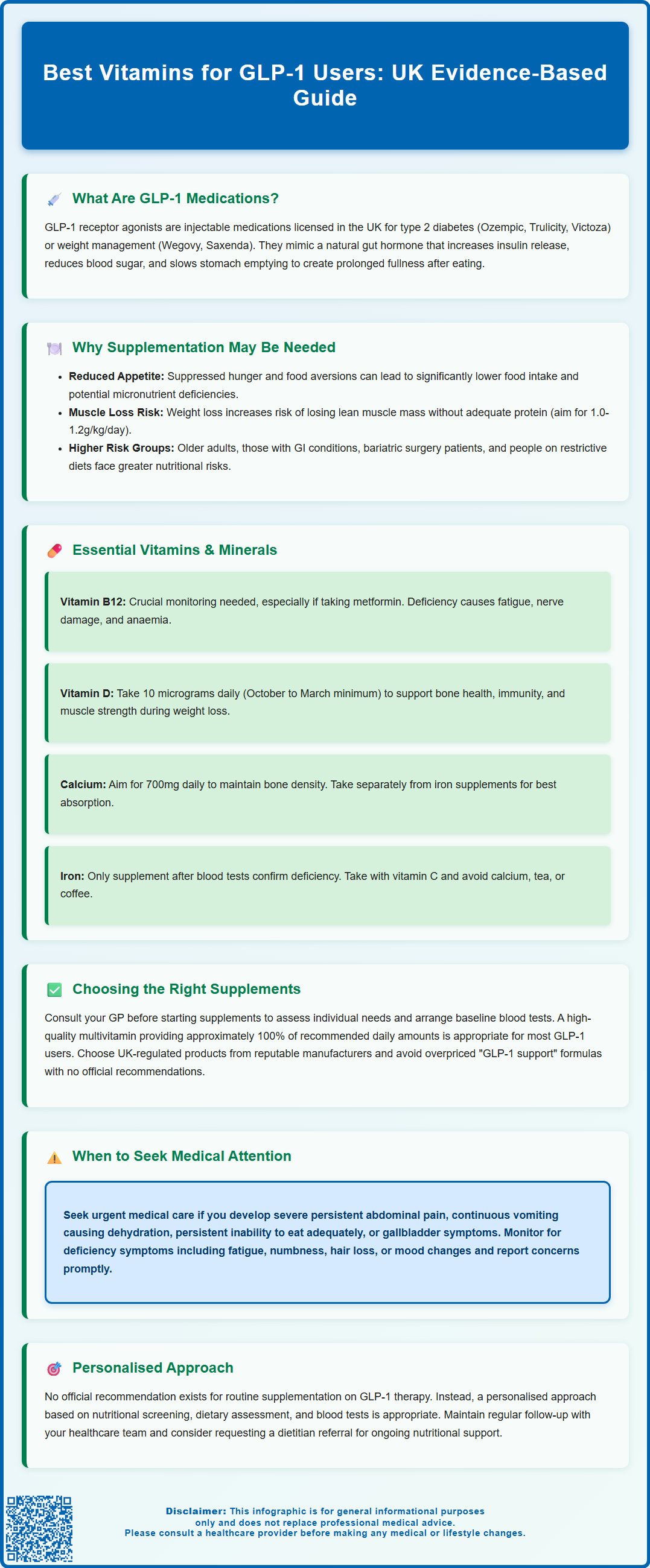
Glucagon-like peptide-1 (GLP-1) receptor agonists, including semaglutide and liraglutide, are increasingly prescribed in the UK for type 2 diabetes and weight management. Whilst these medications offer significant therapeutic benefits through appetite suppression and improved glycaemic control, the resulting reduction in food intake may affect nutritional status in some individuals. Understanding which vitamins and minerals warrant attention during GLP-1 therapy—and when supplementation may be appropriate—can help support overall health during treatment. This article examines the evidence-based approach to vitamin supplementation for GLP-1 users, emphasising individualised assessment and professional guidance rather than routine supplementation for all patients.
Summary: There is no official recommendation for routine vitamin supplementation for all GLP-1 users; instead, an individualised approach based on dietary assessment and blood tests is recommended, with particular attention to vitamin B12, vitamin D, calcium, and iron.
- GLP-1 receptor agonists slow gastric emptying and reduce appetite, which may decrease overall nutrient intake in some individuals.
- Vitamin B12 monitoring is particularly important for patients also taking metformin, as both medications can affect B12 status.
- The NHS recommends 10 micrograms of vitamin D daily for most UK adults, especially from October to March.
- Supplementation decisions should be guided by healthcare professionals following nutritional screening and blood tests rather than routine supplementation.
- Persistent vomiting, dehydration, or inability to maintain adequate oral intake whilst on GLP-1 therapy requires prompt medical review.
Table of Contents
What Are GLP-1 Medications and How Do They Work?
Glucagon-like peptide-1 (GLP-1) receptor agonists are a class of medications with specific UK licences: some are approved for type 2 diabetes management (semaglutide [Ozempic], dulaglutide [Trulicity], liraglutide [Victoza]), while others are specifically licensed for weight management in adults with obesity or overweight with weight-related comorbidities (semaglutide [Wegovy], liraglutide [Saxenda]). These medications are administered primarily via subcutaneous injection, though oral semaglutide is also available for type 2 diabetes.
GLP-1 receptor agonists work by mimicking the action of naturally occurring GLP-1, a hormone released by the intestine in response to food intake. They enhance insulin secretion when blood glucose levels are elevated, suppress glucagon release (which normally raises blood sugar), and slow gastric emptying. This delayed stomach emptying prolongs the sensation of fullness after meals, which contributes significantly to reduced calorie intake and subsequent weight loss.
The slowing of gastric emptying and the associated reduction in appetite mean that many patients on GLP-1 therapy consume smaller portions and may experience changes in food preferences. Whilst these effects are therapeutically beneficial for glycaemic control and weight reduction, they can potentially lead to reduced overall nutrient intake in some individuals. This may affect the intake of essential vitamins and minerals, particularly if the diet becomes more restrictive or less varied.
It's important to seek urgent medical attention if you experience severe, persistent abdominal pain (which could indicate pancreatitis, a rare but serious side effect), persistent vomiting leading to dehydration, or symptoms of gallbladder problems whilst taking these medications.
Why GLP-1 Users May Need Vitamin Supplementation
The appetite-suppressing effects of GLP-1 medications can result in reduced food intake over extended periods. Some patients report eating significantly smaller portion sizes, and many experience food aversions or nausea, particularly during the initial titration phase. This decrease in caloric consumption, combined with potential gastrointestinal side effects such as nausea, vomiting, and diarrhoea, may increase the risk of micronutrient deficiencies in certain individuals.
Weight loss, which is common with GLP-1 therapy, further compounds nutritional considerations. During weight loss, particularly if dietary protein intake is insufficient (generally aim for 1.0-1.2g/kg/day unless contraindicated), there is a risk of losing lean muscle mass alongside fat tissue. Adequate vitamin and mineral intake becomes important to support metabolic processes, maintain bone health, preserve muscle function, and support immune system integrity during this period of physiological change.
Certain populations on GLP-1 therapy may face heightened nutritional vulnerability. Older adults may already have marginal nutritional reserves and reduced absorption capacity. Patients with pre-existing gastrointestinal conditions, those who have undergone bariatric surgery (who typically require specific bariatric-formulation supplements), or individuals following restrictive diets (vegetarian, vegan) may enter GLP-1 treatment with suboptimal nutrient status. Additionally, the medication's effect on gastric emptying may theoretically affect the absorption of certain nutrients, though robust clinical evidence on this specific interaction remains limited.
It is important to note that there is no official recommendation for routine supplementation for all patients on GLP-1 medications. Instead, a personalised approach based on nutritional screening (such as the BAPEN Malnutrition Universal Screening Tool), dietary assessment, and blood tests is more appropriate. If you're experiencing persistent vomiting, signs of dehydration, or inability to maintain adequate oral intake, seek prompt medical review. For ongoing nutritional concerns, your healthcare provider may consider referral to a registered dietitian.
Essential Vitamins and Minerals for GLP-1 Users
Vitamin B12 (cobalamin) is particularly important for GLP-1 users, especially those with type 2 diabetes who may also be taking metformin, which is known to impair B12 absorption. The MHRA has issued a Drug Safety Update recommending B12 monitoring in patients on long-term metformin treatment. This vitamin is essential for neurological function, red blood cell formation, and DNA synthesis. Deficiency can lead to fatigue, peripheral neuropathy, and megaloblastic anaemia. The recommended daily intake is 1.5 micrograms for adults. Food sources include meat, fish, dairy products, and fortified cereals. If blood tests confirm deficiency, your GP may prescribe appropriate treatment, which could include hydroxocobalamin injections or higher-dose oral supplements.
Vitamin D plays a crucial role in calcium absorption, bone health, immune function, and muscle strength—all particularly relevant during weight loss. Many UK residents have insufficient vitamin D levels, especially during autumn and winter months. The NHS recommends that adults consider taking 10 micrograms (400 IU) of vitamin D daily, particularly from October to March. Some groups may need year-round supplementation. Do not exceed 100 micrograms (4,000 IU) daily without medical supervision, as excessive intake can be harmful.
Calcium is vital for maintaining bone density during weight loss, when bone remodelling may be affected. Adults require 700 milligrams daily, ideally obtained through dietary sources such as dairy products, fortified plant milks, leafy greens, and tinned fish with bones. If dietary intake is inadequate, calcium supplements may be recommended, but should be taken separately from iron supplements for optimal absorption. Those with kidney stones or hypercalcaemia should seek medical advice before supplementing.
Iron deficiency can develop if meat consumption decreases significantly. Iron is essential for oxygen transport and energy metabolism. Women of reproductive age and those with heavy menstrual periods are at particular risk. The recommended intake is 8.7 mg daily for men and 14.8 mg for women. Supplementation should be guided by blood tests (serum ferritin, full blood count) as excessive iron can be harmful. Taking iron with vitamin C can improve absorption; avoid taking with calcium, tea, or coffee.
Thiamine (Vitamin B1) deserves special mention, particularly for patients experiencing persistent vomiting, which warrants urgent medical assessment. Adequate intake (1 mg daily for men, 0.8 mg for women) should be ensured through diet or supplementation if gastrointestinal symptoms are prolonged.
For women planning pregnancy or in early pregnancy: folic acid (400 micrograms daily) is essential to reduce the risk of neural tube defects. Avoid vitamin A supplements and liver products during pregnancy due to potential harm to the developing baby.
Other important nutrients include magnesium (supports muscle and nerve function, bone health; use with caution in renal impairment), folate (cell division), zinc (immune function, wound healing), and vitamin C (immune support, iron absorption). A comprehensive approach considers individual dietary patterns, pre-existing deficiencies, and concurrent medications.
How to Choose the Right Supplements on GLP-1 Therapy
Selecting appropriate vitamin supplementation whilst on GLP-1 therapy should be individualised and evidence-based, ideally guided by healthcare professionals. The first step is to consult your GP or prescribing clinician before starting any supplementation regimen. They can assess your specific risk factors, review your dietary intake, and arrange baseline blood tests to identify existing deficiencies. Common investigations include full blood count, vitamin B12, folate, vitamin D (25-hydroxyvitamin D), ferritin, and potentially calcium and magnesium levels.
For most GLP-1 users without identified deficiencies, a high-quality multivitamin and mineral supplement designed to provide approximately 100% of the recommended daily amounts may be appropriate. Look for products that meet UK regulatory standards with compliant labelling (including UK business details and batch/lot numbers). Both cyanocobalamin and methylcobalamin forms of B12 are acceptable; neither has proven superiority in UK clinical practice.
Timing and formulation matter for optimal absorption. Some patients find that taking supplements with a small meal helps reduce nausea, though this may be challenging given reduced appetite. Certain nutrients compete for absorption—for example, calcium and iron should be taken at different times of day (separated by approximately 2 hours). Chewable or liquid formulations may be better tolerated than large tablets, particularly if you experience difficulty swallowing or early satiety.
Be aware of supplement regulation and quality. In the UK, food supplements are regulated by the Food Standards Agency, though the standards differ from those for medicines. Choose products from reputable UK or EU manufacturers with compliant labelling and batch numbers. Be sceptical of supplements marketed specifically as "GLP-1 support" formulas with inflated prices. There is no official recommendation for proprietary supplement blends specifically for GLP-1 users.
Important safety considerations include: staying within safe upper limits (e.g., vitamin D 100 micrograms/day); maintaining consistent vitamin K intake if you take warfarin; and avoiding vitamin A (retinol) supplements during pregnancy. If you take medications, check for potential interactions with your pharmacist.
Monitor your response and maintain regular follow-up with your healthcare team. If you develop symptoms such as unusual fatigue, muscle weakness, numbness or tingling, hair loss, or mood changes, contact your GP as these may indicate nutritional deficiencies requiring investigation and targeted treatment. Report any suspected side effects from supplements or medications via the MHRA Yellow Card scheme (yellowcard.mhra.gov.uk). Remember that supplements are intended to complement, not replace, a balanced diet, so continue working towards consuming nutrient-dense foods within your reduced intake capacity.
Frequently Asked Questions
Do all patients on GLP-1 medications need to take vitamin supplements?
No, there is no official recommendation for routine supplementation for all GLP-1 users. Supplementation should be individualised based on dietary assessment, nutritional screening, and blood tests conducted by your healthcare provider to identify any specific deficiencies.
Which vitamin is most important to monitor if I'm taking both a GLP-1 medication and metformin?
Vitamin B12 is particularly important to monitor, as metformin is known to impair B12 absorption. The MHRA recommends B12 monitoring in patients on long-term metformin treatment, and your GP can arrange appropriate blood tests and prescribe treatment if deficiency is confirmed.
When should I seek medical attention for nutritional concerns whilst on GLP-1 therapy?
Seek prompt medical review if you experience persistent vomiting, signs of dehydration, inability to maintain adequate oral intake, or symptoms such as unusual fatigue, muscle weakness, numbness or tingling, which may indicate nutritional deficiencies requiring investigation.
The health-related content published on this site is based on credible scientific sources and is periodically reviewed to ensure accuracy and relevance. Although we aim to reflect the most current medical knowledge, the material is meant for general education and awareness only.
The information on this site is not a substitute for professional medical advice. For any health concerns, please speak with a qualified medical professional. By using this information, you acknowledge responsibility for any decisions made and understand we are not liable for any consequences that may result.
Heading 1
Heading 2
Heading 3
Heading 4
Heading 5
Heading 6
Lorem ipsum dolor sit amet, consectetur adipiscing elit, sed do eiusmod tempor incididunt ut labore et dolore magna aliqua. Ut enim ad minim veniam, quis nostrud exercitation ullamco laboris nisi ut aliquip ex ea commodo consequat. Duis aute irure dolor in reprehenderit in voluptate velit esse cillum dolore eu fugiat nulla pariatur.
Block quote
Ordered list
- Item 1
- Item 2
- Item 3
Unordered list
- Item A
- Item B
- Item C
Bold text
Emphasis
Superscript
Subscript












