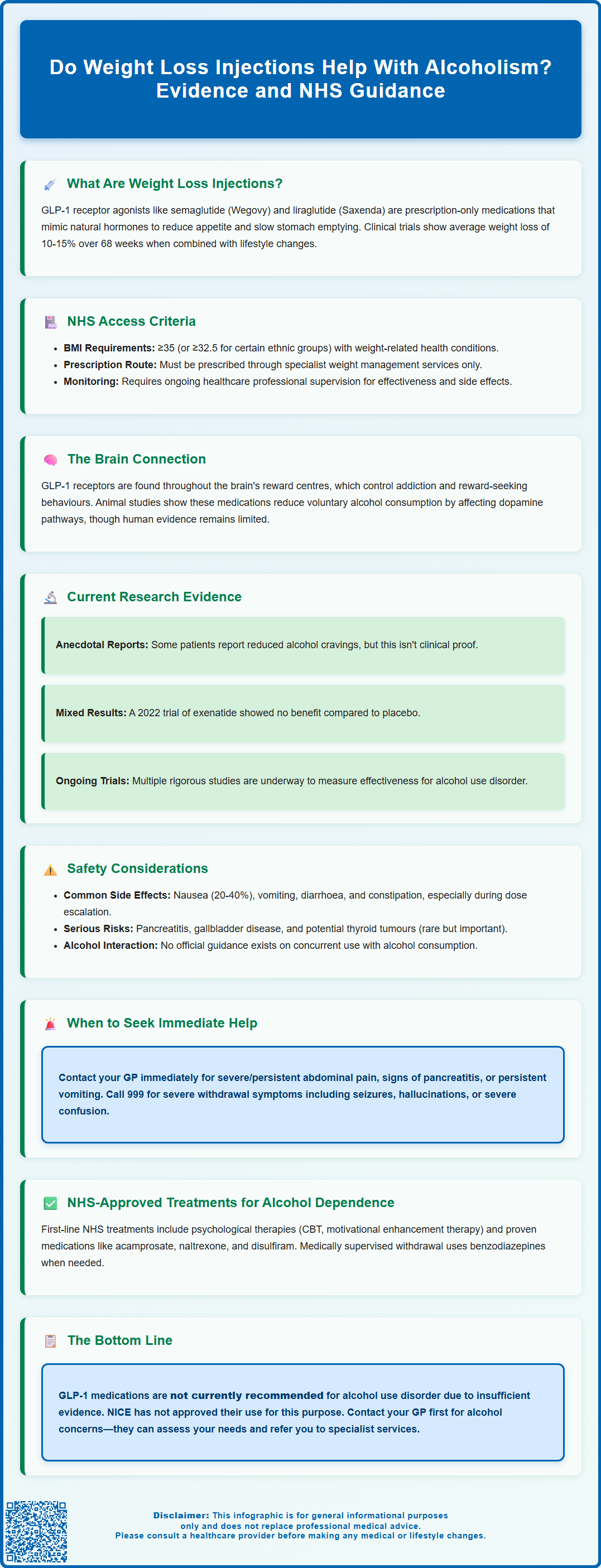
Do weight loss injections help with alcoholism? Emerging research suggests GLP-1 receptor agonists—medications licensed for obesity and type 2 diabetes—may influence alcohol consumption patterns, though this remains an off-label observation. These injectable medications, including semaglutide (Wegovy) and liraglutide (Saxenda), act on brain reward pathways that overlap with addiction circuitry. Whilst animal studies and anecdotal reports indicate reduced alcohol cravings, human clinical trials show mixed results. Importantly, GLP-1 medications are not licensed or recommended by NICE for alcohol use disorder. Current NHS guidance emphasises proven treatments including psychological therapies and medications such as acamprosate and naltrexone. This article examines the evidence, safety considerations, and established treatment pathways for alcohol dependence.
Summary: GLP-1 receptor agonists (weight loss injections) are not licensed or recommended for alcohol use disorder, though emerging research suggests they may influence alcohol consumption via brain reward pathways.
- GLP-1 medications such as semaglutide and liraglutide are licensed only for obesity management and type 2 diabetes, not alcohol use disorder.
- Animal studies show reduced alcohol intake with GLP-1 agonists, but human clinical trials have produced mixed results with no overall proven benefit.
- These medications act on brain reward circuitry involved in both appetite regulation and addiction behaviours.
- Common adverse effects include nausea, vomiting, and gastrointestinal symptoms; rare serious risks include pancreatitis and gallbladder disease.
- NICE recommends proven treatments for alcohol dependence including acamprosate, naltrexone, disulfiram, and psychological therapies such as CBT.
- Any use of GLP-1 medications for alcohol use disorder would be off-label and should occur only within clinical trials or under specialist supervision.
Table of Contents
- Understanding Weight Loss Injections and Their Mechanisms
- The Link Between GLP-1 Medications and Alcohol Consumption
- Current Research on Weight Loss Injections for Alcohol Use Disorder
- Safety Considerations and Potential Risks
- NHS Guidance and Treatment Options for Alcohol Dependence
- Frequently Asked Questions
Understanding Weight Loss Injections and Their Mechanisms
Weight loss injections, primarily glucagon-like peptide-1 (GLP-1) receptor agonists, have become increasingly prominent in obesity management. These prescription-only medications include semaglutide (marketed as Wegovy for weight management) and liraglutide (Saxenda). Ozempic (semaglutide) is licensed only for type 2 diabetes treatment, not for weight loss. The Medicines and Healthcare products Regulatory Agency (MHRA) has approved Wegovy and Saxenda specifically for weight management in adults with a body mass index (BMI) of 30 kg/m² or above, or 27 kg/m² with weight-related comorbidities.
On the NHS, access to these medications is more restricted than their marketing authorisations. NICE guidance (TA875 and TA664) specifies that they should be prescribed by specialist weight management services for people with a BMI of at least 35 kg/m² (or 32.5 kg/m² for certain ethnic groups) with at least one weight-related comorbidity, and only as part of a programme including diet and physical activity.
The mechanism of action centres on mimicking the naturally occurring GLP-1 hormone, which is released from the intestine following food intake. These injectable medications work by binding to GLP-1 receptors in multiple tissues throughout the body, including the brain, pancreas, and gastrointestinal tract. In the pancreas, they enhance glucose-dependent insulin secretion whilst suppressing glucagon release, thereby improving glycaemic control. Within the gastrointestinal system, they slow gastric emptying, which prolongs the sensation of fullness after meals.
Crucially, GLP-1 receptor agonists act on areas of the brain involved in appetite regulation, particularly the hypothalamus and brainstem. By reducing appetite and increasing satiety signals, these medications help patients consume fewer calories naturally. Clinical trials have demonstrated that semaglutide can lead to an average weight loss of 10-15% of body weight over 68 weeks when combined with lifestyle modifications. The medications are administered via subcutaneous injection, typically weekly for semaglutide or daily for liraglutide, and require ongoing monitoring by healthcare professionals to assess efficacy and manage potential adverse effects.
The Link Between GLP-1 Medications and Alcohol Consumption
Emerging evidence suggests that GLP-1 receptor agonists may influence alcohol consumption patterns, though this represents an off-label observation rather than an approved indication. GLP-1 medications are not licensed for alcohol use disorder (AUD) and are not recommended by NICE for this purpose; any such use would be off-label and generally should be limited to clinical trials.
The potential connection stems from the widespread distribution of GLP-1 receptors throughout the brain's reward circuitry, including regions such as the nucleus accumbens, ventral tegmental area, and prefrontal cortex—areas fundamentally involved in addiction and reward-seeking behaviours.
Preclinical studies in animal models have demonstrated that GLP-1 receptor activation can reduce alcohol intake and preference. Rodents treated with GLP-1 agonists showed decreased voluntary alcohol consumption and reduced motivation to seek alcohol rewards. These findings suggest that the medications may modulate the dopaminergic reward pathways that underpin both food intake and substance use behaviours. The neurobiological overlap between appetite regulation and addiction has prompted researchers to investigate whether medications designed for metabolic conditions might have broader applications in addiction medicine.
Anecdotal reports from patients prescribed GLP-1 medications for weight management or diabetes have included observations of reduced alcohol cravings and decreased consumption. Some individuals have reported finding alcohol less appealing or experiencing reduced desire to drink whilst taking these medications. However, human data remain limited and mixed, with some clinical trials showing no overall benefit. It is essential to emphasise that these medications are not licensed for treating alcohol use disorder, and any such use would require careful clinical justification and informed patient consent.
Current Research on Weight Loss Injections for Alcohol Use Disorder
The scientific investigation into GLP-1 medications for alcohol use disorder remains in relatively early stages, with evidence showing mixed results. Some observational studies have suggested potential benefits. For example, analyses of electronic health records have found associations between GLP-1 receptor agonist use and lower rates of alcohol-related hospital encounters compared to other weight loss medications. However, such observational data cannot establish causation and are subject to various confounding factors.
Controlled clinical trials have produced variable results. A randomised controlled trial of exenatide (another GLP-1 receptor agonist) published in 2022 showed no overall benefit for alcohol use disorder compared to placebo, highlighting the need for caution in interpreting preliminary findings. Several prospective clinical trials are currently underway to more rigorously evaluate the efficacy of semaglutide and other GLP-1 agonists in reducing alcohol consumption among individuals with alcohol use disorder. These studies employ randomised, placebo-controlled designs—the gold standard for establishing treatment efficacy. Researchers are measuring outcomes including total alcohol consumption, heavy drinking days, alcohol craving scores, and relapse rates.
The evidence base remains insufficient to support routine clinical use for alcohol dependence. The National Institute for Health and Care Excellence (NICE) has not issued guidance recommending GLP-1 medications for alcohol use disorder, as the quality and quantity of evidence do not yet meet thresholds for clinical recommendations. Important questions remain unanswered, including optimal dosing regimens, which patient populations might benefit most, long-term efficacy, and whether effects persist after medication discontinuation. Additionally, most studies have focused on individuals with co-occurring obesity or diabetes, limiting generalisability to the broader population with alcohol use disorder.
Participation in properly designed clinical trials currently represents the most appropriate way to investigate these medications for alcohol use disorder.
Safety Considerations and Potential Risks
Whilst GLP-1 receptor agonists have established safety profiles for their licensed indications, several important considerations arise when contemplating their use in individuals with alcohol use disorder. Common adverse effects include gastrointestinal symptoms such as nausea (affecting 20-40% of patients), vomiting, diarrhoea, constipation, and abdominal discomfort. These effects are typically most pronounced during dose escalation and may diminish over time, though they can be severe enough to necessitate treatment discontinuation in approximately 5-10% of patients. Gradual dose escalation as per the SmPC can help mitigate these effects.
More serious but rare adverse effects include pancreatitis, with patients advised to seek immediate medical attention if experiencing severe, persistent abdominal pain radiating to the back. Treatment should be discontinued if pancreatitis is suspected. Gallbladder disease, including cholelithiasis and cholecystitis, occurs with increased frequency, likely related to rapid weight loss.
Animal studies have shown thyroid C-cell tumours with GLP-1 receptor agonists, though the human relevance is unknown. Patients should seek medical review if they develop symptoms such as a lump in the neck, persistent hoarseness, or difficulty swallowing.
Additional safety considerations include: risk of diabetic retinopathy complications in people with diabetes (particularly with semaglutide); increased risk of hypoglycaemia when used with insulin or sulfonylureas; and potential for dehydration and acute kidney injury with severe gastrointestinal side effects. These medications are not recommended during pregnancy or breastfeeding.
For individuals with alcohol use disorder, additional safety concerns warrant consideration. Alcohol itself can cause gastritis and gastrointestinal irritation, potentially compounding the gastrointestinal side effects of GLP-1 medications. Patients with alcohol-related liver disease require careful assessment, though UK SmPCs indicate no clinically relevant effect in mild to moderate hepatic impairment (data in severe impairment are limited). Furthermore, the combination of alcohol and these medications has not been extensively studied, and there is no official guidance on their concurrent use.
Patients should contact their GP immediately if they experience: severe or persistent abdominal pain, signs of pancreatitis, unexplained weight loss beyond expected parameters, persistent vomiting leading to dehydration, or any concerning symptoms. Regular monitoring of renal function, particularly in patients at risk of dehydration, is advisable. Patients should report suspected side effects via the MHRA Yellow Card scheme (yellowcard.mhra.gov.uk). It is crucial that any use of GLP-1 medications in the context of alcohol use disorder occurs only under specialist supervision with comprehensive informed consent.
NHS Guidance and Treatment Options for Alcohol Dependence
The NHS provides comprehensive, evidence-based treatment pathways for alcohol dependence, as outlined in NICE guideline CG115 (Alcohol-use disorders: diagnosis, assessment and management of harmful drinking and alcohol dependence). Current recommended approaches include psychological interventions, pharmacological treatments with established efficacy, and structured support programmes. GLP-1 receptor agonists do not feature in these guidelines, as the evidence base remains insufficient for clinical recommendation.
First-line psychological interventions include cognitive behavioural therapy (CBT), motivational enhancement therapy, and behavioural couples therapy for those in relationships. These approaches address the psychological drivers of alcohol use and develop coping strategies. For individuals with moderate to severe alcohol dependence, NICE recommends considering pharmacological treatments including acamprosate (which modulates glutamate neurotransmission to reduce cravings), naltrexone (an opioid antagonist that reduces the rewarding effects of alcohol), and disulfiram (which causes unpleasant reactions when alcohol is consumed, acting as a deterrent). For people who are drinking at high-risk levels but are not physically dependent on alcohol, nalmefene may be considered to help reduce alcohol consumption, as recommended in NICE TA325.
Patients requiring medically assisted alcohol withdrawal should be assessed for community or inpatient detoxification, typically using benzodiazepines such as chlordiazepoxide under close medical supervision. The NHS also provides access to specialist alcohol services, including community alcohol teams, residential rehabilitation programmes, and mutual aid groups such as Alcoholics Anonymous.
Urgent medical attention is required for anyone experiencing severe alcohol withdrawal symptoms such as seizures, hallucinations, severe confusion, or suspected Wernicke's encephalopathy. These are medical emergencies requiring immediate assessment via 999 or A&E attendance.
Individuals concerned about their alcohol consumption should contact their GP as the first point of access to these services. GPs can conduct initial assessments using validated tools such as the AUDIT (Alcohol Use Disorders Identification Test), provide brief interventions for hazardous drinking, and refer to specialist services when appropriate. For immediate support, the NHS recommends contacting local alcohol services directly or calling the national Drinkline helpline (0300 123 1110) for confidential advice. Additional resources are available on the NHS alcohol support webpage. Whilst research into novel treatments including GLP-1 medications continues, patients should access proven, guideline-recommended interventions that offer the best current evidence for recovery from alcohol dependence.
Frequently Asked Questions
Are GLP-1 weight loss injections approved for treating alcohol use disorder?
No, GLP-1 receptor agonists such as semaglutide and liraglutide are not licensed or recommended by NICE for alcohol use disorder. They are approved only for obesity management and type 2 diabetes treatment.
What does current research show about GLP-1 medications and alcohol consumption?
Research shows mixed results. Animal studies suggest reduced alcohol intake, and some observational data indicate potential benefits, but randomised controlled trials in humans have not demonstrated overall efficacy for alcohol use disorder.
What are the NHS-recommended treatments for alcohol dependence?
NICE recommends psychological interventions such as cognitive behavioural therapy, and pharmacological treatments including acamprosate, naltrexone, and disulfiram. Patients should contact their GP for assessment and referral to specialist alcohol services.
The health-related content published on this site is based on credible scientific sources and is periodically reviewed to ensure accuracy and relevance. Although we aim to reflect the most current medical knowledge, the material is meant for general education and awareness only.
The information on this site is not a substitute for professional medical advice. For any health concerns, please speak with a qualified medical professional. By using this information, you acknowledge responsibility for any decisions made and understand we are not liable for any consequences that may result.
Heading 1
Heading 2
Heading 3
Heading 4
Heading 5
Heading 6
Lorem ipsum dolor sit amet, consectetur adipiscing elit, sed do eiusmod tempor incididunt ut labore et dolore magna aliqua. Ut enim ad minim veniam, quis nostrud exercitation ullamco laboris nisi ut aliquip ex ea commodo consequat. Duis aute irure dolor in reprehenderit in voluptate velit esse cillum dolore eu fugiat nulla pariatur.
Block quote
Ordered list
- Item 1
- Item 2
- Item 3
Unordered list
- Item A
- Item B
- Item C
Bold text
Emphasis
Superscript
Subscript