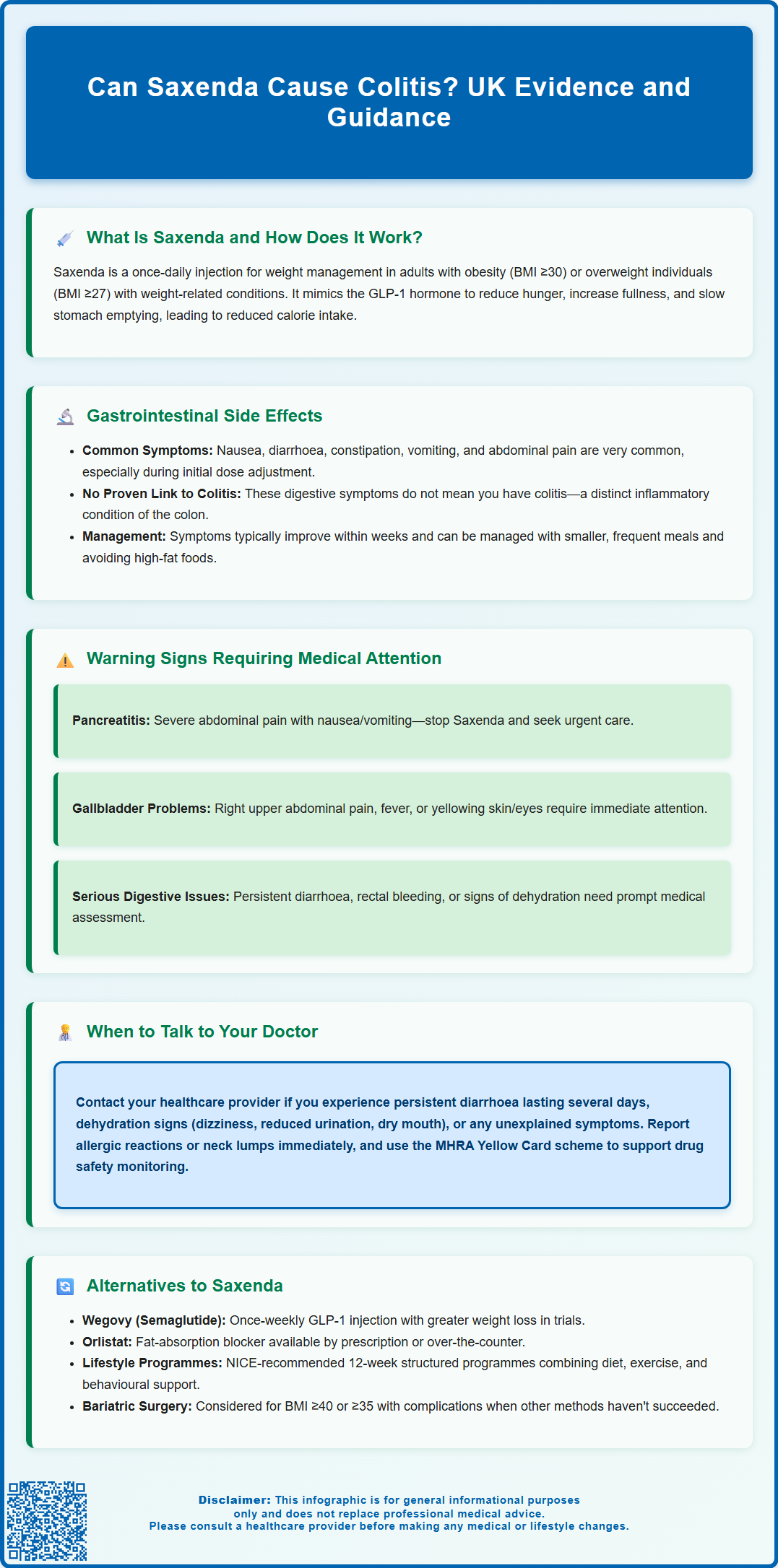
Can Saxenda cause colitis? This is an important question for patients considering or currently using this GLP-1 receptor agonist for weight management. Saxenda (liraglutide 3.0 mg) is a prescription medicine licensed in the UK for obesity treatment, administered as a daily subcutaneous injection alongside lifestyle modifications. Whilst gastrointestinal side effects such as nausea, diarrhoea, and abdominal discomfort are commonly reported with Saxenda, there is currently no established causal link between the medication and colitis—a distinct inflammatory condition of the colon. Understanding the difference between common gastrointestinal symptoms and true colitis is essential for safe and effective treatment. This article examines the evidence, explores when symptoms warrant medical review, and discusses alternative weight management options available in the UK.
Summary: There is currently no established causal link between Saxenda (liraglutide) and the development of colitis.
- Saxenda is a GLP-1 receptor agonist licensed in the UK for weight management in adults and adolescents with obesity or overweight with comorbidities.
- Common gastrointestinal side effects include nausea, diarrhoea, constipation, and abdominal pain, particularly during initial dose titration.
- These symptoms result from slowed gastric emptying and altered gut motility, not inflammatory colitis.
- Persistent diarrhoea, rectal bleeding, or severe abdominal pain should prompt medical evaluation to exclude other gastrointestinal pathology.
- Saxenda carries an increased risk of gallbladder disorders and rare but serious pancreatitis, requiring monitoring and patient counselling.
- Treatment should be discontinued after 12 weeks at maintenance dose if less than 5% initial body weight has been lost.
Table of Contents
What Is Saxenda and How Does It Work?
Saxenda (liraglutide 3.0 mg) is a prescription medicine licensed in the UK for weight management in adults with obesity (BMI ≥30 kg/m²) or those who are overweight (BMI ≥27 kg/m²) with at least one weight-related comorbidity, such as type 2 diabetes, hypertension, or dyslipidaemia. It is also licensed for weight management in adolescents aged 12 years and above with obesity. Saxenda is administered as a once-daily subcutaneous injection and is intended to be used alongside a reduced-calorie diet and increased physical activity.
Liraglutide belongs to a class of medications known as glucagon-like peptide-1 (GLP-1) receptor agonists. It works by mimicking the action of the naturally occurring hormone GLP-1, which is released from the intestine in response to food intake. By activating GLP-1 receptors in the brain, particularly in areas that regulate appetite, Saxenda helps to reduce hunger and increase feelings of fullness. This mechanism leads to a reduction in calorie intake and, consequently, weight loss over time.
Additionally, liraglutide slows gastric emptying, meaning food remains in the stomach for longer, which further contributes to satiety. It also has glucose-dependent effects on insulin secretion and glucagon suppression at the 3.0 mg dose used for weight management. The Medicines and Healthcare products Regulatory Agency (MHRA) and the European Medicines Agency (EMA) have approved Saxenda based on clinical trial evidence demonstrating meaningful weight loss when combined with lifestyle interventions.
Saxenda is started at a low dose (0.6 mg daily) and gradually increased weekly to minimise gastrointestinal side effects, reaching the full 3.0 mg maintenance dose after 4-5 weeks. Treatment should be discontinued after 12 weeks at the 3.0 mg dose if weight loss of at least 5% of initial body weight has not been achieved.
It is important to note that Saxenda should not be used during pregnancy, and should be discontinued if pregnancy occurs. Caution is advised in patients with a history of pancreatitis, gallbladder disease, or severe gastrointestinal disorders such as gastroparesis. A thorough medical assessment by a healthcare professional is essential before starting treatment.
Gastrointestinal Side Effects of Saxenda
Gastrointestinal adverse effects are among the most commonly reported side effects associated with Saxenda. Clinical trials and post-marketing surveillance data indicate that nausea, diarrhoea, constipation, vomiting, dyspepsia, and abdominal pain occur frequently, particularly during the initial titration phase. These symptoms are generally mild to moderate in severity and tend to diminish as the body adjusts to the medication over several weeks.
The mechanism underlying these gastrointestinal effects is related to liraglutide's action on GLP-1 receptors in the gut. By slowing gastric emptying and altering gut motility, the medication can cause temporary disruption to normal digestive processes. Most patients experience these symptoms transiently, and they can often be managed with dietary modifications, such as eating smaller, more frequent meals and avoiding high-fat foods.
Regarding colitis specifically, there is currently no established causal link between Saxenda and the development of colitis (inflammation of the colon). Colitis encompasses a range of conditions, including ulcerative colitis, Crohn's disease affecting the colon, infectious colitis, and ischaemic colitis. While gastrointestinal symptoms such as diarrhoea and abdominal pain are common with Saxenda, these do not equate to colitis, which is a distinct inflammatory condition. In UK primary care, suspected colitis is typically initially investigated with faecal calprotectin testing and stool cultures before considering colonoscopy and biopsy.
That said, any new or worsening gastrointestinal symptoms—particularly persistent diarrhoea, rectal bleeding, severe abdominal pain, or unexplained weight loss beyond expected therapeutic effect—should prompt medical evaluation. Prolonged vomiting or diarrhoea can lead to dehydration and potentially acute kidney injury, so maintaining adequate fluid intake is important.
Saxenda is also associated with an increased risk of gallbladder disorders, including gallstones and cholecystitis. Symptoms such as right upper quadrant pain, fever, or jaundice should be promptly reported to a healthcare professional.
If a patient has pre-existing inflammatory bowel disease (IBD), careful monitoring is advisable, although there is no official contraindication to Saxenda use in this population. Healthcare professionals should assess each case individually, considering the patient's overall gastrointestinal health and symptom profile.
When to Seek Medical Advice While Taking Saxenda
While many side effects of Saxenda are mild and self-limiting, certain symptoms warrant prompt medical attention. Patients should be counselled on recognising warning signs that may indicate serious complications or conditions requiring further investigation.
Seek urgent medical advice if you experience:
-
Severe or persistent abdominal pain, especially if accompanied by nausea and vomiting, as this may indicate pancreatitis—a rare but serious adverse effect associated with GLP-1 receptor agonists. Pancreatitis typically presents with intense, constant pain in the upper abdomen that may radiate to the back. If pancreatitis is suspected, stop taking Saxenda and seek urgent medical attention.
-
Right upper quadrant pain, fever, or yellowing of the skin or eyes, which could indicate gallbladder problems such as gallstones or inflammation of the gallbladder (cholecystitis).
-
Rectal bleeding or blood in stools, which could suggest gastrointestinal inflammation, ulceration, or other pathology unrelated to Saxenda but requiring investigation.
-
Persistent diarrhoea lasting more than a few days, particularly if associated with dehydration (dizziness, reduced urine output, dry mouth), as this may require rehydration therapy and assessment for alternative causes.
-
Signs of an allergic reaction, including rash, itching, swelling of the face or throat, difficulty breathing, or rapid heartbeat.
-
Symptoms such as a lump in the neck, hoarseness, difficulty swallowing, or shortness of breath. While a causal relationship with thyroid tumours in humans has not been established, these symptoms should be evaluated.
Patients with pre-existing gastrointestinal conditions should maintain regular contact with their GP or specialist, particularly if symptoms change or worsen. According to NICE guidance on obesity management, ongoing monitoring and support are essential components of pharmacological weight management interventions.
It is also important to report any unexplained symptoms to your healthcare professional, even if they seem unrelated to Saxenda. The MHRA's Yellow Card scheme allows patients and healthcare professionals to report suspected side effects, contributing to ongoing drug safety surveillance. Do not discontinue Saxenda without consulting your healthcare professional, as they can advise on appropriate dose adjustment or alternative management strategies.
Alternatives to Saxenda for Weight Management
For individuals who cannot tolerate Saxenda or for whom it is contraindicated, several alternative approaches to weight management are available, both pharmacological and non-pharmacological. The choice of intervention should be individualised based on clinical assessment, patient preference, comorbidities, and previous treatment responses.
Pharmacological alternatives licensed in the UK include:
-
Orlistat (Xenical, Alli): A lipase inhibitor that reduces fat absorption from the diet. It is available on prescription and over-the-counter at lower doses. Common side effects include gastrointestinal symptoms such as oily stools and faecal urgency, particularly if dietary fat intake is high.
-
Wegovy (semaglutide 2.4 mg): Another GLP-1 receptor agonist, structurally similar to liraglutide but with once-weekly dosing. It has demonstrated greater weight loss efficacy in clinical trials compared to Saxenda, as recognised in NICE technology appraisal guidance (TA875). However, it shares a similar side effect profile, including gastrointestinal symptoms.
-
Tirzepatide: A dual GIP/GLP-1 receptor agonist that has shown substantial weight loss in clinical studies. Availability and specific brand names for weight management in the UK should be confirmed with current MHRA authorisation information.
Non-pharmacological interventions remain the cornerstone of weight management and are recommended by NICE for all patients, regardless of whether medication is used:
-
Structured lifestyle programmes: Multicomponent interventions incorporating dietary advice, physical activity, and behavioural support. NICE recommends programmes lasting at least 12 weeks.
-
Psychological support: Cognitive behavioural therapy (CBT) and other psychological interventions can address emotional eating, body image concerns, and motivation.
-
Bariatric surgery: For individuals with BMI ≥40 kg/m² (or ≥35 kg/m² with comorbidities) who have not achieved adequate weight loss with non-surgical methods, procedures such as gastric bypass or sleeve gastrectomy may be considered. NICE guidance includes specific considerations for people with recent-onset type 2 diabetes and ethnicity-related BMI adjustments.
Your GP or specialist weight management service can provide tailored advice on the most appropriate options based on your individual circumstances, medical history, and treatment goals. All pharmacological treatments require ongoing lifestyle support and monitoring in line with NICE guidance.
Frequently Asked Questions
What are the most common gastrointestinal side effects of Saxenda?
The most common gastrointestinal side effects of Saxenda include nausea, diarrhoea, constipation, vomiting, dyspepsia, and abdominal pain. These symptoms are usually mild to moderate, occur particularly during the initial dose titration phase, and typically diminish as the body adjusts to the medication over several weeks.
When should I seek medical advice whilst taking Saxenda?
Seek urgent medical advice if you experience severe or persistent abdominal pain (which may indicate pancreatitis), rectal bleeding, right upper quadrant pain with fever or jaundice (suggesting gallbladder problems), persistent diarrhoea with dehydration, or signs of an allergic reaction. Any unexplained or worsening symptoms should be reported to your healthcare professional.
What are the alternatives to Saxenda for weight management in the UK?
UK-licensed pharmacological alternatives include orlistat (a lipase inhibitor), Wegovy (semaglutide, a once-weekly GLP-1 receptor agonist), and tirzepatide (a dual GIP/GLP-1 receptor agonist). Non-pharmacological options include structured lifestyle programmes, psychological support such as CBT, and bariatric surgery for eligible patients, all recommended by NICE guidance.
The health-related content published on this site is based on credible scientific sources and is periodically reviewed to ensure accuracy and relevance. Although we aim to reflect the most current medical knowledge, the material is meant for general education and awareness only.
The information on this site is not a substitute for professional medical advice. For any health concerns, please speak with a qualified medical professional. By using this information, you acknowledge responsibility for any decisions made and understand we are not liable for any consequences that may result.
Heading 1
Heading 2
Heading 3
Heading 4
Heading 5
Heading 6
Lorem ipsum dolor sit amet, consectetur adipiscing elit, sed do eiusmod tempor incididunt ut labore et dolore magna aliqua. Ut enim ad minim veniam, quis nostrud exercitation ullamco laboris nisi ut aliquip ex ea commodo consequat. Duis aute irure dolor in reprehenderit in voluptate velit esse cillum dolore eu fugiat nulla pariatur.
Block quote
Ordered list
- Item 1
- Item 2
- Item 3
Unordered list
- Item A
- Item B
- Item C
Bold text
Emphasis
Superscript
Subscript