unless other interventions are implemented. Your GP should arrange follow-up monitoring and may recommend alternative diabetes medications or lifestyle modifications.
Will I regain weight after stopping Ozempic?
Weight regain is common after stopping Ozempic because the appetite-suppressing effects cease, often leading to increased hunger and caloric intake. Maintaining dietary changes and physical activity established during treatment can help minimise weight regain.
The health-related content published on this site is based on credible scientific sources and is periodically reviewed to ensure accuracy and relevance. Although we aim to reflect the most current medical knowledge, the material is meant for general education and awareness only.
The information on this site is not a substitute for professional medical advice. For any health concerns, please speak with a qualified medical professional. By using this information, you acknowledge responsibility for any decisions made and understand we are not liable for any consequences that may result.
Heading 1
Heading 2
Heading 3
Heading 4
Heading 5
Heading 6
Lorem ipsum dolor sit amet, consectetur adipiscing elit, sed do eiusmod tempor incididunt ut labore et dolore magna aliqua. Ut enim ad minim veniam, quis nostrud exercitation ullamco laboris nisi ut aliquip ex ea commodo consequat. Duis aute irure dolor in reprehenderit in voluptate velit esse cillum dolore eu fugiat nulla pariatur.
Block quote
Ordered list
- Item 1
- Item 2
- Item 3
Unordered list
- Item A
- Item B
- Item C
Bold text
Emphasis
Superscript
Subscript












