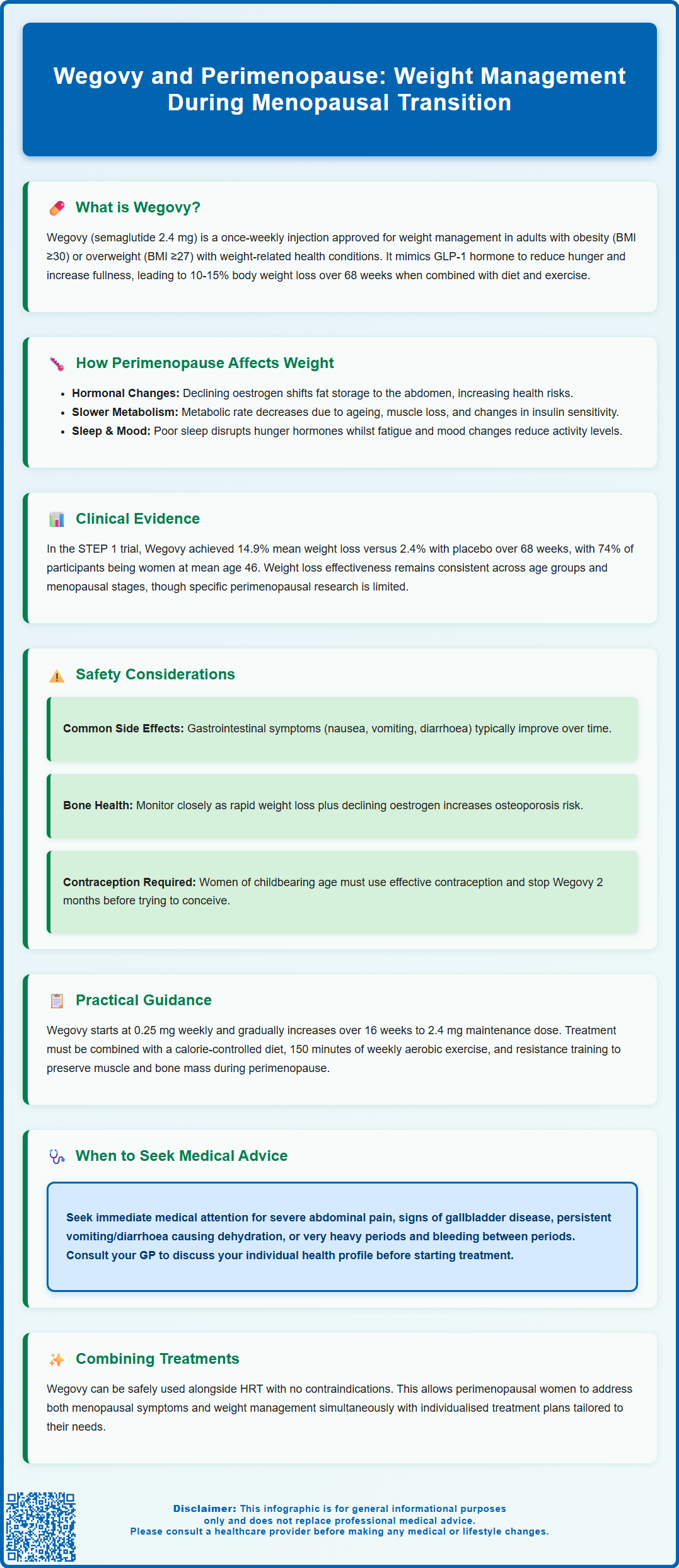
Wegovy and perimenopause represent an important intersection in women's health, as many women experience challenging weight gain during the menopausal transition. Wegovy (semaglutide 2.4 mg) is a once-weekly GLP-1 receptor agonist licensed by the MHRA for chronic weight management in adults with obesity or overweight with comorbidities. During perimenopause, hormonal fluctuations, metabolic changes, and symptoms such as sleep disturbance can make weight control increasingly difficult. This article examines the evidence for Wegovy use in perimenopausal women, safety considerations, and practical guidance for those considering this treatment alongside lifestyle interventions within UK specialist weight management services.
Summary: Wegovy (semaglutide 2.4 mg) is a GLP-1 receptor agonist that can support weight management in perimenopausal women who meet eligibility criteria, though it is not specifically licensed for perimenopausal symptoms.
- Wegovy is a once-weekly subcutaneous injection that reduces appetite by mimicking GLP-1 hormone action in the brain.
- Licensed for adults with BMI ≥30 kg/m² or ≥27 kg/m² with weight-related comorbidities, used alongside lifestyle interventions.
- Common side effects include gastrointestinal symptoms (nausea, vomiting, diarrhoea) that typically diminish during dose escalation.
- Contraindicated in pregnancy; women should discontinue at least 2 months before planned conception and use effective contraception.
- NICE TA875 recommends use within specialist weight management services after optimising dietary, physical activity, and behavioural interventions.
- Regular monitoring for pancreatitis, gallbladder disease, and bone health is important, particularly during the perimenopausal transition.
Table of Contents
- Understanding Wegovy and Its Role in Weight Management During Perimenopause
- How Perimenopause Affects Weight and Metabolism
- Clinical Evidence for Wegovy Use in Perimenopausal Women
- Safety Considerations and Contraindications for Wegovy in Perimenopause
- Practical Guidance: Using Wegovy During the Perimenopausal Transition
- Frequently Asked Questions
Understanding Wegovy and Its Role in Weight Management During Perimenopause
Wegovy (semaglutide 2.4 mg) is a glucagon-like peptide-1 (GLP-1) receptor agonist licensed by the MHRA for chronic weight management in adults with obesity (BMI ≥30 kg/m²) or overweight (BMI ≥27 kg/m²) with at least one weight-related comorbidity. Administered as a once-weekly subcutaneous injection, Wegovy works by mimicking the action of the naturally occurring hormone GLP-1, which regulates appetite and food intake.
The mechanism of action involves binding to GLP-1 receptors in the brain, particularly in areas that control appetite and satiety. This leads to reduced hunger, increased feelings of fullness, and delayed gastric emptying, collectively resulting in decreased caloric intake. Clinical trials have demonstrated that semaglutide can produce substantial weight loss—typically 10–15% of initial body weight over 68 weeks—when combined with lifestyle interventions including dietary modification and increased physical activity.
For women experiencing perimenopause—the transitional phase leading to menopause characterised by hormonal fluctuations and eventual cessation of menstruation—weight management often becomes increasingly challenging. Many perimenopausal women report difficulty losing weight despite maintaining previous dietary and exercise habits. Wegovy may offer a pharmacological option for those struggling with weight gain during this life stage, particularly when lifestyle measures alone prove insufficient.
It is important to note that Wegovy is not specifically licensed for perimenopausal symptoms but rather for weight management in eligible individuals. NICE technology appraisal (TA875) recommends semaglutide for managing overweight and obesity within specialist weight management services, after dietary, physical activity, and behavioural interventions have been optimised. Women considering Wegovy during perimenopause should discuss their individual circumstances, including menopausal status and overall health profile, with their GP or specialist.
How Perimenopause Affects Weight and Metabolism
Perimenopause typically begins in a woman's 40s, though it can start earlier, and lasts an average of four years before menopause (defined as 12 consecutive months without menstruation). During this transition, fluctuating levels of oestrogen and progesterone create physiological changes that can impact body composition, metabolism, and weight distribution.
Hormonal changes during perimenopause may contribute to metabolic alterations, though weight gain is multifactorial and not solely attributable to hormonal shifts. Declining oestrogen levels, alongside ageing and lifestyle factors, are associated with changes in fat distribution from peripheral (hips and thighs) to central (abdominal) adiposity. This visceral fat accumulation is linked to increased cardiovascular and metabolic risks, including higher likelihood of developing type 2 diabetes, hypertension, and dyslipidaemia. Many women experience gradual weight gain during the perimenopausal transition, with changes in body composition even when weight remains stable.
Metabolic rate naturally declines with age, and this, combined with perimenopausal changes, can affect weight management. Changes in insulin sensitivity may occur, potentially making weight control more challenging. Additionally, loss of muscle mass (sarcopenia), which occurs with ageing, decreases basal metabolic rate since muscle tissue burns more calories at rest than adipose tissue.
Other perimenopausal symptoms—including sleep disturbances, mood changes, fatigue, and hot flushes—can indirectly contribute to weight gain. Poor sleep quality disrupts appetite-regulating hormones (ghrelin and leptin), potentially increasing hunger and cravings. Fatigue and mood disturbances may reduce motivation for physical activity and lead to emotional eating patterns. These interconnected factors create a challenging environment for weight management, making pharmacological interventions like Wegovy potentially valuable for appropriately selected perimenopausal women struggling with obesity or overweight with comorbidities.
Important note: If you experience very heavy periods, bleeding between periods, or any bleeding after menopause, seek prompt medical advice as these require assessment by your GP.
Clinical Evidence for Wegovy Use in Perimenopausal Women
The pivotal clinical trials for semaglutide 2.4 mg (Wegovy) included participants across various age groups, including perimenopausal and postmenopausal women, though subgroup analyses specifically examining perimenopausal women are limited in published literature. The STEP (Semaglutide Treatment Effect in People with obesity) programme comprised several large randomised controlled trials demonstrating consistent weight loss efficacy across diverse populations.
In the STEP 1 trial (Wilding et al., NEJM 2021), which included adults with obesity or overweight with weight-related comorbidities, participants receiving semaglutide 2.4 mg achieved a mean weight loss of 14.9% compared to 2.4% with placebo over 68 weeks. The majority of participants (74.1%) were women, with a mean age of 46 years, suggesting substantial representation of perimenopausal individuals. Subgroup analyses by age and sex showed consistent efficacy across demographic categories, though specific menopausal status was not routinely reported.
The STEP 2 trial (Davies et al., Lancet 2021) specifically enrolled participants with type 2 diabetes, a condition more prevalent during perimenopause due to metabolic changes. Results demonstrated mean weight loss of 9.6% with semaglutide 2.4 mg versus 3.4% with placebo, alongside improvements in glycaemic control. For perimenopausal women with concurrent type 2 diabetes, this dual benefit may be particularly relevant.
While some post-hoc analyses of GLP-1 receptor agonist studies suggest comparable weight loss outcomes between premenopausal and postmenopausal women, specific data for perimenopausal women are limited. Individual responses vary, and there is currently insufficient evidence to suggest that perimenopausal status significantly alters the effectiveness of Wegovy.
It is important to emphasise that clinical decisions should be individualised. Women considering Wegovy during perimenopause should be assessed according to standard eligibility criteria (BMI thresholds and comorbidities) rather than menopausal status alone. In the UK, NICE TA875 provides guidance on semaglutide use within specialist weight management services. Ongoing research may provide more specific guidance for this population in future.
Safety Considerations and Contraindications for Wegovy in Perimenopause
Wegovy is generally well-tolerated, but like all medications, it carries potential adverse effects and specific considerations that require careful assessment, particularly in perimenopausal women who may have additional health concerns.
Common adverse effects include:
-
Gastrointestinal symptoms: Nausea, vomiting, diarrhoea, constipation, and abdominal pain are the most frequently reported side effects, typically occurring during dose escalation. These effects are usually mild to moderate and diminish over time. Starting with a low dose and gradually titrating upwards helps minimise gastrointestinal intolerance.
-
Injection site reactions: Mild reactions such as redness, itching, or discomfort at the injection site may occur but are generally transient.
Serious but rare adverse effects require awareness:
-
Pancreatitis: Acute pancreatitis has been reported with GLP-1 receptor agonists. Patients should seek immediate medical attention if they experience severe, persistent abdominal pain radiating to the back. If pancreatitis is confirmed, Wegovy should be permanently discontinued.
-
Gallbladder disease: Rapid weight loss increases the risk of cholelithiasis (gallstones). Perimenopausal women may already have elevated risk due to hormonal factors.
-
Hypoglycaemia: Risk is low with Wegovy monotherapy but increases when used alongside insulin or sulfonylureas, relevant for women with type 2 diabetes.
-
Dehydration and kidney injury: Severe gastrointestinal side effects may lead to dehydration and acute kidney injury. Patients should maintain adequate fluid intake, especially if experiencing vomiting or diarrhoea.
-
Diabetic retinopathy: In people with type 2 diabetes, rapid improvement in glucose control may temporarily worsen diabetic retinopathy. Regular eye examinations are recommended.
-
Heart rate increase: Small increases in heart rate have been observed with semaglutide.
Specific considerations for perimenopausal women:
-
Bone health: Rapid weight loss may affect bone density, a particular concern during perimenopause when oestrogen decline already increases osteoporosis risk. Adequate calcium and vitamin D intake should be ensured.
-
Cardiovascular assessment: Perimenopausal women have increasing cardiovascular risk. Wegovy has demonstrated cardiovascular benefits in clinical trials, but baseline cardiovascular assessment is prudent.
-
Medication interactions: Review of concurrent medications is essential. For women taking warfarin or other coumarins, INR monitoring is advised when initiating Wegovy. Delayed gastric emptying may affect absorption of some oral medicines, though oral contraceptives are not clinically affected.
According to the UK SmPC, Wegovy is contraindicated in patients with hypersensitivity to semaglutide or any excipients. It should not be used during pregnancy or breastfeeding, and women of childbearing potential should use effective contraception. Women planning pregnancy should discontinue Wegovy at least 2 months before conception. The SmPC includes a precaution regarding thyroid C-cell tumours based on animal studies, though human relevance remains uncertain.
Suspected adverse reactions should be reported via the MHRA Yellow Card Scheme (yellowcard.mhra.gov.uk or the Yellow Card app).
Practical Guidance: Using Wegovy During the Perimenopausal Transition
Initiating Wegovy during perimenopause requires a comprehensive, individualised approach that addresses both weight management goals and the broader context of menopausal transition.
Pre-treatment assessment should include:
-
BMI calculation and confirmation of eligibility criteria (BMI ≥30 kg/m² or ≥27 kg/m² with weight-related comorbidities such as type 2 diabetes, hypertension, or dyslipidaemia)
-
Medical history review, including thyroid disease, pancreatitis, gallbladder disease, and cardiovascular risk factors
-
Current medications, particularly antidiabetic agents that may require dose adjustment
-
Pregnancy status and contraception counselling where relevant (Wegovy should not be used during pregnancy and should be discontinued at least 2 months before planned conception)
-
Baseline investigations: HbA1c (if diabetic or at risk), lipid profile, liver function tests, and thyroid function tests as clinically indicated
-
Discussion of realistic expectations: Wegovy is most effective when combined with lifestyle modifications, not as monotherapy
Dosing schedule follows a gradual escalation protocol to minimise gastrointestinal side effects:
-
Weeks 1–4: 0.25 mg once weekly
-
Weeks 5–8: 0.5 mg once weekly
-
Weeks 9–12: 1 mg once weekly
-
Weeks 13–16: 1.7 mg once weekly
-
Week 17 onwards: 2.4 mg once weekly (maintenance dose)
If patients experience intolerable side effects, the dose escalation may be delayed. Some patients may remain on 1.7 mg if 2.4 mg is not tolerated.
Injection technique:
-
Rotate injection sites (abdomen, thigh, or upper arm)
-
Inject subcutaneously (under the skin, not into muscle)
-
Follow the pen instructions carefully
Missed doses: If a dose is missed and the next scheduled dose is more than 2 days away (>48 hours), take the missed dose as soon as possible. If less than 2 days until the next scheduled dose, skip the missed dose and take the next dose on the regular day.
Lifestyle integration remains fundamental:
-
Dietary modification: A balanced, calorie-controlled diet rich in whole foods, with adequate protein to preserve muscle mass during weight loss
-
Physical activity: Combination of aerobic exercise (150 minutes moderate intensity weekly) and resistance training to maintain muscle mass and bone density—particularly important during perimenopause
-
Behavioural support: Addressing emotional eating, stress management, and sleep hygiene
Monitoring and follow-up:
-
Review at 3–6 months to assess weight loss, tolerability, and comorbidity improvement
-
Consider discontinuation if weight loss is less than 5% after 6 months on the maintenance dose
-
Regular review of cardiovascular risk factors, bone health, and perimenopausal symptoms
When to contact your GP:
-
Severe, persistent abdominal pain (possible pancreatitis)
-
Signs of gallbladder disease (right upper quadrant pain, jaundice)
-
Symptoms of hypoglycaemia if taking concurrent antidiabetic medications
-
Persistent vomiting or diarrhoea leading to dehydration
-
Any concerns about side effects or treatment efficacy
Integration with HRT: There is no contraindication to using Wegovy alongside hormone replacement therapy. Many perimenopausal women may benefit from both treatments—HRT for vasomotor and other menopausal symptoms, and Wegovy for weight management. Decisions should be individualised based on each woman's symptom profile, risk factors, and treatment goals, with regular review to optimise both therapies.
In the UK, Wegovy is available through specialist weight management services according to NICE TA875 criteria.
Frequently Asked Questions
Can I use Wegovy during perimenopause?
Yes, Wegovy can be used during perimenopause if you meet eligibility criteria (BMI ≥30 kg/m² or ≥27 kg/m² with weight-related comorbidities). It should be prescribed through specialist weight management services alongside lifestyle interventions, following NICE guidance.
Does perimenopause affect how well Wegovy works?
Current evidence suggests Wegovy is effective across age groups and menopausal stages, though specific data for perimenopausal women are limited. Individual responses vary, and treatment decisions should be based on standard eligibility criteria rather than menopausal status alone.
Can I take Wegovy with hormone replacement therapy (HRT)?
Yes, there is no contraindication to using Wegovy alongside HRT. Many perimenopausal women may benefit from both treatments—HRT for menopausal symptoms and Wegovy for weight management—with individualised assessment and regular review by your GP or specialist.
The health-related content published on this site is based on credible scientific sources and is periodically reviewed to ensure accuracy and relevance. Although we aim to reflect the most current medical knowledge, the material is meant for general education and awareness only.
The information on this site is not a substitute for professional medical advice. For any health concerns, please speak with a qualified medical professional. By using this information, you acknowledge responsibility for any decisions made and understand we are not liable for any consequences that may result.
Heading 1
Heading 2
Heading 3
Heading 4
Heading 5
Heading 6
Lorem ipsum dolor sit amet, consectetur adipiscing elit, sed do eiusmod tempor incididunt ut labore et dolore magna aliqua. Ut enim ad minim veniam, quis nostrud exercitation ullamco laboris nisi ut aliquip ex ea commodo consequat. Duis aute irure dolor in reprehenderit in voluptate velit esse cillum dolore eu fugiat nulla pariatur.
Block quote
Ordered list
- Item 1
- Item 2
- Item 3
Unordered list
- Item A
- Item B
- Item C
Bold text
Emphasis
Superscript
Subscript