Many people using Saxenda (liraglutide) for weight management experience constipation as a side effect. This raises an important question about whether laxatives can be safely used alongside this GLP-1 receptor agonist medication. Understanding the interaction between Saxenda and laxatives is essential for managing digestive symptoms effectively whilst maintaining treatment safety. This article examines the compatibility of laxatives with Saxenda, explores practical strategies for managing constipation, and provides guidance on when to seek medical advice, all aligned with current UK clinical guidance from NICE, the MHRA, and the BNF.
Summary: Laxatives are generally safe to take with Saxenda, though you should consult your GP or prescribing clinician before starting any laxative treatment.
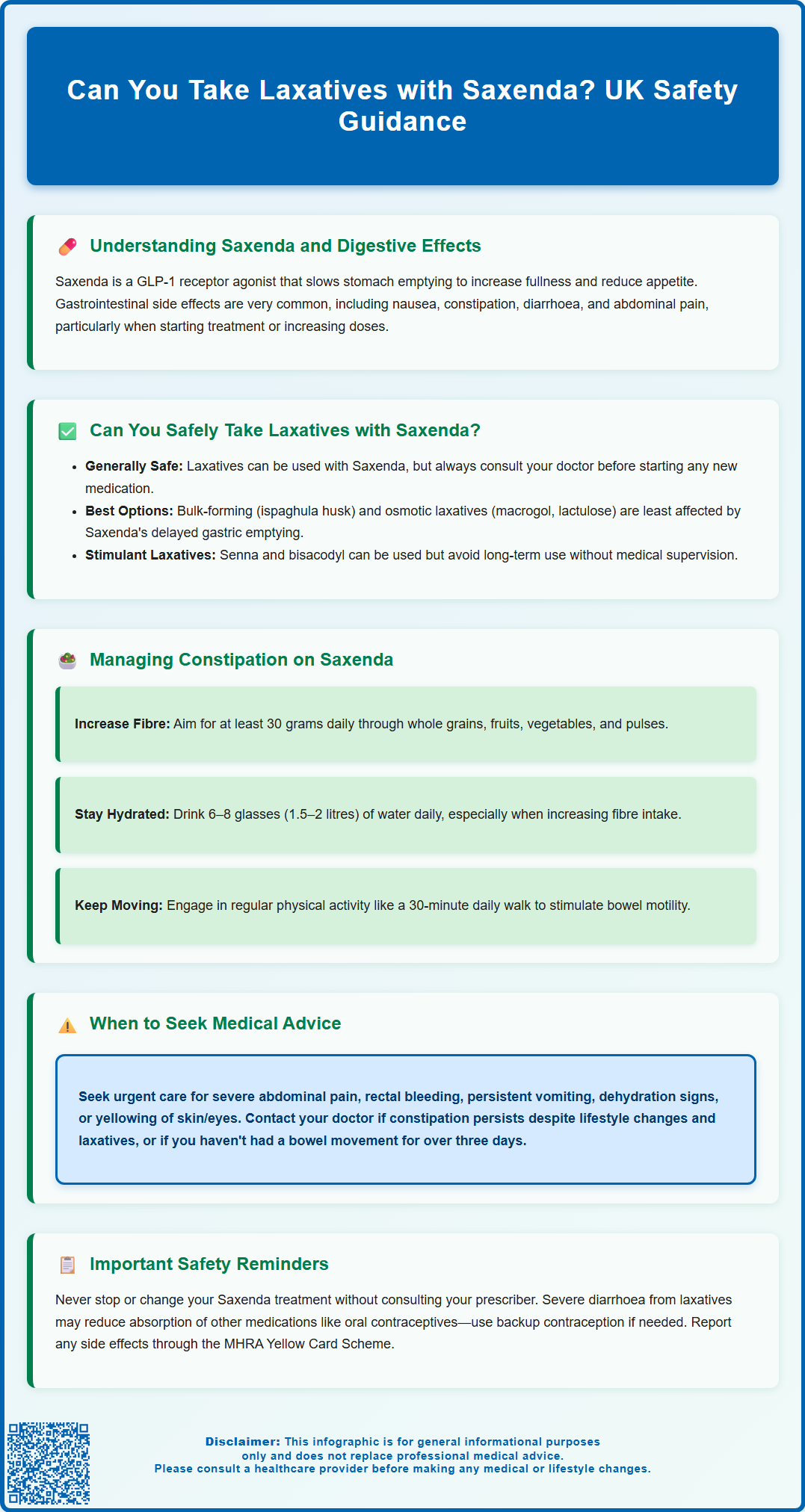
- Saxenda (liraglutide) is a GLP-1 receptor agonist that slows gastric emptying, commonly causing constipation in up to 1 in 10 users.
- Bulk-forming and osmotic laxatives work locally in the bowel and are unlikely to be affected by Saxenda's delayed gastric emptying mechanism.
- Lifestyle modifications including increased dietary fibre (30g daily), adequate hydration (1.5–2 litres), and regular physical activity should be first-line management for constipation.
- Seek urgent medical advice for severe abdominal pain, blood in stools, persistent vomiting, or right upper abdominal pain, which may indicate serious complications such as pancreatitis or gallbladder disease.
Table of Contents
Understanding Saxenda and Its Gastrointestinal Effects
Saxenda (liraglutide 3 mg) is a prescription medicine licensed in the UK for weight management in adults with obesity or overweight with weight-related health conditions. It belongs to a class of medications called glucagon-like peptide-1 (GLP-1) receptor agonists, which work by mimicking a naturally occurring hormone that regulates appetite and food intake.
The mechanism of action of Saxenda involves slowing gastric emptying, which means food moves more slowly from the stomach into the small intestine. This delayed gastric emptying contributes to increased feelings of fullness and reduced appetite, supporting weight loss efforts. This mechanism can also contribute to various digestive side effects.
Gastrointestinal adverse effects are among the most commonly reported with Saxenda use. According to the MHRA/EMC Summary of Product Characteristics, these include nausea, vomiting, diarrhoea, constipation, dyspepsia, and abdominal pain. Nausea is particularly common, especially when starting treatment or increasing the dose, though it typically improves over time as the body adjusts to the medication.
Constipation is classified as a 'common' side effect of Saxenda, affecting up to 1 in 10 users in clinical trials. The slowed movement of food through the digestive system can reduce bowel frequency and make stools harder to pass.
It's also important to be aware that liraglutide has been associated with rare but serious conditions including pancreatitis and gallbladder disease (such as gallstones). Understanding these gastrointestinal effects is essential for patients and healthcare professionals when considering how to manage digestive symptoms that may arise during Saxenda treatment, including whether additional interventions such as laxatives might be appropriate.
Can You Safely Take Laxatives with Saxenda?
Laxatives are generally compatible with Saxenda, and many patients may safely use over-the-counter laxatives to manage constipation. However, several important considerations should guide this decision, and it is always advisable to consult with your GP or prescribing clinician before starting any new medication, including laxatives.
According to the Saxenda SmPC, while liraglutide delays gastric emptying, this has minimal clinically relevant effects on the absorption of most oral medicines. For most laxatives, this is unlikely to pose significant problems, but the timing and type of laxative may matter. Bulk-forming laxatives (such as ispaghula husk or methylcellulose) and osmotic laxatives (like lactulose or macrogol) generally work locally in the bowel and are less likely to be affected by delayed gastric emptying. When using bulk-forming laxatives, ensure you drink plenty of fluids to prevent intestinal obstruction.
Stimulant laxatives (such as senna or bisacodyl) are also commonly used and can be taken with Saxenda, though patients should be aware that combining medications that both affect bowel motility requires monitoring. Avoid excessive or long-term use of stimulant laxatives without medical review.
If you experience severe diarrhoea from laxative use whilst on Saxenda, this could potentially affect the absorption of other important medications you may be taking. This includes oral contraceptives – if you experience severe diarrhoea, follow the 'missed pill' guidance in the patient information leaflet and consider additional contraceptive precautions as advised by the Faculty of Sexual and Reproductive Healthcare (FSRH).
The British National Formulary (BNF) does not list specific interactions between Saxenda and commonly used laxatives. However, individual responses can vary, and what works well for one person may cause problems for another. Starting with the lowest effective dose of laxative and monitoring your response is a sensible approach. If you have any underlying bowel conditions, such as inflammatory bowel disease or irritable bowel syndrome, discussing laxative use with your healthcare provider becomes even more important.
Managing Constipation While Using Saxenda
Lifestyle and dietary modifications should always be the first-line approach to managing constipation whilst taking Saxenda, before considering laxative use. These non-pharmacological strategies are safe, effective, and align with NICE Clinical Knowledge Summary (CKS) guidance on managing constipation in adults.
Increasing dietary fibre intake is fundamental to promoting regular bowel movements. Aim for at least 30 grams of fibre daily through:
-
Whole grain cereals, bread, and pasta
-
Fresh fruits and vegetables (with skins where appropriate)
-
Pulses, beans, and lentils
-
Nuts and seeds
Adequate hydration is equally crucial, particularly when increasing fibre intake. Adults should aim for 6–8 glasses (approximately 1.5–2 litres) of fluid daily. Water is ideal, though other sugar-free drinks also contribute. Proper hydration helps soften stools and supports the action of dietary fibre.
Regular physical activity stimulates bowel motility and can help prevent constipation. Even moderate exercise, such as a 30-minute daily walk, can make a significant difference. This has the added benefit of supporting your weight management goals whilst using Saxenda.
If lifestyle measures prove insufficient, over-the-counter laxatives can be introduced gradually. Bulk-forming laxatives are often recommended as a first step, as they work naturally by increasing stool volume. If these are ineffective after several days, osmotic laxatives like macrogol (polyethylene glycol) may be tried. Stimulant laxatives should generally be reserved for short-term use when other options have failed.
Establishing a regular toilet routine can also help. Try to allow sufficient time after meals, when the gastrocolic reflex naturally stimulates bowel activity. Never ignore the urge to open your bowels, as delaying can worsen constipation.
According to the Saxenda SmPC, slower dose escalation or temporary delay in up-titration can help mitigate gastrointestinal side effects. Saxenda can be administered at any time of day, independent of meals, as per the product guidance.
When to Seek Medical Advice About Bowel Changes on Saxenda
Whilst mild constipation can often be managed with lifestyle changes and over-the-counter remedies, certain symptoms warrant prompt medical attention. Understanding when to contact your GP or healthcare provider is essential for patient safety.
Seek medical advice urgently if you experience:
-
Severe abdominal pain, particularly if persistent or radiating to your back (which could indicate pancreatitis)
-
Blood in your stools or rectal bleeding
-
Unexplained weight loss beyond your expected Saxenda-related weight reduction
-
Persistent nausea and vomiting that prevents you from eating or drinking
-
Signs of dehydration (dark urine, dizziness, extreme thirst)
-
Severe or persistent diarrhoea
-
Right upper abdominal pain, fever or yellowing of the skin/eyes (which could indicate gallbladder problems)
You should also contact your GP or prescribing clinician if:
-
Constipation persists despite lifestyle modifications and appropriate laxative use
-
You have not had a bowel movement for more than three days despite using laxatives
-
You develop new or worsening gastrointestinal symptoms after several weeks on a stable Saxenda dose
-
You're unsure whether your symptoms are related to Saxenda or might indicate another condition
-
You need to use laxatives regularly for more than a week or two
It is important to remember that severe or persistent gastrointestinal symptoms may require dose adjustment or, in some cases, discontinuation of Saxenda. Your healthcare provider can assess whether your symptoms are within the expected range of side effects or whether further investigation is needed.
NICE guidance recommends that Saxenda should be discontinued if you have not lost at least 5% of your initial body weight after 12 weeks on the full 3 mg daily dose. Regular follow-up appointments within a weight management service are essential to monitor both efficacy and tolerability.
If you experience severe adverse effects, you may need to stop taking Saxenda and seek urgent medical advice. Otherwise, consult your prescriber before making any changes to your treatment. If you have concerns about any aspect of your treatment, including bowel changes or laxative use, your healthcare team is there to support you in achieving safe and effective weight management.
If you suspect you're experiencing side effects from Saxenda, you can report these through the MHRA Yellow Card Scheme, which helps monitor the safety of medicines in the UK.
Scientific References
- Saxenda 6 mg/mL solution for injection in pre-filled pen - Summary of Product Characteristics.
- Saxenda - European Public Assessment Report (EPAR).
- Liraglutide for managing overweight and obesity (TA664).
- GLP-1 receptor agonists: reminder of the potential side effects and to be aware of the potential for misuse.
- GLP-1 medicines for weight loss and diabetes: what you need to know.
Frequently Asked Questions
Which type of laxative is safest to use with Saxenda?
Bulk-forming laxatives (such as ispaghula husk) and osmotic laxatives (like macrogol) are generally safest as they work locally in the bowel and are less affected by Saxenda's delayed gastric emptying. Always ensure adequate fluid intake when using bulk-forming laxatives.
How long does constipation from Saxenda typically last?
Constipation from Saxenda is most common when starting treatment or increasing the dose, and typically improves as your body adjusts to the medication. If constipation persists despite lifestyle modifications and laxative use, contact your GP or prescribing clinician.
Should I stop taking Saxenda if I experience severe constipation?
Do not stop Saxenda without consulting your prescriber. Mild to moderate constipation can usually be managed with lifestyle changes and appropriate laxatives, but persistent or severe symptoms may require dose adjustment or medical review to rule out other complications.
The health-related content published on this site is based on credible scientific sources and is periodically reviewed to ensure accuracy and relevance. Although we aim to reflect the most current medical knowledge, the material is meant for general education and awareness only.
The information on this site is not a substitute for professional medical advice. For any health concerns, please speak with a qualified medical professional. By using this information, you acknowledge responsibility for any decisions made and understand we are not liable for any consequences that may result.
Heading 1
Heading 2
Heading 3
Heading 4
Heading 5
Heading 6
Lorem ipsum dolor sit amet, consectetur adipiscing elit, sed do eiusmod tempor incididunt ut labore et dolore magna aliqua. Ut enim ad minim veniam, quis nostrud exercitation ullamco laboris nisi ut aliquip ex ea commodo consequat. Duis aute irure dolor in reprehenderit in voluptate velit esse cillum dolore eu fugiat nulla pariatur.
Block quote
Ordered list
- Item 1
- Item 2
- Item 3
Unordered list
- Item A
- Item B
- Item C
Bold text
Emphasis
Superscript
Subscript