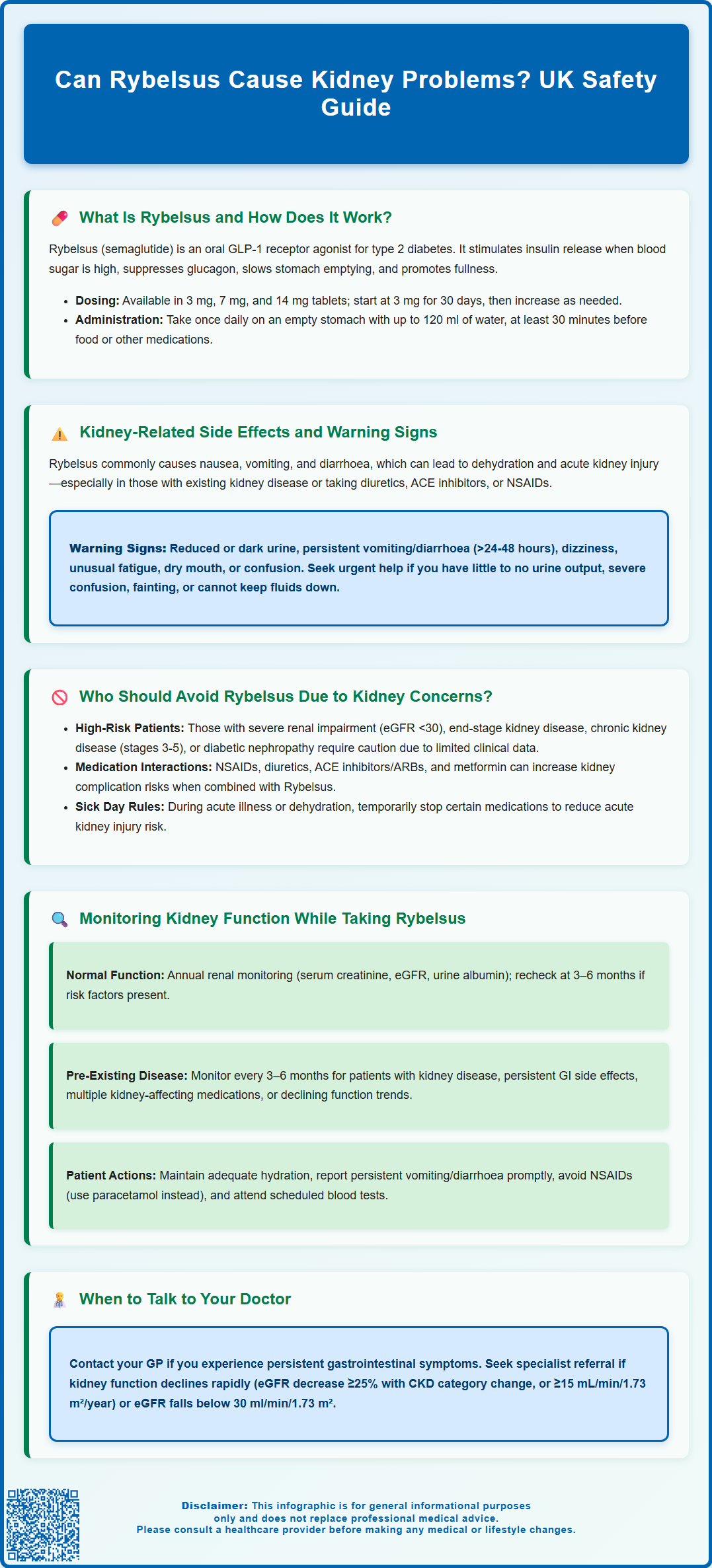
Rybelsus (semaglutide) is an oral GLP-1 receptor agonist licensed in the UK for type 2 diabetes management. Whilst it offers effective glycaemic control and potential weight benefits, understanding its renal safety profile is essential for prescribers and patients alike. Although Rybelsus does not directly damage the kidneys, gastrointestinal side effects—particularly nausea, vomiting, and diarrhoea—can lead to dehydration and precipitate acute kidney injury in susceptible individuals. This article examines the relationship between Rybelsus and kidney function, identifies at-risk patient groups, and outlines monitoring strategies to ensure safe use in clinical practice.
Summary: Rybelsus does not directly cause kidney damage, but gastrointestinal side effects can lead to dehydration-induced acute kidney injury in vulnerable patients.
- Rybelsus is a GLP-1 receptor agonist that stimulates glucose-dependent insulin secretion and suppresses glucagon release.
- Common gastrointestinal effects (nausea, vomiting, diarrhoea) may cause dehydration, reducing renal perfusion and precipitating acute kidney injury.
- Patients with pre-existing chronic kidney disease, elderly individuals, and those on nephrotoxic medications require careful assessment before initiation.
- Regular monitoring of renal function (eGFR, serum creatinine) is recommended, with more frequent checks for at-risk groups or during persistent gastrointestinal symptoms.
- Warning signs include reduced urine output, persistent vomiting or diarrhoea, dizziness, and unusual fatigue—prompt medical review is essential if these occur.
Table of Contents
What Is Rybelsus and How Does It Work?
Rybelsus (semaglutide) is an oral medication licensed in the UK for the treatment of type 2 diabetes mellitus in adults. It belongs to a class of drugs known as glucagon-like peptide-1 (GLP-1) receptor agonists. Rybelsus is typically prescribed when diet and exercise alone have not achieved adequate glycaemic control, and it may be used alongside other glucose-lowering medications such as metformin or insulin.
The mechanism of action of Rybelsus centres on mimicking the naturally occurring hormone GLP-1, which is released by the intestine in response to food intake. By binding to GLP-1 receptors in the pancreas, semaglutide stimulates insulin secretion in a glucose-dependent manner—meaning it only promotes insulin release when blood glucose levels are elevated. This reduces the risk of hypoglycaemia compared to some other diabetes medications, particularly when used alone or without insulin or sulfonylureas. Additionally, Rybelsus suppresses glucagon secretion, slows gastric emptying, and promotes satiety, which can contribute to weight loss—a beneficial effect for many patients with type 2 diabetes.
Rybelsus is available in three tablet strengths: 3 mg, 7 mg, and 14 mg. Treatment begins with the 3 mg dose for 30 days as an initiation dose only (not for ongoing glycaemic control), before escalating to 7 mg and potentially 14 mg if further glycaemic control is required. The tablet must be taken once daily on an empty stomach with a small amount of water (up to 120 ml), at least 30 minutes before any food, drink, or other oral medications. Tablets should be swallowed whole and not split, crushed or chewed. This specific administration requirement is essential for optimal absorption, as semaglutide has relatively low oral bioavailability.
While Rybelsus is generally well tolerated, understanding its potential effects on various organ systems—including the kidneys—is crucial for safe prescribing and patient monitoring.
Kidney-Related Side Effects and Warning Signs
Acute kidney injury (AKI) has been reported with semaglutide, usually secondary to dehydration from gastrointestinal adverse effects. While direct nephrotoxicity is not well-established, rare cases of intrinsic renal injury have been reported. The most clinically significant concern relates to gastrointestinal adverse effects, which are common with GLP-1 receptor agonists.
Patients taking Rybelsus frequently experience nausea, vomiting, and diarrhoea, especially during the initial weeks of treatment or following dose escalation. These symptoms can lead to dehydration and volume depletion, which may precipitate acute kidney injury (AKI) in susceptible individuals. Dehydration reduces renal perfusion, and in patients with pre-existing chronic kidney disease (CKD) or those taking other medications that affect kidney function (such as diuretics, ACE inhibitors, or NSAIDs), this can result in a significant decline in glomerular filtration rate (GFR).
Warning signs that may indicate kidney problems or dehydration include:
-
Reduced urine output or dark-coloured urine
-
Persistent nausea, vomiting, or diarrhoea lasting more than 24–48 hours
-
Dizziness or lightheadedness, particularly on standing
-
Unusual fatigue or weakness
-
Dry mouth and increased thirst
-
Confusion or altered mental state (in severe cases)
Patients experiencing gastrointestinal symptoms should be advised to maintain adequate fluid intake and contact their GP or diabetes specialist nurse promptly. Renal function (U&Es/eGFR) should be checked if persistent vomiting or diarrhoea occurs, and temporary discontinuation of Rybelsus may be necessary until fluid balance is restored and kidney function stabilises.
Seek urgent medical help (call NHS 111 or 999) if you experience minimal or absent urine output, severe confusion, fainting, or signs of severe dehydration that prevent you from keeping fluids down.
If you suspect Rybelsus has caused side effects, report them through the MHRA Yellow Card scheme (yellowcard.mhra.gov.uk).
Who Should Avoid Rybelsus Due to Kidney Concerns?
Rybelsus is not contraindicated in patients with chronic kidney disease, and dose adjustment based solely on renal function is not required according to current prescribing information. However, caution is advised in certain patient populations where the risk of kidney-related complications may be elevated.
Patients with severe renal impairment (estimated glomerular filtration rate [eGFR] less than 30 ml/min/1.73 m²) or end-stage kidney disease should be prescribed Rybelsus with particular caution, as there is limited clinical experience in this population. Whilst pharmacokinetic studies suggest that renal impairment does not significantly alter semaglutide exposure (as the drug is primarily metabolised via proteolytic cleavage rather than renal excretion), the increased vulnerability to dehydration-induced AKI remains a concern.
Specific patient groups requiring careful assessment include:
-
Individuals with pre-existing CKD (stages 3–5), particularly if eGFR is declining
-
Patients taking concomitant nephrotoxic medications (NSAIDs, aminoglycoside antibiotics, ACE inhibitors/ARBs, diuretics, metformin)
-
Those with a history of acute kidney injury
-
Elderly patients, who may have reduced renal reserve and be more susceptible to dehydration
-
Patients with diabetic nephropathy, where glycaemic control must be balanced against renal protection
Before initiating Rybelsus, clinicians should conduct a comprehensive medication review to identify drugs that may increase the risk of renal complications. During acute illness or dehydration, UK 'sick day rules' should be considered, which may involve temporarily withholding certain medications (SGLT2 inhibitors, ACE inhibitors/ARBs, diuretics, metformin and NSAIDs) to reduce AKI risk.
According to NICE guidance on type 2 diabetes management (NG28) and chronic kidney disease (NG203), baseline renal function should be assessed, and the overall risk-benefit profile considered for each patient. In some cases, alternative glucose-lowering therapies with more established safety profiles in advanced CKD may be more appropriate. Shared decision-making with patients, incorporating discussion of potential risks and the importance of monitoring, is essential to safe prescribing practice.
Monitoring Kidney Function While Taking Rybelsus
Regular monitoring of renal function is an important component of diabetes care and becomes particularly relevant when prescribing medications like Rybelsus that may indirectly affect the kidneys. Whilst routine monitoring protocols are primarily guided by the patient's baseline kidney function and overall diabetes management plan, certain situations warrant more frequent assessment.
For patients with normal baseline renal function, standard diabetes care typically includes annual measurement of serum creatinine and calculation of eGFR, alongside urine albumin-to-creatinine ratio (ACR) to screen for diabetic nephropathy. Any raised ACR should be confirmed on repeat testing. This aligns with NICE recommendations for type 2 diabetes monitoring. However, when initiating Rybelsus, particularly in patients with risk factors for kidney disease, it may be prudent to recheck renal function within 3–6 months of starting treatment to ensure stability.
More frequent monitoring (every 3–6 months or sooner) is advisable for:
-
Patients with pre-existing CKD (eGFR <60 ml/min/1.73 m²)
-
Those experiencing persistent gastrointestinal side effects
-
Individuals taking multiple medications affecting renal function
-
Patients with declining eGFR trends prior to Rybelsus initiation
-
Elderly patients or those with cardiovascular comorbidities
Renal function should be measured promptly if significant gastrointestinal adverse effects occur after starting or up-titrating Rybelsus.
Patient education plays a vital role in kidney protection. Individuals should be counselled to:
-
Maintain adequate hydration, especially during hot weather or illness
-
Report persistent vomiting or diarrhoea promptly
-
Avoid NSAIDs where possible (use paracetamol for pain relief)
-
Attend scheduled blood test appointments
If kidney function deteriorates significantly (e.g., sustained eGFR decrease ≥25% with change in CKD category within 12 months, or ≥15 mL/min/1.73 m²/year), clinicians should review the treatment regimen, consider temporary discontinuation of Rybelsus if dehydration is suspected, and investigate other potential causes of renal decline. Referral to a nephrologist may be appropriate for patients with rapidly declining function or eGFR <30 ml/min/1.73 m². Through vigilant monitoring and patient engagement, the benefits of Rybelsus in glycaemic control can be realised whilst minimising potential kidney-related risks.
Frequently Asked Questions
Does Rybelsus directly damage the kidneys?
No, Rybelsus does not directly damage kidney tissue. However, gastrointestinal side effects such as vomiting and diarrhoea can cause dehydration, which may lead to acute kidney injury, particularly in patients with pre-existing renal impairment or those taking other medications affecting kidney function.
Can I take Rybelsus if I have chronic kidney disease?
Rybelsus is not contraindicated in chronic kidney disease and does not require dose adjustment based on renal function. However, caution is advised in severe renal impairment (eGFR <30 ml/min/1.73 m²) due to limited clinical experience and increased vulnerability to dehydration-related complications.
How often should kidney function be monitored on Rybelsus?
Patients with normal baseline renal function typically require annual monitoring as part of standard diabetes care, with a recheck at 3–6 months after starting Rybelsus. Those with pre-existing chronic kidney disease, persistent gastrointestinal symptoms, or multiple nephrotoxic medications should have more frequent monitoring every 3–6 months or sooner if clinically indicated.
The health-related content published on this site is based on credible scientific sources and is periodically reviewed to ensure accuracy and relevance. Although we aim to reflect the most current medical knowledge, the material is meant for general education and awareness only.
The information on this site is not a substitute for professional medical advice. For any health concerns, please speak with a qualified medical professional. By using this information, you acknowledge responsibility for any decisions made and understand we are not liable for any consequences that may result.
Heading 1
Heading 2
Heading 3
Heading 4
Heading 5
Heading 6
Lorem ipsum dolor sit amet, consectetur adipiscing elit, sed do eiusmod tempor incididunt ut labore et dolore magna aliqua. Ut enim ad minim veniam, quis nostrud exercitation ullamco laboris nisi ut aliquip ex ea commodo consequat. Duis aute irure dolor in reprehenderit in voluptate velit esse cillum dolore eu fugiat nulla pariatur.
Block quote
Ordered list
- Item 1
- Item 2
- Item 3
Unordered list
- Item A
- Item B
- Item C
Bold text
Emphasis
Superscript
Subscript












