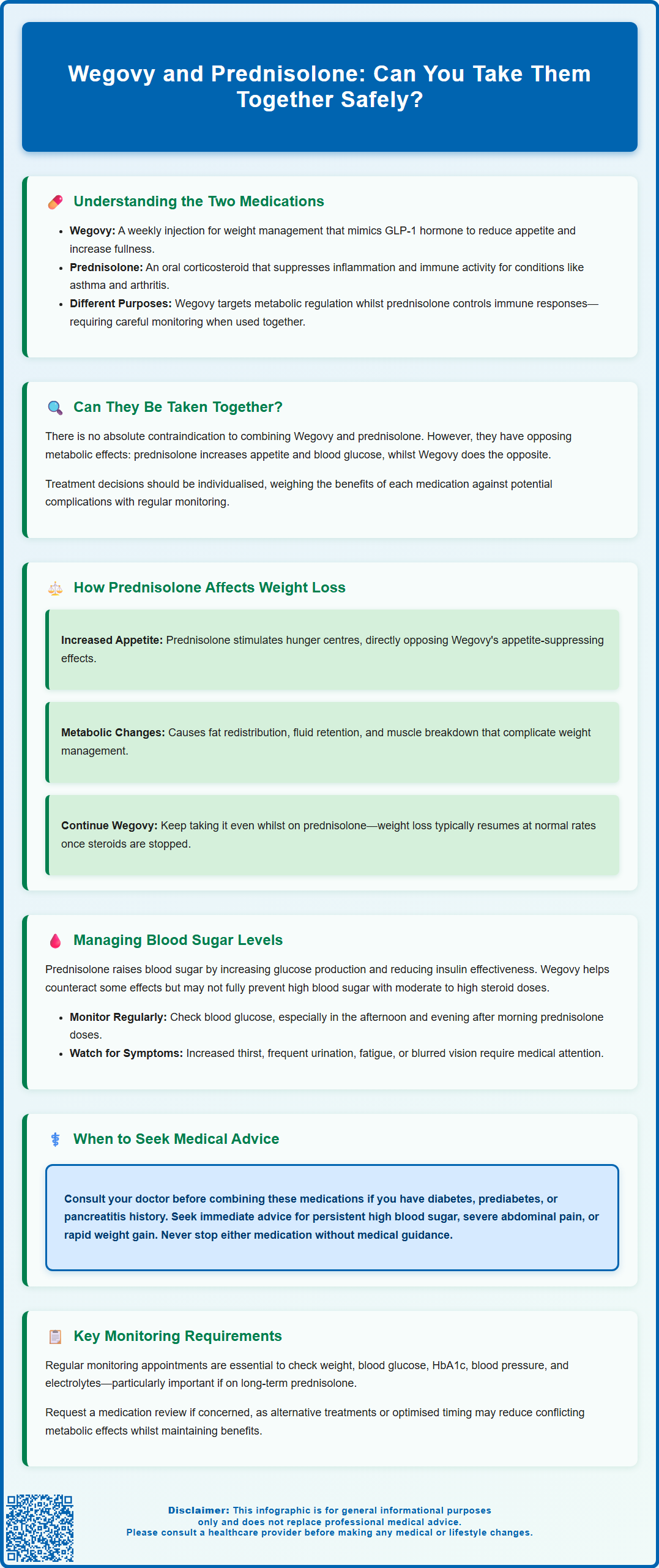
Wegovy (semaglutide) and prednisolone are two distinct medications that patients may need to take concurrently for different health conditions. Wegovy is a GLP-1 receptor agonist licensed for chronic weight management in adults with obesity or overweight with comorbidities, whilst prednisolone is a corticosteroid used to suppress inflammation and immune activity in conditions such as asthma, rheumatoid arthritis, and inflammatory bowel disease. Although there is no absolute contraindication to using both medications together, their opposing metabolic effects—particularly on appetite, weight, and blood glucose—require careful monitoring and individualised management. Understanding how these medications interact helps patients and clinicians optimise treatment outcomes whilst minimising potential complications.
Summary: Wegovy and prednisolone can be taken together as there is no absolute contraindication, but their opposing metabolic effects require careful monitoring and individualised management.
- Wegovy is a GLP-1 receptor agonist for weight management; prednisolone is a corticosteroid that suppresses inflammation and immune responses.
- Prednisolone increases appetite and may cause weight gain, potentially counteracting Wegovy's weight loss effects.
- Prednisolone elevates blood glucose whilst Wegovy improves glycaemic control, necessitating vigilant glucose monitoring.
- Patients with diabetes or prediabetes may require adjustments to glucose-lowering medications when using both drugs concurrently.
- Regular GP or specialist review is essential to monitor weight, blood glucose, HbA1c, and other metabolic parameters.
- Never stop either medication without medical guidance; abrupt prednisolone cessation can cause adrenal insufficiency.
Table of Contents
Understanding Wegovy and Prednisolone: Two Different Medications
Wegovy (semaglutide 2.4 mg) and prednisolone are two fundamentally different medications prescribed for distinct clinical purposes. Understanding how each works is essential when considering their combined use.
Wegovy is a glucagon-like peptide-1 (GLP-1) receptor agonist licensed by the MHRA for chronic weight management in adults with obesity (BMI ≥30 kg/m²) or overweight (BMI ≥27 kg/m²) with at least one weight-related comorbidity. It works by mimicking the natural hormone GLP-1, which regulates appetite and food intake. Semaglutide slows gastric emptying (most pronounced early in treatment), increases feelings of fullness, and reduces hunger signals in the brain. It is administered once weekly via subcutaneous injection. In the NHS, Wegovy is typically prescribed within specialist weight management services for up to 2 years, alongside lifestyle modifications including diet and exercise.
Prednisolone is the standard oral corticosteroid used in UK practice to suppress inflammation and immune system activity. It is prescribed for a wide range of conditions including asthma exacerbations, rheumatoid arthritis, inflammatory bowel disease, allergic reactions, and autoimmune disorders. Prednisolone works by mimicking cortisol, a natural hormone produced by the adrenal glands, and suppresses the production of inflammatory mediators. It can be prescribed for short courses (days to weeks) or as long-term maintenance therapy, depending on the underlying condition.
These medications have entirely different mechanisms of action and therapeutic targets. Wegovy addresses metabolic regulation and weight management, whilst prednisolone modulates immune and inflammatory responses. However, their differing effects on metabolism, appetite, and blood glucose mean that patients prescribed both medications require careful monitoring and individualised management plans.
Note: In the US, prednisone is commonly prescribed; this is converted to prednisolone in the liver. In the UK, prednisolone is typically prescribed directly.
Can You Take Wegovy and Prednisolone Together?
There is no absolute contraindication to taking Wegovy and prednisolone concurrently, and no direct pharmacological interaction between semaglutide and corticosteroids has been identified that would prevent their combined use. Patients may legitimately require both medications simultaneously—for example, someone with obesity and rheumatoid arthritis, or a patient with asthma requiring corticosteroid therapy who is also managing weight-related health conditions.
However, the combination does present clinical challenges that require careful consideration and monitoring. The primary concern is that prednisolone and Wegovy have opposing effects on several metabolic parameters. Whilst Wegovy promotes weight loss and improves glycaemic control, prednisolone tends to increase appetite, promote weight gain, and can elevate blood glucose levels. This creates a situation where the therapeutic benefits of one medication may be partially offset by the adverse effects of the other.
It's worth noting that Wegovy slows gastric emptying, which may slightly delay the absorption of oral medicines including prednisolone. While this is usually of minimal clinical significance, it's something to be aware of, particularly early in treatment.
Before starting or continuing both medications together, patients should have a thorough discussion with their GP or specialist. This conversation should cover:
-
The medical necessity of both treatments
-
The expected duration of prednisolone therapy (short-term versus long-term)
-
Individual risk factors, particularly regarding diabetes or prediabetes
-
Realistic expectations about weight loss outcomes whilst on corticosteroids
-
Monitoring requirements for blood glucose and other metabolic parameters
The decision to use both medications should be individualised, weighing the clinical benefits of each treatment against potential complications. In some cases, the underlying condition requiring prednisolone may take priority, whilst in others, alternative anti-inflammatory agents with less metabolic impact might be considered.
Importantly, Wegovy should not be used with other GLP-1 receptor agonists or other weight-loss medicines unless specifically advised by a specialist.
How Prednisolone May Affect Weight Loss on Wegovy
Prednisolone can significantly counteract the weight loss effects of Wegovy through several physiological mechanisms. Understanding these interactions helps set realistic expectations and guides management strategies.
Increased appetite and food intake represent the most direct challenge. Corticosteroids stimulate appetite centres in the hypothalamus, often causing marked increases in hunger and food-seeking behaviour. Patients frequently report intense cravings, particularly for carbohydrate-rich and high-calorie foods. This effect directly opposes Wegovy's appetite-suppressing action, potentially reducing the caloric deficit necessary for weight loss. Even with semaglutide's satiety signals, the powerful appetite stimulation from prednisolone may override these effects, especially at higher corticosteroid doses.
Metabolic changes induced by prednisolone further complicate weight management. Corticosteroids promote:
-
Fat redistribution, causing central (truncal) obesity and the characteristic "cushingoid" appearance with prolonged use
-
Fluid retention, leading to weight gain that may not reflect true fat accumulation but can be discouraging
-
Muscle protein breakdown, reducing lean body mass and potentially lowering metabolic rate
-
Insulin resistance, making weight loss more difficult
The magnitude of these effects is generally dose- and duration-dependent. Short courses of prednisolone typically have less impact on overall weight loss trajectory compared to longer-term therapy at higher doses. It's reassuring to know that steroid-related fluid retention and some metabolic effects often improve after dose reduction or cessation.
Patients should not discontinue Wegovy simply because they require prednisolone. The GLP-1 agonist may still provide benefits including improved glycaemic control and some degree of appetite regulation, even if weight loss is slower than expected. Once prednisolone is tapered or discontinued, weight loss typically resumes at a more predictable rate.
It's important to follow the licensed dose escalation for Wegovy regardless of prednisolone use, with a maximum dose of 2.4 mg weekly as per the MHRA product licence.
Managing Blood Sugar When Using Both Medications
The combination of Wegovy and prednisolone requires vigilant blood glucose monitoring, particularly in patients with diabetes, prediabetes, or risk factors for glucose intolerance. These medications have opposing effects on glycaemic control that necessitate proactive management.
Prednisolone-induced hyperglycaemia is a well-recognised adverse effect occurring through multiple mechanisms. Corticosteroids increase hepatic glucose production, reduce peripheral glucose uptake in muscle and adipose tissue, and impair insulin secretion from pancreatic beta cells. The resulting insulin resistance can elevate blood glucose levels significantly, sometimes precipitating steroid-induced diabetes in previously normoglycaemic individuals. The hyperglycaemic effect is dose-dependent and typically most pronounced in the afternoon and evening, several hours after morning prednisolone administration.
Wegovy provides some protective effect against corticosteroid-induced hyperglycaemia. Semaglutide enhances glucose-dependent insulin secretion, suppresses inappropriate glucagon release, and slows gastric emptying, all of which help moderate blood glucose excursions. However, Wegovy alone may not fully counteract the hyperglycaemic effects of moderate to high-dose corticosteroids. Importantly, semaglutide rarely causes hypoglycaemia unless used with insulin or sulfonylureas—doses of these medications may need review.
Monitoring recommendations for patients using both medications include:
-
Regular blood glucose testing—particularly post-lunch and early evening when morning prednisolone is used
-
Consider action if readings are persistently above 12 mmol/L (with individualisation based on your care plan)
-
HbA1c measurement every 3 months for patients with diabetes or prediabetes
-
Fasting glucose checks if not previously diabetic, particularly during corticosteroid therapy
-
Symptom awareness for hyperglycaemia (increased thirst, frequent urination, fatigue, blurred vision)
Patients with established diabetes may require adjustments to their glucose-lowering regimen whilst on prednisolone. This might include increased doses of existing medications, addition of new agents, or temporary insulin therapy. These decisions should be made in consultation with your GP or diabetes team. NICE guidance emphasises individualised glycaemic targets, particularly when multiple medications affecting glucose metabolism are used concurrently.
If you develop new symptoms suggestive of hyperglycaemia or your home glucose readings consistently exceed your target range, contact your GP or diabetes team promptly. For severe hyperglycaemia with dehydration or other concerning symptoms, seek same-day urgent care, call NHS 111, or go to A&E.
When to Seek Medical Advice About This Combination
Certain situations require prompt medical review when taking Wegovy and prednisolone together. Being aware of warning signs ensures timely intervention and prevents complications.
Before starting the combination, consult your GP or specialist if:
-
You have diabetes or prediabetes—your glucose-lowering regimen may need adjustment
-
You have a history of pancreatitis—semaglutide carries warnings about pancreatitis risk
-
You experience severe gastrointestinal symptoms on Wegovy—corticosteroids can affect the GI tract
-
You are taking multiple medications—comprehensive review prevents overlooked interactions
During concurrent therapy, seek medical advice if you experience:
-
Persistent hyperglycaemia—blood glucose consistently above target despite medication adherence
-
Symptoms of diabetes—excessive thirst, frequent urination, unexplained fatigue, or blurred vision
-
Severe gastrointestinal symptoms—persistent nausea, vomiting, or abdominal pain, which could indicate pancreatitis or other complications (seek urgent same-day assessment or go to A&E for severe, persistent abdominal pain with vomiting; stop semaglutide if pancreatitis is suspected)
-
Signs of infection—prednisolone suppresses immune function, warranting vigilance
-
Mood changes or depression—both medications can affect mental health in susceptible individuals
-
Unexplained weight gain—particularly rapid gain suggesting fluid retention or inadequate disease control
Regular follow-up appointments are essential when using this combination. Your GP should monitor:
-
Weight trends and body composition changes
-
Blood glucose and HbA1c levels
-
Blood pressure (both medications can influence cardiovascular parameters)
-
Electrolyte balance (prednisolone can cause hypokalaemia)
-
Bone health if long-term corticosteroid use is anticipated (following NOGG guidance for glucocorticoid-induced osteoporosis risk assessment and prophylaxis)
Never stop either medication without medical guidance. Abrupt prednisolone cessation after prolonged use can cause adrenal insufficiency, a potentially serious condition. Similarly, discontinuing Wegovy should be discussed with your prescriber, particularly if it forms part of your diabetes management strategy.
If you have concerns about the necessity of taking both medications, request a medication review with your GP or specialist. In some cases, alternative treatments with fewer metabolic effects might be appropriate, or the timing of therapies could be optimised to minimise conflicting effects whilst maintaining therapeutic benefit.
If you experience any suspected side effects from either medication, report them through the MHRA Yellow Card scheme.
Frequently Asked Questions
Will prednisolone stop Wegovy from working for weight loss?
Prednisolone may reduce Wegovy's weight loss effectiveness by increasing appetite, promoting fluid retention, and causing metabolic changes, but Wegovy can still provide benefits including improved blood glucose control. Weight loss typically resumes at a more predictable rate once prednisolone is tapered or discontinued.
Do I need to check my blood sugar more often when taking Wegovy and prednisolone together?
Yes, regular blood glucose monitoring is essential as prednisolone raises blood sugar whilst Wegovy lowers it. Check particularly in the afternoon and evening if taking morning prednisolone, and contact your GP if readings consistently exceed your target range or if you develop symptoms of hyperglycaemia.
Should I stop Wegovy if I need a short course of prednisolone?
No, you should not stop Wegovy for a short course of prednisolone unless specifically advised by your GP or specialist. Wegovy may still provide metabolic benefits and appetite regulation even during corticosteroid therapy, and weight loss typically improves once the prednisolone course is completed.
The health-related content published on this site is based on credible scientific sources and is periodically reviewed to ensure accuracy and relevance. Although we aim to reflect the most current medical knowledge, the material is meant for general education and awareness only.
The information on this site is not a substitute for professional medical advice. For any health concerns, please speak with a qualified medical professional. By using this information, you acknowledge responsibility for any decisions made and understand we are not liable for any consequences that may result.
Heading 1
Heading 2
Heading 3
Heading 4
Heading 5
Heading 6
Lorem ipsum dolor sit amet, consectetur adipiscing elit, sed do eiusmod tempor incididunt ut labore et dolore magna aliqua. Ut enim ad minim veniam, quis nostrud exercitation ullamco laboris nisi ut aliquip ex ea commodo consequat. Duis aute irure dolor in reprehenderit in voluptate velit esse cillum dolore eu fugiat nulla pariatur.
Block quote
Ordered list
- Item 1
- Item 2
- Item 3
Unordered list
- Item A
- Item B
- Item C
Bold text
Emphasis
Superscript
Subscript