Do you have to take a GLP-1 forever? This is a common question for people prescribed glucagon-like peptide-1 (GLP-1) receptor agonists for type 2 diabetes or obesity. The answer depends on your underlying condition, treatment response, and individual circumstances. For type 2 diabetes, GLP-1 medications are typically long-term treatments due to the progressive nature of the condition, though some patients may reduce therapy with sustained lifestyle changes. For obesity, NHS-commissioned treatment with semaglutide 2.4mg (Wegovy) is limited to a maximum of two years through specialist services. This article explores treatment duration, what happens when you stop, and factors influencing how long you may need GLP-1 therapy.
Summary: Whether you need to take GLP-1 medications indefinitely depends on your condition—type 2 diabetes typically requires long-term treatment, whilst NHS-commissioned obesity treatment is limited to a maximum of two years.
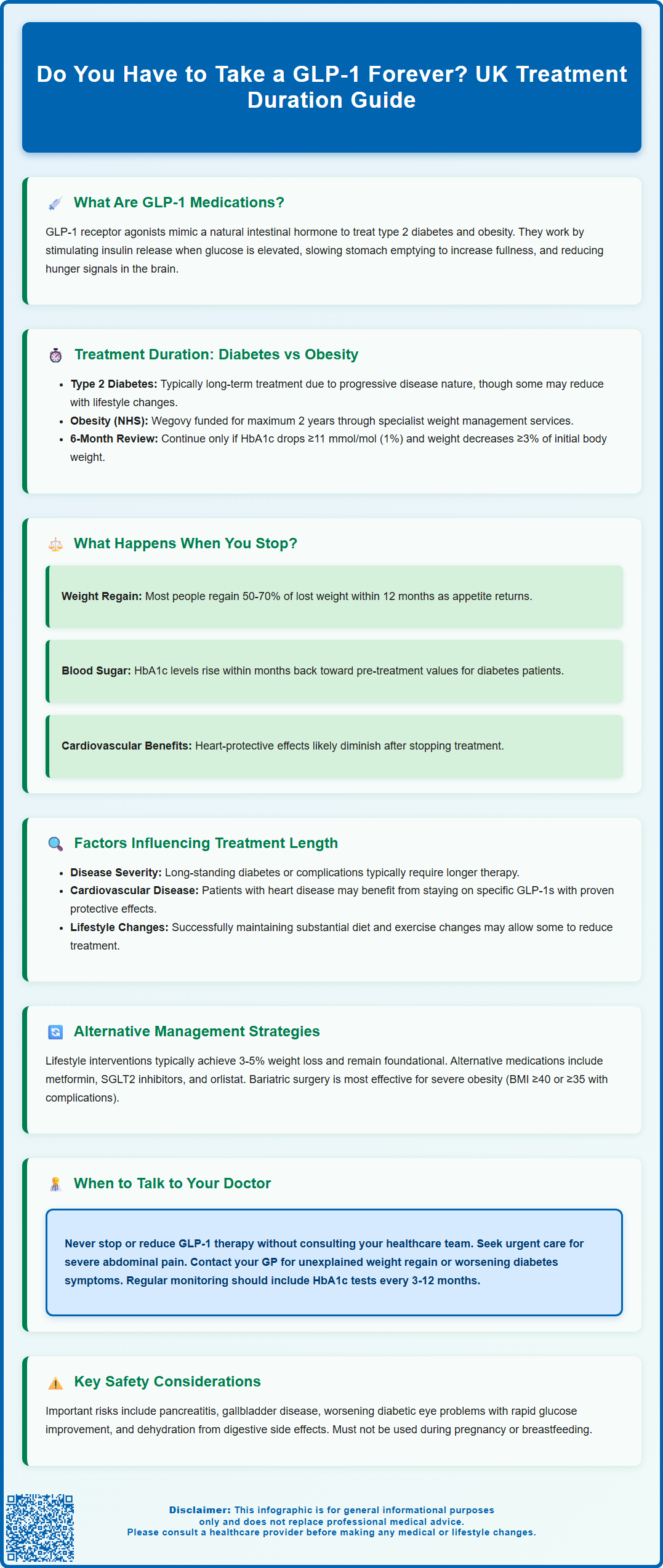
- GLP-1 receptor agonists stimulate insulin secretion, suppress glucagon, slow gastric emptying, and reduce appetite through multiple physiological pathways.
- Type 2 diabetes is a progressive condition requiring ongoing management, though some patients may reduce therapy with sustained lifestyle modifications under medical supervision.
- NHS-commissioned semaglutide 2.4mg (Wegovy) for obesity is restricted to specialist weight management services with a maximum treatment duration of two years.
- Stopping GLP-1 therapy typically leads to weight regain (50-70% within 12 months) and worsening glycaemic control in diabetes patients.
- NICE recommends reviewing GLP-1 treatment at six months and continuing only with meaningful HbA1c reduction (≥11 mmol/mol) and ≥3% weight loss.
- Treatment duration decisions require regular review with your healthcare team, considering response, tolerability, comorbidities, and individual circumstances.
Table of Contents
What Are GLP-1 Medications and How Do They Work?
Glucagon-like peptide-1 (GLP-1) receptor agonists are a class of medications primarily used to manage type 2 diabetes and, more recently, obesity. Most are injectable, though oral semaglutide (Rybelsus) is also available in the UK for type 2 diabetes. These medications mimic the action of naturally occurring GLP-1, a hormone produced in the intestine that plays a crucial role in glucose regulation and appetite control. Common examples include semaglutide (Ozempic, Wegovy, Rybelsus), dulaglutide (Trulicity), and liraglutide (Victoza, Saxenda).
The mechanism of action involves several physiological pathways. GLP-1 receptor agonists stimulate insulin secretion from pancreatic beta cells in a glucose-dependent manner, meaning they only promote insulin release when blood glucose levels are elevated. This reduces the risk of hypoglycaemia, though this risk increases when combined with insulin or sulfonylureas. Simultaneously, these drugs suppress glucagon secretion, a hormone that raises blood glucose, further contributing to glycaemic control.
Beyond glucose regulation, GLP-1 medications significantly affect appetite and satiety. They slow gastric emptying, prolonging the feeling of fullness after meals, and act on appetite centres in the brain to reduce hunger signals. This dual action on metabolism and appetite has made them particularly effective for weight management, with clinical trials demonstrating substantial weight loss in people with obesity.
The NICE guidelines recognise GLP-1 receptor agonists as valuable treatment options for type 2 diabetes when other therapies have proven insufficient. For weight management, medications like Wegovy (semaglutide 2.4mg) are restricted to specialist weight management services with specific eligibility criteria. Important safety considerations include risks of pancreatitis, gallbladder disease, diabetic retinopathy progression with rapid blood glucose improvement, and dehydration from gastrointestinal side effects. These medications are contraindicated in pregnancy and breastfeeding.
Do You Have to Take a GLP-1 Forever?
The question of whether GLP-1 medications require lifelong use does not have a straightforward answer, as it depends on the underlying condition being treated and individual patient circumstances. For type 2 diabetes, GLP-1 receptor agonists are generally considered a long-term treatment, as diabetes is a chronic progressive condition requiring ongoing management. However, 'forever' may not be accurate for everyone.
In diabetes management, the need for continued GLP-1 therapy relates to the progressive nature of beta-cell dysfunction. Type 2 diabetes typically worsens over time without intervention, and stopping effective medication often results in deteriorating glycaemic control. NICE guidelines (NG28) recommend reviewing GLP-1 treatment at around 6 months and continuing only if there has been a meaningful reduction in HbA1c (typically at least 11 mmol/mol [1%]) and weight loss of at least 3% of initial body weight. Some patients who achieve significant lifestyle modifications may be able to reduce or discontinue GLP-1 therapy under careful medical supervision, though this is not common.
For obesity treatment, the situation is different in the UK. Semaglutide 2.4mg (Wegovy) is commissioned by the NHS only through specialist weight management services, with specific eligibility criteria (including BMI thresholds, which are lower for people from some ethnic groups) and a maximum treatment duration of 2 years. Clinical evidence suggests that weight regain is common after discontinuing GLP-1 medications, as the underlying biological drivers of obesity—including appetite dysregulation and metabolic adaptations—typically persist. The STEP trials with semaglutide demonstrated that participants regained approximately two-thirds of their lost weight within a year of stopping treatment.
Regular review with your healthcare provider is essential to determine the most appropriate treatment duration for your specific circumstances, with decisions based on therapeutic response, tolerability, patient preferences, and ongoing risk-benefit assessment.
What Happens When You Stop Taking GLP-1 Medications?
Discontinuing GLP-1 receptor agonists typically leads to reversal of their therapeutic effects, though the timeline and extent vary between individuals. Understanding these changes is important for informed decision-making about treatment continuation.
Weight regain is one of the most documented consequences of stopping GLP-1 therapy. Research, including the STEP 1 extension study with semaglutide, consistently shows that most people experience a return of appetite to pre-treatment levels within weeks of discontinuation. The metabolic adaptations that contributed to weight loss—including reduced hunger signalling and delayed gastric emptying—diminish as the medication clears from the system. Without ongoing lifestyle interventions, patients may regain 50-70% of lost weight within 12 months of stopping treatment.
For those using GLP-1 medications for diabetes management, discontinuation often results in worsening glycaemic control. HbA1c levels typically rise within months, returning towards pre-treatment values. This occurs because the underlying insulin resistance and beta-cell dysfunction remain unchanged. Your diabetes care team will need to adjust your treatment plan, potentially introducing or intensifying alternative medications to maintain glucose targets.
Cardiovascular benefits associated with some GLP-1 receptor agonists (semaglutide, dulaglutide, liraglutide) observed in clinical trials are likely to diminish after discontinuation, though the exact persistence of these benefits remains uncertain.
Physically, most people do not experience withdrawal symptoms, as GLP-1 medications are not associated with physiological dependence. However, the return of appetite and hunger can feel pronounced after months of suppression. Some patients report gastrointestinal changes as their digestive system readjusts to normal gastric emptying rates.
If you are considering stopping GLP-1 therapy, discuss a structured monitoring plan with your GP or specialist, including regular checks of HbA1c, weight, blood pressure and lipids. Seek urgent medical attention if you experience severe, persistent abdominal pain, which could indicate pancreatitis.
Factors That Influence How Long You Need GLP-1 Treatment
Several clinical and personal factors determine the appropriate duration of GLP-1 therapy, and these should be regularly reviewed with your healthcare team.
Underlying condition severity is paramount. Individuals with long-standing type 2 diabetes, particularly those with significant beta-cell dysfunction or complications, typically require longer-term treatment. Conversely, someone with recent-onset diabetes and substantial weight loss may potentially reduce therapy if lifestyle changes are maintained and glycaemic control remains stable. For obesity treatment in the UK, NHS-commissioned semaglutide 2.4mg (Wegovy) is limited to a maximum of 2 years through specialist weight management services, with specific BMI thresholds (including lower thresholds for some ethnic groups).
Lifestyle modifications play a crucial role. Patients who successfully implement and sustain meaningful dietary changes, regular physical activity, and behavioural strategies may have better outcomes if treatment is reduced or stopped. However, evidence suggests that maintaining weight loss without pharmacological support remains challenging for most people due to biological adaptations that defend against weight loss.
Treatment response and tolerability are key considerations. NICE guidelines for type 2 diabetes (NG28) recommend reviewing GLP-1 treatment at around 6 months and continuing only if there has been a meaningful reduction in HbA1c (typically at least 11 mmol/mol [1%]) and weight loss of at least 3% of initial body weight.
Comorbidities and cardiovascular risk also factor into decision-making. Patients with established cardiovascular disease may benefit from specific GLP-1 therapies (semaglutide, dulaglutide, or liraglutide) that have demonstrated cardiovascular risk reduction in clinical trials, though these benefits are observed during active treatment.
Patient preferences, treatment burden, and cost are legitimate considerations. GLP-1 medications require ongoing injections (except oral semaglutide) and can be expensive. Shared decision-making should balance clinical benefits against personal circumstances, quality of life, and individual treatment goals. Regular monitoring and open communication with your healthcare provider ensure treatment duration aligns with your evolving needs and follows appropriate UK clinical guidelines.
Alternatives and Long-Term Management Strategies
For those seeking to reduce reliance on GLP-1 medications or exploring complementary approaches, several evidence-based strategies exist, though none replicate the combined metabolic effects of these drugs.
Lifestyle interventions remain the foundation of long-term management for both diabetes and obesity. Structured programmes incorporating dietary modification, physical activity, and behavioural support can produce meaningful improvements. The NHS Diabetes Prevention Programme and specialist weight management services offer evidence-based support. However, realistic expectations are important—lifestyle interventions alone typically achieve 3-5% weight loss, considerably less than GLP-1 medications, and maintaining these changes long-term proves difficult for many people.
Alternative pharmacological options exist for both conditions. For type 2 diabetes, NICE-recommended alternatives include metformin (first-line), SGLT2 inhibitors, DPP-4 inhibitors, and insulin therapy, each with distinct mechanisms and side-effect profiles. For obesity, orlistat and naltrexone-bupropion (Mysimba) are available but generally less effective than GLP-1 receptor agonists. Tirzepatide (Mounjaro), a dual GIP/GLP-1 receptor agonist, has been approved for type 2 diabetes in the UK and shows even greater efficacy for both glucose control and weight loss.
Bariatric surgery represents the most effective long-term intervention for severe obesity. NICE recommends considering this for people with a BMI ≥40 kg/m² or ≥35 kg/m² with comorbidities (with lower thresholds for people from certain ethnic groups), and for people with type 2 diabetes with a BMI between 30-34.9 kg/m². Procedures such as gastric bypass or sleeve gastrectomy produce substantial, sustained weight loss and often induce diabetes remission. Referral to tier 3/4 specialist services should be considered for appropriate candidates.
Structured monitoring and support are essential regardless of treatment approach. Regular follow-up with your GP or specialist diabetes team should include:
-
HbA1c monitoring (typically every 3-6 months initially, then 6-12 monthly when stable)
-
Weight and cardiovascular risk factor tracking
-
Medication adjustment as needed
-
Early identification of complications
-
Psychological support for behaviour change
When to seek medical advice: Contact your GP if you experience unexplained weight regain, worsening diabetes symptoms (increased thirst, urination, fatigue), or wish to discuss treatment modifications. Seek urgent medical attention for severe, persistent abdominal pain. Any decision to stop or reduce GLP-1 therapy should be made collaboratively with your healthcare team, with appropriate monitoring arrangements in place to safeguard your metabolic health.
If you experience side effects from any medication, report them to the MHRA Yellow Card scheme (yellowcard.mhra.gov.uk).
Frequently Asked Questions
Can you stop taking GLP-1 medications once you reach your target weight?
Stopping GLP-1 medications typically leads to weight regain, with most people regaining 50-70% of lost weight within 12 months as appetite and metabolic adaptations return. Any decision to stop should be made with your healthcare team, with appropriate monitoring in place.
How long can you take GLP-1 medications on the NHS?
For type 2 diabetes, GLP-1 medications can be prescribed long-term if clinically appropriate. For obesity, NHS-commissioned semaglutide 2.4mg (Wegovy) through specialist weight management services is limited to a maximum of two years.
What happens to your blood sugar if you stop GLP-1 for diabetes?
HbA1c levels typically rise within months of stopping GLP-1 therapy, often returning towards pre-treatment values, as the underlying insulin resistance and beta-cell dysfunction remain. Your diabetes care team will need to adjust your treatment plan accordingly.
The health-related content published on this site is based on credible scientific sources and is periodically reviewed to ensure accuracy and relevance. Although we aim to reflect the most current medical knowledge, the material is meant for general education and awareness only.
The information on this site is not a substitute for professional medical advice. For any health concerns, please speak with a qualified medical professional. By using this information, you acknowledge responsibility for any decisions made and understand we are not liable for any consequences that may result.
Heading 1
Heading 2
Heading 3
Heading 4
Heading 5
Heading 6
Lorem ipsum dolor sit amet, consectetur adipiscing elit, sed do eiusmod tempor incididunt ut labore et dolore magna aliqua. Ut enim ad minim veniam, quis nostrud exercitation ullamco laboris nisi ut aliquip ex ea commodo consequat. Duis aute irure dolor in reprehenderit in voluptate velit esse cillum dolore eu fugiat nulla pariatur.
Block quote
Ordered list
- Item 1
- Item 2
- Item 3
Unordered list
- Item A
- Item B
- Item C
Bold text
Emphasis
Superscript
Subscript












