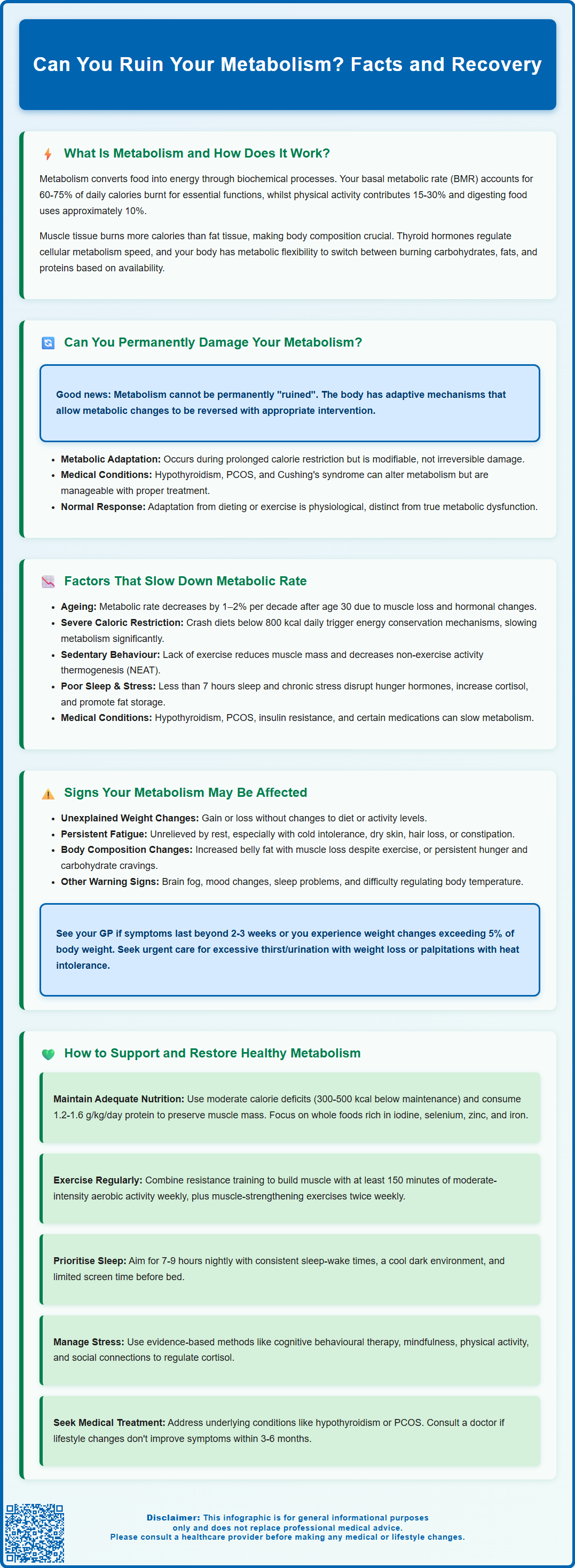
Many people worry about whether dieting, ageing, or lifestyle factors can permanently 'ruin' their metabolism. Whilst metabolic rate can certainly be influenced by caloric restriction, inactivity, medical conditions, and natural ageing, the concept of irreversible metabolic damage is largely a misconception. The human body possesses remarkable adaptive mechanisms that allow metabolism to adjust and, in most cases, recover with appropriate intervention. Understanding how metabolism works, what factors genuinely affect it, and evidence-based strategies to support metabolic health can help dispel common myths and guide effective approaches to maintaining a healthy metabolic rate throughout life.
Summary: You cannot permanently ruin your metabolism through dieting or lifestyle factors, though metabolic rate can adapt and slow temporarily in response to prolonged caloric restriction, inactivity, or medical conditions.
- Metabolic adaptation is a normal, reversible physiological response to energy restriction, not permanent damage.
- Basal metabolic rate accounts for 60–75% of daily energy expenditure and is influenced by muscle mass, age, sex, and thyroid hormones.
- Hypothyroidism and other endocrine disorders can significantly reduce metabolic rate but are treatable with appropriate medical intervention.
- Severe caloric restriction, sedentary behaviour, sleep deprivation, and chronic stress can temporarily slow metabolism through hormonal and physiological mechanisms.
- Contact your GP if you experience unexplained weight changes, persistent fatigue, or symptoms affecting daily function for medical assessment including thyroid function tests.
Table of Contents
What Is Metabolism and How Does It Work?
Metabolism refers to the complex network of biochemical processes that convert food and drink into energy to sustain life. This encompasses all chemical reactions occurring within cells, including breaking down nutrients (catabolism) and building cellular components (anabolism). Your metabolic rate determines how many calories your body burns at rest and during activity.
The largest component of metabolism is basal metabolic rate (BMR), which typically accounts for approximately 60–75% of total daily energy expenditure, though this varies between individuals based on activity levels. BMR represents the energy required for essential functions such as breathing, circulation, cell production, and maintaining body temperature. In practice, resting metabolic rate (RMR) is more commonly measured, which is slightly higher than BMR as it doesn't require the same fasting and complete rest conditions. Additional energy expenditure comes from physical activity (15–30%) and the thermic effect of food—the energy needed to digest, absorb, and process nutrients (approximately 10%).
Several factors influence metabolic rate, including body composition (muscle tissue is more metabolically active than fat tissue), age, sex, genetics, and hormonal status. Thyroid hormones, particularly thyroxine (T4) and triiodothyronine (T3), play a crucial regulatory role by controlling the rate of cellular metabolism. The hypothalamic-pituitary-thyroid axis maintains metabolic homeostasis through negative feedback mechanisms.
Metabolism is remarkably adaptive, responding to changes in energy intake, physical activity, and environmental conditions. This adaptive capacity, known as metabolic flexibility, allows the body to switch between different fuel sources (carbohydrates, fats, proteins) depending on availability and demand. Understanding these fundamental processes helps contextualise concerns about whether metabolism can be permanently compromised through lifestyle factors or dietary practices.
Can You Permanently Damage Your Metabolism?
The concept of 'ruining' or permanently damaging metabolism is largely a misconception, though metabolic rate can certainly be influenced by various factors. The human body possesses remarkable adaptive mechanisms that allow metabolism to adjust in response to changing circumstances. Whilst significant metabolic changes can occur, these are typically reversible with appropriate intervention rather than representing permanent damage.
Metabolic adaptation, sometimes termed 'adaptive thermogenesis', describes the body's response to prolonged caloric restriction. During extended periods of reduced energy intake, the body becomes more metabolically efficient, reducing energy expenditure beyond what would be predicted by changes in body composition alone. Evidence shows metabolic adaptation can persist for months to years after weight loss but is modifiable; there is no robust evidence of irreversible 'damage' from dieting in otherwise healthy individuals. Studies following participants from weight loss programmes have demonstrated that whilst metabolic rate may remain lower than expected, it continues to function and can improve with targeted interventions.
Certain medical conditions can significantly affect metabolic function. Hypothyroidism, characterised by insufficient thyroid hormone production, reduces metabolic rate and may cause weight gain, fatigue, and cold intolerance. This condition is treatable with levothyroxine replacement therapy, which typically restores normal metabolic function. Treatment decisions differ for overt versus subclinical hypothyroidism, following NICE and BNF guidance. Conversely, hyperthyroidism can increase metabolic rate, potentially causing weight loss, tremor, and palpitations—symptoms that warrant medical advice. Other conditions such as polycystic ovary syndrome (PCOS), Cushing's syndrome, and other endocrine disorders can alter metabolism but are manageable with appropriate medical treatment.
The key distinction is between metabolic adaptation—a normal physiological response—and true metabolic dysfunction requiring medical intervention. Whilst extreme or prolonged dietary restriction, excessive exercise, or underlying medical conditions can significantly impact metabolic rate, these effects are generally not permanent and respond to evidence-based treatment approaches.
Factors That Slow Down Metabolic Rate
Multiple physiological and lifestyle factors can contribute to a reduction in metabolic rate, some of which are modifiable whilst others represent natural biological processes.
Age-related metabolic decline is a well-documented phenomenon. Metabolic rate typically decreases by approximately 1–2% per decade after age 30, primarily due to loss of lean muscle mass (sarcopenia) and hormonal changes. This natural decline is partly inevitable but can be mitigated through resistance training and adequate protein intake to preserve muscle tissue.
Severe caloric restriction and crash dieting represent significant metabolic stressors. When energy intake drops substantially below requirements, the body initiates protective mechanisms to conserve energy. This includes reduced thyroid hormone conversion (decreased T3 production), lowered sympathetic nervous system activity, and decreased spontaneous physical activity. Very low-calorie diets (below 800 kcal daily) can reduce metabolic rate significantly and should only be undertaken with clinical supervision (e.g., via NHS or specialist services).
Sedentary behaviour and insufficient physical activity contribute to lower metabolic rate through multiple mechanisms. Lack of exercise leads to muscle loss, reducing the metabolically active tissue that burns calories at rest. Additionally, prolonged sitting decreases non-exercise activity thermogenesis (NEAT)—the energy expended during daily activities outside formal exercise.
Sleep deprivation and chronic stress affect metabolic function through hormonal pathways. Insufficient sleep (less than 7 hours nightly) disrupts leptin and ghrelin regulation, increases cortisol production, and impairs glucose metabolism. Elevated cortisol from chronic stress promotes fat storage, particularly visceral adiposity, and can reduce insulin sensitivity.
Other factors include:
-
Inadequate protein intake, reducing the thermic effect of food and muscle maintenance
-
Certain medications, including some antidepressants, antipsychotics, and beta-blockers (do not stop or change prescribed medicines without speaking to your GP or pharmacist)
-
Endocrine and metabolic conditions such as hypothyroidism, PCOS, or insulin resistance
-
Hydration status – maintaining adequate fluid intake supports overall metabolic function
Recognising these factors enables targeted interventions to support metabolic health.
Signs Your Metabolism May Be Affected
Identifying potential metabolic changes can be challenging, as symptoms often develop gradually and may overlap with other conditions. However, certain signs warrant attention and possible medical evaluation.
Unexplained weight changes represent a primary indicator of altered metabolic function. Persistent weight gain despite maintaining usual dietary and activity patterns, or conversely, unexpected weight loss, may suggest metabolic dysregulation. It is important to note that weight fluctuations can result from numerous factors including fluid retention, medication effects, or underlying medical conditions, so isolated weight changes do not necessarily indicate metabolic problems.
Persistent fatigue and low energy levels that do not improve with adequate rest may reflect reduced metabolic efficiency. This can manifest as difficulty completing previously manageable activities, excessive daytime sleepiness, or requiring longer recovery periods after exertion. When accompanied by cold intolerance, dry skin, hair loss, or constipation, these symptoms may indicate hypothyroidism and warrant thyroid function testing (TSH, free T4).
Changes in body composition, particularly increased central adiposity with concurrent muscle loss, can signal metabolic alterations. This pattern is commonly associated with insulin resistance, metabolic syndrome, or age-related metabolic decline. Difficulty building or maintaining muscle mass despite resistance training may also indicate metabolic or hormonal issues.
Appetite and satiety dysregulation may reflect metabolic hormone imbalances. Persistent hunger shortly after meals, intense cravings (particularly for carbohydrates), or loss of normal satiety signals can indicate leptin resistance or other metabolic disturbances.
Additional concerning signs include:
-
Cognitive changes: difficulty concentrating, memory problems, or 'brain fog'
-
Mood alterations: depression, anxiety, or irritability
-
Sleep disturbances: insomnia or non-restorative sleep
-
Temperature regulation issues: feeling excessively cold or heat intolerant
When to contact your GP: If you experience multiple symptoms persisting beyond 2–3 weeks, unexplained weight changes (as a general guide, exceeding 5% of body weight), or symptoms significantly affecting daily function, arrange a consultation. Seek urgent medical advice for new polyuria/polydipsia with unexplained weight loss (possible diabetes), persistent unintentional weight loss with other symptoms, or palpitations/tremor/heat intolerance (possible hyperthyroidism). Your GP can perform appropriate investigations including thyroid function tests, HbA1c (and/or fasting glucose as indicated), lipid profile, and other relevant assessments to identify underlying causes.
How to Support and Restore Healthy Metabolism
Supporting metabolic health involves evidence-based lifestyle modifications and, when necessary, medical intervention. A comprehensive approach addresses multiple factors influencing metabolic function.
Adequate nutrition forms the foundation of metabolic health. Avoid severe caloric restriction; instead, aim for moderate deficits (300–500 kcal below maintenance) if weight loss is required. Ensure sufficient protein intake – most adults require at least 0.75 g/kg/day; 1.2–1.6 g/kg/day may help preserve lean mass during weight loss. Seek personalised advice, especially if you have kidney disease. Include a variety of whole foods providing essential micronutrients—particularly iodine, selenium, zinc, and iron—which support thyroid function and metabolic processes. Aim to meet these requirements through diet; avoid supplements (especially iodine) unless advised by your clinician. Regular meal timing may help regulate metabolic hormones, though there is no official link confirming superiority of any specific eating pattern.
Resistance training helps preserve and increase muscle mass and may modestly increase resting energy expenditure. Combine this with regular aerobic activity and daily movement for optimal metabolic health. The UK Chief Medical Officers' Physical Activity Guidelines recommend at least 150 minutes of moderate-intensity or 75 minutes of vigorous-intensity activity weekly, plus muscle-strengthening activities on at least two days weekly to enhance overall metabolic health and insulin sensitivity.
Sleep optimisation is crucial for metabolic regulation. Aim for 7–9 hours of quality sleep nightly. Establish consistent sleep-wake times, create a cool, dark sleeping environment, and limit screen exposure before bedtime. Address sleep disorders such as obstructive sleep apnoea, which significantly impairs metabolic function.
Stress management helps regulate cortisol and supports metabolic homeostasis. Evidence-based approaches include cognitive behavioural therapy (CBT), mindfulness-based stress reduction, regular physical activity, and maintaining social connections.
Hydration supports metabolic processes; aim for 6–8 glasses (approximately 1.5–2 litres) of fluid daily, adjusting for activity level and climate.
Medical management: If underlying conditions are identified, appropriate treatment is essential. Hypothyroidism requires levothyroxine replacement; dosing is individual – for many adults 50–100 micrograms daily initially, with lower starting doses (e.g., 12.5–25 micrograms) in older adults or those with cardiac disease. Doses are titrated according to thyroid function tests. PCOS management may include combined oral contraceptives or metformin (which may be prescribed off-label in the UK) following specialist or GP advice. Regular monitoring ensures treatment effectiveness. Do not start or stop prescribed medicines or supplements without medical advice.
Avoid extreme approaches: 'Metabolic reset' diets, excessive supplementation, or extreme exercise regimens lack robust evidence and may prove counterproductive. Focus instead on sustainable, evidence-based interventions that support long-term metabolic health. If implementing lifestyle changes does not produce expected improvements within 3–6 months, or if symptoms worsen, seek medical review to exclude underlying pathology requiring specific treatment.
Frequently Asked Questions
Does crash dieting permanently damage metabolism?
No, crash dieting does not permanently damage metabolism. Whilst severe caloric restriction causes metabolic adaptation (reduced energy expenditure), this is a reversible physiological response that improves with appropriate nutrition, resistance training, and adequate energy intake.
What medical conditions can affect metabolic rate?
Hypothyroidism, hyperthyroidism, polycystic ovary syndrome (PCOS), Cushing's syndrome, and other endocrine disorders can significantly affect metabolic rate. These conditions are manageable with appropriate medical treatment, and thyroid disorders typically respond well to hormone replacement therapy.
How can I support healthy metabolism naturally?
Support healthy metabolism through adequate protein intake (at least 0.75 g/kg/day), regular resistance training and physical activity, 7–9 hours quality sleep nightly, stress management, and avoiding severe caloric restriction. If symptoms persist despite lifestyle changes, consult your GP for medical assessment.
The health-related content published on this site is based on credible scientific sources and is periodically reviewed to ensure accuracy and relevance. Although we aim to reflect the most current medical knowledge, the material is meant for general education and awareness only.
The information on this site is not a substitute for professional medical advice. For any health concerns, please speak with a qualified medical professional. By using this information, you acknowledge responsibility for any decisions made and understand we are not liable for any consequences that may result.
Heading 1
Heading 2
Heading 3
Heading 4
Heading 5
Heading 6
Lorem ipsum dolor sit amet, consectetur adipiscing elit, sed do eiusmod tempor incididunt ut labore et dolore magna aliqua. Ut enim ad minim veniam, quis nostrud exercitation ullamco laboris nisi ut aliquip ex ea commodo consequat. Duis aute irure dolor in reprehenderit in voluptate velit esse cillum dolore eu fugiat nulla pariatur.
Block quote
Ordered list
- Item 1
- Item 2
- Item 3
Unordered list
- Item A
- Item B
- Item C
Bold text
Emphasis
Superscript
Subscript