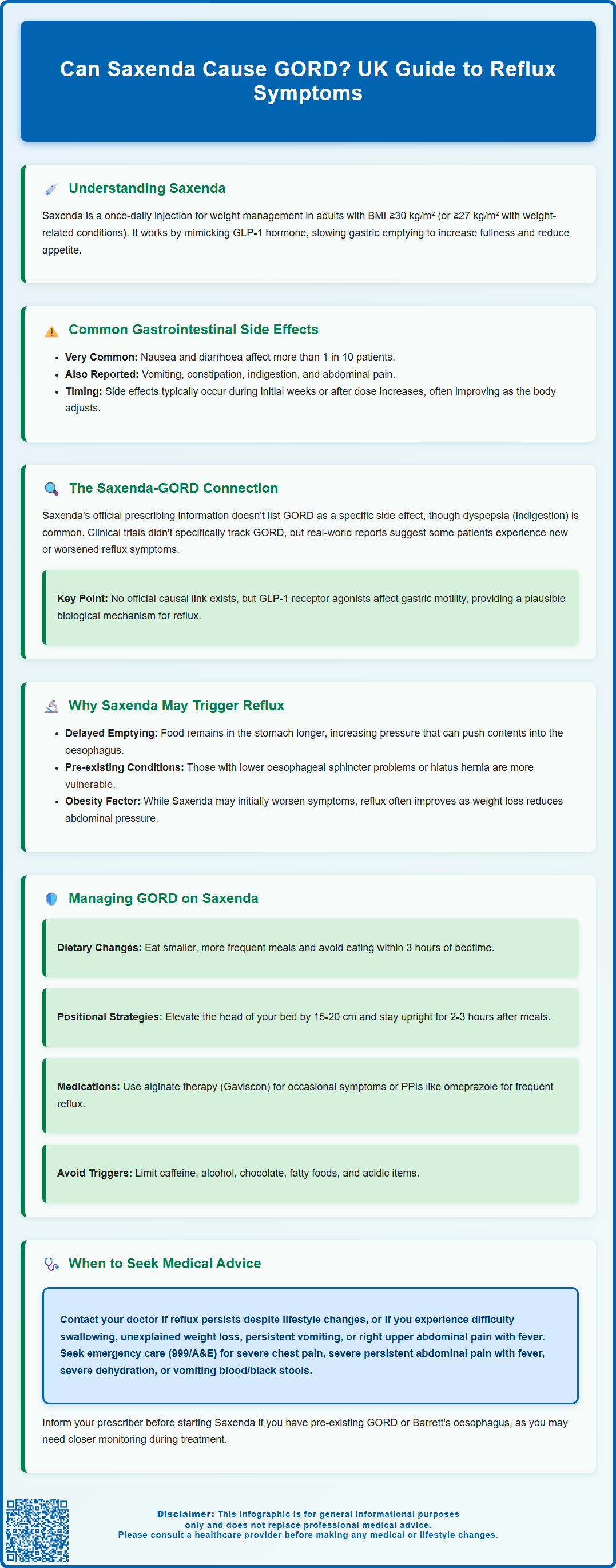
Can Saxenda cause GORD? Saxenda (liraglutide 3.0 mg) is a GLP-1 receptor agonist licensed in the UK for weight management. Whilst gastro-oesophageal reflux disease (GORD) is not listed as a specific adverse reaction in official prescribing information, the medication's effect on gastric emptying may trigger or worsen reflux symptoms in some patients. Dyspepsia, a common side effect with overlapping symptoms, affects up to 1 in 10 people taking Saxenda. Understanding the relationship between this medication and reflux symptoms helps patients and clinicians manage treatment effectively whilst optimising weight loss outcomes.
Summary: Saxenda is not officially documented to cause GORD, though its mechanism of delaying gastric emptying may trigger or worsen reflux symptoms in some patients.
- Saxenda (liraglutide 3.0 mg) is a GLP-1 receptor agonist licensed in the UK for weight management as an adjunct to diet and exercise.
- The medication slows gastric emptying, which increases satiety but may elevate intragastric pressure and promote reflux in susceptible individuals.
- Dyspepsia is a common side effect (1 in 10 to 1 in 100 patients), with symptoms overlapping those of GORD including heartburn and upper abdominal discomfort.
- Lifestyle modifications, alginate therapy, and proton pump inhibitors can help manage reflux symptoms whilst continuing Saxenda treatment.
- Patients should seek medical advice for persistent symptoms, difficulty swallowing, severe abdominal pain, or signs of gastrointestinal bleeding.
- Treatment should be discontinued if the 3.0 mg maintenance dose cannot be tolerated or if inadequate weight loss occurs after 12 weeks.
Table of Contents
Understanding Saxenda and Its Gastrointestinal Effects
Saxenda (liraglutide 3.0 mg) is a glucagon-like peptide-1 (GLP-1) receptor agonist licensed in the UK for weight management in adults with a body mass index (BMI) of 30 kg/m² or greater, or 27 kg/m² or greater with weight-related comorbidities, as an adjunct to a reduced-calorie diet and increased physical activity. Administered as a once-daily subcutaneous injection at the same time each day (with or without food), Saxenda works by mimicking the action of the naturally occurring hormone GLP-1, which regulates appetite and food intake.
The mechanism of action of Saxenda involves several physiological effects that directly impact the gastrointestinal system. GLP-1 receptor agonists slow gastric emptying, meaning food remains in the stomach for longer periods before passing into the small intestine. This delayed gastric emptying contributes to increased satiety and reduced appetite, which are central to the medication's weight loss effects. Additionally, Saxenda influences areas of the brain involved in appetite regulation, further supporting calorie reduction.
Gastrointestinal side effects are among the most commonly reported adverse reactions with Saxenda therapy. According to the Summary of Product Characteristics (SmPC) approved by the Medicines and Healthcare products Regulatory Agency (MHRA), nausea and diarrhoea are very common, affecting more than 1 in 10 patients. Vomiting, constipation, dyspepsia, and abdominal pain are also frequently reported. These effects typically occur during the initial weeks of treatment or following dose escalation, and often diminish over time as the body adapts to the medication.
It's important to note that GLP-1 receptor agonists like Saxenda can also be associated with gallbladder disease, which may cause upper abdominal symptoms. Patients should seek medical advice if they experience right upper quadrant pain, fever, or jaundice.
Understanding these gastrointestinal effects is essential for patients considering or currently taking Saxenda, as they may influence treatment tolerability and adherence. Whilst many side effects are transient and manageable, some patients may experience more persistent symptoms that require clinical attention or treatment modification. If a patient cannot tolerate the 3.0 mg maintenance dose, treatment should be discontinued. Additionally, if less than 5% weight loss is achieved after 12 weeks on the 3.0 mg dose, treatment should be stopped.
The Link Between Saxenda and GORD: What the Evidence Shows
Gastro-oesophageal reflux disease (GORD), also called GERD in some sources, is characterised by the backward flow of stomach contents into the oesophagus, causing symptoms such as heartburn, regurgitation, and chest discomfort. The relationship between Saxenda and GORD has been a subject of clinical interest, though the evidence base requires careful interpretation.
The official prescribing information for Saxenda (MHRA/EMC SmPC) does not list GORD as a specific adverse reaction in the standard frequency categories. However, dyspepsia (indigestion) is documented as a common side effect, affecting between 1 in 10 and 1 in 100 patients. Dyspepsia and GORD share overlapping symptoms, including upper abdominal discomfort, burning sensations, and acid-related symptoms, which can make clinical distinction challenging. Some patients reporting dyspepsia may actually be experiencing reflux symptoms.
Clinical trial data and post-marketing surveillance have provided insights into gastrointestinal tolerability. In the SCALE (Satiety and Clinical Adiposity – Liraglutide Evidence) clinical trial programme, which formed the basis for Saxenda's approval, gastrointestinal adverse events were prominent but specific reporting of GORD as a distinct entity was limited. Real-world evidence and patient reports suggest that some individuals do experience new-onset or worsened reflux symptoms whilst taking Saxenda, though establishing direct causation remains complex.
There is no official, definitively established causal link between Saxenda and GORD in regulatory documentation. However, the pharmacological effects of GLP-1 receptor agonists on gastric motility provide a plausible biological mechanism through which reflux symptoms might occur or worsen. Healthcare professionals should remain alert to reflux-related complaints in patients taking Saxenda and assess whether symptoms represent true GORD, functional dyspepsia, or other gastrointestinal disturbances.
It's worth noting that GORD is usually a clinical diagnosis, with endoscopy reserved for patients with alarm features or those who don't respond to treatment, in line with NICE guidance. Individual patient factors, including pre-existing reflux disease, obesity-related reflux, and concurrent medications, must also be considered when evaluating symptom causation.
Why Saxenda May Trigger or Worsen Acid Reflux
Several pharmacological and physiological mechanisms may explain why some patients experience reflux symptoms whilst taking Saxenda. Understanding these mechanisms helps both patients and clinicians anticipate and manage potential side effects more effectively.
Delayed gastric emptying is the primary mechanism through which Saxenda might contribute to reflux symptoms. By activating GLP-1 receptors in the stomach, liraglutide significantly slows the rate at which food moves from the stomach into the duodenum. Whilst this promotes satiety and reduces calorie intake, it also means that stomach contents remain present for extended periods. This prolonged gastric distension can increase intragastric pressure, potentially overwhelming the lower oesophageal sphincter (LOS) – the muscular valve that normally prevents stomach contents from flowing backwards into the oesophagus.
Additionally, increased gastric volume and pressure from delayed emptying may exacerbate reflux in individuals with pre-existing LOS dysfunction or hiatus hernia. Patients who already have compromised oesophageal defence mechanisms may be particularly susceptible to developing symptomatic reflux when gastric emptying is pharmacologically slowed.
Nausea and dietary changes associated with Saxenda may also play indirect roles. Some patients experiencing nausea may alter their eating patterns, consuming smaller, more frequent meals or changing food choices. Certain dietary modifications, whilst well-intentioned, might inadvertently trigger reflux if they include foods known to relax the LOS or increase gastric acid production.
It is important to note that obesity itself is a significant risk factor for GORD. Excess abdominal adiposity increases intra-abdominal pressure, which can promote reflux. As patients lose weight on Saxenda, this mechanical pressure typically decreases, potentially improving reflux symptoms over time. Therefore, the relationship between Saxenda and reflux may be temporally complex – initial worsening due to delayed gastric emptying, followed by improvement as weight loss progresses.
Interestingly, the GLP-1-mediated gastric emptying delay may attenuate over time (tachyphylaxis), which could explain why some patients experience improvement in gastrointestinal symptoms with continued treatment. Individual responses vary considerably, and not all patients will experience reflux symptoms whilst taking this medication.
Managing GORD Symptoms While Taking Saxenda
For patients experiencing reflux symptoms whilst taking Saxenda, several practical management strategies can help improve tolerability without necessarily discontinuing treatment. These approaches should be implemented in consultation with a healthcare professional.
Lifestyle and dietary modifications form the foundation of reflux management and align with NICE guidance on GORD. Key recommendations include:
-
Eating smaller, more frequent meals rather than large portions, which can reduce gastric distension
-
Avoiding eating within 3 hours of bedtime to allow partial gastric emptying before lying down
-
Elevating the head of the bed by 15–20 cm, which uses gravity to reduce nocturnal reflux
-
Identifying and avoiding trigger foods such as caffeine, alcohol, chocolate, fatty foods, and acidic items
-
Maintaining an upright posture after meals for at least 2–3 hours
-
Wearing loose-fitting clothing to avoid increasing abdominal pressure
Pharmacological management may be appropriate for persistent symptoms. Over-the-counter antacids can provide rapid, short-term relief for occasional heartburn. Alginate therapy (such as Gaviscon) forms a protective raft on top of stomach contents, preventing reflux and is widely recommended in UK practice. For more frequent symptoms, proton pump inhibitors (PPIs) such as omeprazole or lansoprazole are highly effective at reducing gastric acid production. These are available over the counter at lower doses or on prescription for standard therapeutic doses. H2-receptor antagonists (e.g., famotidine) represent another option, though PPIs are generally more effective for moderate to severe symptoms.
Patients should discuss with their GP or prescribing clinician whether dose adjustment of Saxenda might be beneficial. The medication is titrated gradually from 0.6 mg to the maintenance dose of 3.0 mg over several weeks. If reflux symptoms emerge or worsen during dose escalation, the SmPC advises considering delaying the dose increase by one week. If the 3.0 mg dose cannot be tolerated, treatment should be discontinued.
Timing of Saxenda administration should be consistent, with injections given at the same time each day (with or without food) as per the SmPC. Some patients find that administering the injection at a different time of day may influence symptom patterns, though evidence for this approach is anecdotal rather than evidence-based. Continued monitoring and open communication with healthcare providers ensures that management strategies can be refined based on individual response and symptom evolution.
Patients are encouraged to report any suspected side effects to the MHRA Yellow Card Scheme (yellowcard.mhra.gov.uk or via the Yellow Card app).
When to Seek Medical Advice About Reflux on Saxenda
Whilst mild, transient reflux symptoms may be manageable with lifestyle modifications and over-the-counter remedies, certain situations warrant prompt medical evaluation. Patients should be aware of warning signs that indicate the need for professional assessment.
Contact your GP or prescribing clinician if you experience:
-
Persistent or worsening reflux symptoms despite lifestyle modifications and appropriate use of antacids or PPIs
-
Difficulty or pain when swallowing (dysphagia or odynophagia), which may indicate oesophageal inflammation or stricture and requires urgent referral per NICE guidance
-
Unintentional weight loss beyond expected therapeutic weight reduction, particularly if accompanied by reduced appetite or difficulty eating
-
Persistent nausea or vomiting that interferes with adequate nutrition or hydration
-
Right upper quadrant pain, fever, or jaundice, which could indicate gallbladder disease – a known risk with GLP-1 receptor agonists and rapid weight loss
Seek urgent medical attention (contact 999 or attend A&E) if you develop:
-
Severe chest pain, particularly if it differs from typical reflux discomfort, as cardiac causes must be excluded
-
Severe, persistent abdominal pain, especially if accompanied by fever, as this may indicate pancreatitis – a rare but serious adverse effect of GLP-1 receptor agonists
-
Signs of severe dehydration from persistent vomiting, including reduced urination, dizziness, or confusion
-
Vomiting blood (haematemesis) or passing black, tarry stools (melaena), which may indicate gastrointestinal bleeding
Regular monitoring and review are essential components of safe Saxenda therapy. NICE guidance on obesity management emphasises the importance of ongoing clinical assessment. Your healthcare provider should review treatment response, tolerability, and any adverse effects at regular intervals. If reflux symptoms significantly impair quality of life or prevent continuation of therapy, your clinician may consider alternative weight management strategies, including other pharmacological options or referral to specialist weight management services.
Patients with pre-existing GORD or Barrett's oesophagus should inform their prescriber before starting Saxenda, as closer monitoring may be appropriate. Similarly, those taking medications that may interact with treatments for reflux should ensure their healthcare provider has a complete medication history. Collaborative decision-making between patient and clinician ensures that the benefits of weight loss therapy are balanced against tolerability and safety considerations, optimising outcomes whilst minimising adverse effects.
Frequently Asked Questions
Does Saxenda officially cause GORD?
GORD is not listed as a specific adverse reaction in Saxenda's UK prescribing information, though dyspepsia (indigestion) is a common side effect. Some patients may experience reflux symptoms due to the medication's effect on gastric emptying, but a definitive causal link has not been established in regulatory documentation.
How does Saxenda affect the digestive system?
Saxenda slows gastric emptying by activating GLP-1 receptors, meaning food remains in the stomach longer. This increases satiety and supports weight loss but may also increase gastric pressure, potentially triggering reflux symptoms in susceptible individuals.
What should I do if I develop reflux symptoms on Saxenda?
Start with lifestyle modifications such as smaller meals, avoiding eating before bedtime, and elevating the head of your bed. Over-the-counter alginate therapy or antacids may help, and your GP can prescribe proton pump inhibitors for persistent symptoms. Contact your healthcare provider if symptoms worsen or do not improve with these measures.
The health-related content published on this site is based on credible scientific sources and is periodically reviewed to ensure accuracy and relevance. Although we aim to reflect the most current medical knowledge, the material is meant for general education and awareness only.
The information on this site is not a substitute for professional medical advice. For any health concerns, please speak with a qualified medical professional. By using this information, you acknowledge responsibility for any decisions made and understand we are not liable for any consequences that may result.
Heading 1
Heading 2
Heading 3
Heading 4
Heading 5
Heading 6
Lorem ipsum dolor sit amet, consectetur adipiscing elit, sed do eiusmod tempor incididunt ut labore et dolore magna aliqua. Ut enim ad minim veniam, quis nostrud exercitation ullamco laboris nisi ut aliquip ex ea commodo consequat. Duis aute irure dolor in reprehenderit in voluptate velit esse cillum dolore eu fugiat nulla pariatur.
Block quote
Ordered list
- Item 1
- Item 2
- Item 3
Unordered list
- Item A
- Item B
- Item C
Bold text
Emphasis
Superscript
Subscript