Mounjaro (tirzepatide) is a once-weekly injectable medication licensed in the UK for type 2 diabetes management. As a dual GIP and GLP-1 receptor agonist, it significantly reduces appetite and slows gastric emptying, often leading to substantial weight loss. Whilst these effects support glycaemic control, they can inadvertently reduce overall food intake, making adequate protein consumption essential. Choosing the best protein for Mounjaro therapy helps preserve lean muscle mass, maintain metabolic health, and support immune function during weight loss. This article examines optimal protein sources, recommended intake levels, and practical strategies for meeting nutritional requirements whilst managing common side effects.
Summary: The best protein for Mounjaro includes lean sources such as chicken, white fish, Greek yoghurt, eggs, and plant-based options like lentils and tofu, which provide essential amino acids whilst being well-tolerated during appetite changes.
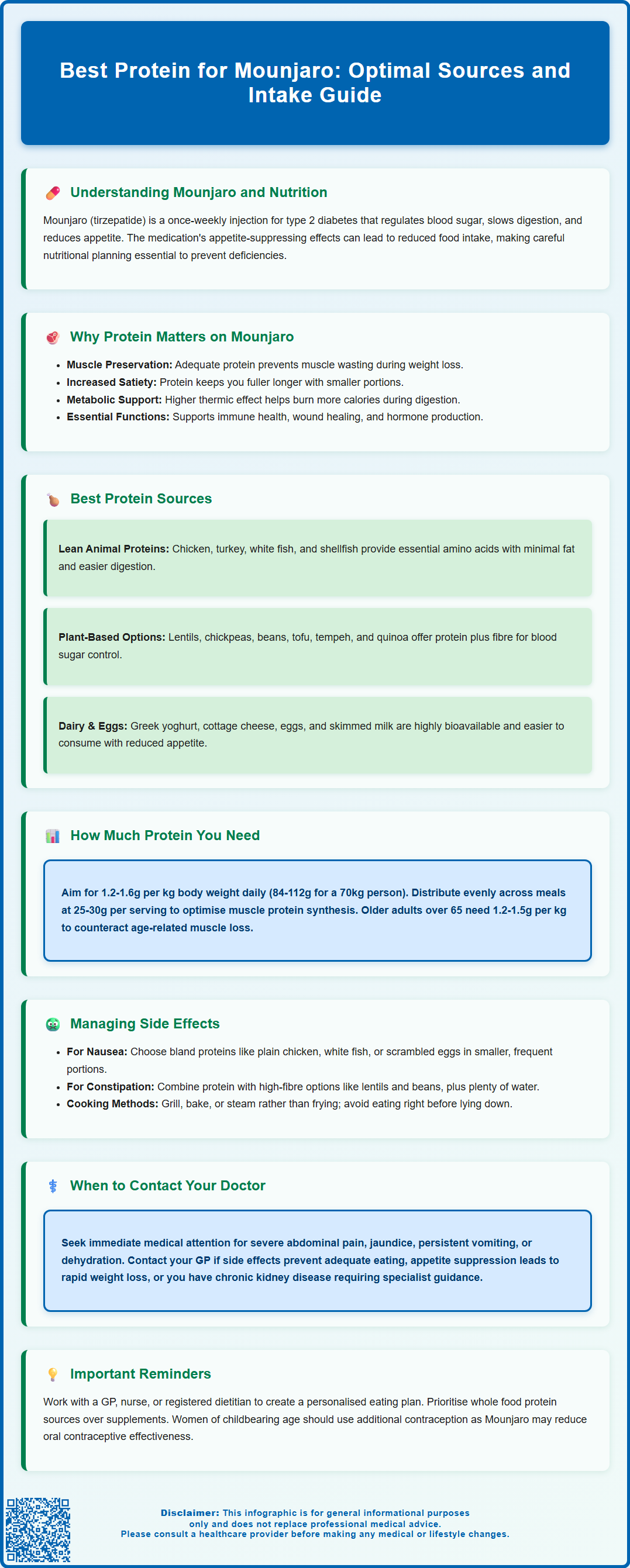
- Mounjaro (tirzepatide) is a dual GIP/GLP-1 receptor agonist licensed in the UK for type 2 diabetes, reducing appetite and slowing gastric emptying.
- Adequate protein intake (1.2–1.6g per kg adjusted body weight daily during weight loss) helps preserve lean muscle mass and metabolic function.
- Lean proteins (poultry, white fish, Greek yoghurt, eggs) and plant-based options (lentils, tofu, beans) are generally well-tolerated and nutritionally optimal.
- Common gastrointestinal side effects may be managed through smaller, frequent protein portions and bland, easily digestible sources.
- Patients should work with their GP or registered dietitian to establish personalised protein targets and monitor for adverse effects requiring medical review.
Table of Contents
Understanding Mounjaro and Nutritional Requirements
Mounjaro (tirzepatide) is a once-weekly injectable medication licensed in the UK for the treatment of type 2 diabetes mellitus. In the UK, tirzepatide is currently marketed as Mounjaro for diabetes management, while its use for weight management is subject to ongoing regulatory review. As a dual glucose-dependent insulinotropic polypeptide (GIP) and glucagon-like peptide-1 (GLP-1) receptor agonist, Mounjaro works by mimicking naturally occurring incretin hormones that regulate blood glucose levels and appetite. According to the MHRA-approved Summary of Product Characteristics (SmPC), the medication slows gastric emptying, enhances insulin secretion in response to meals, suppresses glucagon release, and reduces appetite through central nervous system pathways, leading to decreased food intake and subsequent weight loss.
When taking Mounjaro, patients often experience significant changes in appetite and eating patterns, with many reporting reduced hunger and earlier satiety. These effects, whilst therapeutically beneficial for glycaemic control and weight management, can inadvertently lead to reduced overall food intake and potential nutritional deficiencies if dietary choices are not carefully considered. Adequate protein intake becomes particularly important during treatment, as the body requires sufficient protein to preserve lean muscle mass during weight loss, support immune function, maintain tissue repair, and ensure optimal metabolic health.
The MHRA-approved prescribing information for Mounjaro does not mandate specific dietary modifications, but clinical evidence suggests that nutritional optimisation may enhance treatment outcomes. Importantly, patients should be aware that Mounjaro's effect on delaying gastric emptying may reduce the effectiveness of oral contraceptives, particularly during dose initiation and escalation; additional contraceptive methods may be needed during this period. Patients should work collaboratively with their GP, practice nurse, or a registered dietitian to develop an individualised eating plan that meets their protein requirements whilst accommodating the appetite changes associated with Mounjaro therapy. Understanding the relationship between medication effects and nutritional needs forms the foundation for successful long-term treatment outcomes.
Why Protein Intake Matters When Taking Mounjaro
Protein serves multiple critical functions that become especially important during Mounjaro treatment. When individuals lose weight, the body naturally loses both fat mass and lean muscle mass. Research consistently demonstrates that inadequate protein intake during energy restriction accelerates muscle loss, which can reduce metabolic rate, decrease functional capacity, and compromise long-term weight maintenance. Maintaining adequate protein consumption helps preserve muscle tissue, ensuring that weight loss predominantly reflects fat reduction rather than muscle wasting. This preservation of lean body mass is particularly important for older adults, who face greater risks of sarcopenia and functional decline.
Beyond muscle preservation, protein plays a vital role in satiety regulation. Evidence from systematic reviews suggests that high-protein foods typically promote greater feelings of fullness compared to carbohydrate or fat-rich alternatives, which can be advantageous when managing the appetite changes induced by Mounjaro. Adequate protein intake may help patients feel satisfied with smaller portions whilst ensuring nutritional adequacy. Protein also has a higher thermic effect than other macronutrients, meaning the body expends more energy digesting and metabolising protein, which may modestly support weight management efforts.
Furthermore, protein is essential for immune function, wound healing, hormone production, and enzyme synthesis. Patients taking Mounjaro who experience gastrointestinal side effects such as nausea or reduced appetite may inadvertently consume insufficient protein, potentially compromising these vital physiological processes. The amino acids derived from dietary protein cannot be stored in the body for extended periods, making regular, adequate intake necessary. If patients experience significant appetite suppression leading to inadequate food intake or unintended rapid weight loss, they should contact their healthcare provider promptly. Healthcare professionals should emphasise to patients that whilst Mounjaro effectively reduces appetite, meeting protein requirements remains a clinical priority throughout treatment to optimise health outcomes and maintain metabolic function during weight loss.
Best Protein Sources for Mounjaro Patients
Selecting appropriate protein sources whilst taking Mounjaro requires consideration of both nutritional quality and tolerability. In line with the NHS Eatwell Guide, lean protein sources are generally preferable, as they provide essential amino acids without excessive saturated fat or calories. Poultry such as chicken and turkey breast, white fish including cod, haddock, and plaice, and shellfish offer high-quality, easily digestible protein with minimal fat content. These options are often well-tolerated by patients experiencing gastrointestinal side effects, as they are less likely to exacerbate nausea compared to fatty meats.
Plant-based proteins represent excellent alternatives and can be particularly suitable for patients finding animal proteins difficult to tolerate. Legumes such as lentils, chickpeas, and beans provide protein alongside beneficial fibre, which supports digestive health and glycaemic control. Tofu, tempeh, and other soya-based products offer complete proteins containing all essential amino acids. Quinoa, though technically a seed, provides a complete protein profile and can be incorporated into various meals. These plant-based options may be gentler on the digestive system for some individuals whilst contributing to overall nutritional diversity. Patients following predominantly plant-based diets should ensure adequate vitamin B12 and iron intake, as recommended by the British Dietetic Association.
Dairy products, including Greek yoghurt, cottage cheese, and skimmed milk, provide high-quality protein with the added benefit of calcium and leucine, an amino acid particularly important for muscle protein synthesis. Greek yoghurt, in particular, offers a concentrated protein source that many patients find easy to consume even when appetite is reduced. Eggs remain one of the most bioavailable protein sources, containing all essential amino acids in optimal ratios. For patients struggling to meet protein requirements through whole foods alone, protein supplements such as whey or plant-based protein powders may be considered under healthcare professional guidance, though whole food sources should remain the primary approach. Patients with diabetes should check for added sugars in flavoured protein products. The key is identifying protein sources that align with individual tolerances, preferences, and any concurrent dietary requirements related to diabetes management or other health conditions.
How Much Protein Should You Eat on Mounjaro
Determining optimal protein intake for individuals taking Mounjaro requires consideration of several factors, including current body weight, weight loss goals, activity level, age, and any concurrent medical conditions. The UK Scientific Advisory Committee on Nutrition (SACN) sets the reference nutrient intake (RNI) for protein at 0.75 grams per kilogram of body weight daily for adults, which represents the minimum amount needed to prevent deficiency in the general population. However, this baseline recommendation may be insufficient for individuals undergoing active weight loss or taking medications like Mounjaro that significantly alter eating patterns.
Current evidence suggests that higher protein intakes may better support muscle preservation during energy restriction and weight loss. UK dietetic practice often recommends ranges of 1.2 to 1.6 grams per kilogram of adjusted body weight daily during weight loss (particularly in obesity). For a person with an adjusted body weight of 70 kilograms, this translates to approximately 84 to 112 grams of protein daily. Some clinical guidelines recommend distributing protein intake relatively evenly across meals, with approximately 25 to 30 grams per meal, as this pattern may optimally stimulate muscle protein synthesis. For older adults (over 65 years), protein requirements may be higher, potentially reaching 1.2 to 1.5 grams per kilogram of body weight, to counteract age-related muscle loss.
Patients should work with their healthcare team, ideally including a registered dietitian, to establish personalised protein targets based on their individual circumstances. Those with chronic kidney disease require careful protein management, as excessive intake may not be appropriate. The UK Kidney Association provides specific guidance, and patients with CKD stages 3-5 should receive specialist renal dietetic input. Practical strategies for meeting protein goals include planning meals around a protein source, incorporating protein-rich snacks such as nuts or yoghurt, and monitoring intake through food diaries or mobile applications. Regular review with a healthcare professional ensures that protein intake remains adequate as weight loss progresses and body composition changes. If patients struggle to consume adequate protein due to persistent nausea or early satiety, they should contact their GP or prescribing clinician to discuss potential dose adjustments or additional supportive measures.
Managing Side Effects Through Protein Selection
Gastrointestinal side effects represent the most commonly reported adverse reactions to Mounjaro, with nausea, vomiting, diarrhoea, constipation, and abdominal discomfort affecting a substantial proportion of patients, particularly during dose escalation. Strategic protein selection and preparation methods can help manage these symptoms whilst maintaining adequate nutritional intake. When experiencing nausea, patients often find that bland, easily digestible protein sources such as plain chicken breast, white fish, or scrambled eggs are better tolerated than rich, fatty, or heavily seasoned options. Consuming smaller, more frequent protein portions throughout the day, rather than large servings at single meals, can reduce the likelihood of triggering nausea or early satiety.
For patients experiencing constipation, combining protein sources with adequate fibre and hydration becomes important. Plant-based proteins such as lentils and beans naturally provide both protein and fibre, supporting regular bowel movements. Ensuring sufficient fluid intake alongside protein consumption helps prevent dehydration, which can exacerbate constipation and potentially lead to acute kidney injury in severe cases. Conversely, if diarrhoea occurs, patients may temporarily benefit from lower-fibre protein sources and should maintain hydration with appropriate fluids. Some individuals find that cold or room-temperature proteins, such as Greek yoghurt or cottage cheese, are more palatable than hot meals when experiencing nausea.
Protein preparation methods also influence tolerability. Grilled, baked, or steamed proteins are generally better tolerated than fried or heavily sauced options, which may worsen gastrointestinal symptoms. Patients should avoid consuming protein immediately before lying down, as this may exacerbate reflux symptoms that occasionally occur with Mounjaro. Patients should be aware of important safety considerations from the MHRA SmPC: severe, persistent abdominal pain (with or without vomiting) may indicate pancreatitis; jaundice or right upper quadrant pain may suggest gallbladder disease; and patients taking insulin or sulfonylureas alongside Mounjaro should monitor for hypoglycaemia. Women of childbearing potential should note that Mounjaro may reduce the effectiveness of oral contraceptives, particularly during dose initiation and escalation; additional contraceptive methods may be needed during this period. Mounjaro is not recommended during pregnancy or breastfeeding.
If side effects persist despite dietary modifications, or if patients cannot maintain adequate protein intake due to severe symptoms, they should contact their GP promptly. For severe symptoms such as persistent vomiting, severe abdominal pain, or signs of dehydration, patients should contact NHS 111 or seek urgent medical assessment. In an emergency, they should call 999. Healthcare professionals may consider temporary dose reduction, additional antiemetic medication, or referral to specialist services to ensure patients can continue treatment safely whilst meeting their nutritional requirements.
Frequently Asked Questions
How much protein should I eat whilst taking Mounjaro?
Current evidence suggests 1.2 to 1.6 grams per kilogram of adjusted body weight daily during weight loss, distributed across meals. Patients should work with their healthcare team to establish personalised targets based on individual circumstances, age, and any concurrent medical conditions.
What are the best protein sources if I experience nausea on Mounjaro?
Bland, easily digestible proteins such as plain chicken breast, white fish, scrambled eggs, Greek yoghurt, and cottage cheese are generally better tolerated. Consuming smaller, more frequent portions and choosing cold or room-temperature options may help manage nausea.
Can I use protein supplements whilst taking Mounjaro?
Protein supplements such as whey or plant-based powders may be considered under healthcare professional guidance if whole food sources are insufficient, though whole foods should remain the primary approach. Patients with diabetes should check for added sugars in flavoured products.
The health-related content published on this site is based on credible scientific sources and is periodically reviewed to ensure accuracy and relevance. Although we aim to reflect the most current medical knowledge, the material is meant for general education and awareness only.
The information on this site is not a substitute for professional medical advice. For any health concerns, please speak with a qualified medical professional. By using this information, you acknowledge responsibility for any decisions made and understand we are not liable for any consequences that may result.
Heading 1
Heading 2
Heading 3
Heading 4
Heading 5
Heading 6
Lorem ipsum dolor sit amet, consectetur adipiscing elit, sed do eiusmod tempor incididunt ut labore et dolore magna aliqua. Ut enim ad minim veniam, quis nostrud exercitation ullamco laboris nisi ut aliquip ex ea commodo consequat. Duis aute irure dolor in reprehenderit in voluptate velit esse cillum dolore eu fugiat nulla pariatur.
Block quote
Ordered list
- Item 1
- Item 2
- Item 3
Unordered list
- Item A
- Item B
- Item C
Bold text
Emphasis
Superscript
Subscript












